Abstract
Rev Bras Ter Intensiva. 2016;28(3):285-293
DOI 10.5935/0103-507X.20160043
To evaluate the knowledge and acceptance of the public and professionals working in intensive care units regarding organ donation after cardiac death.
The three hospitals with the most brain death notifications in Curitiba were selected, and two groups of respondents were established for application of the same questionnaire: the general public (i.e., visitors of patients in intensive care units) and health professionals working in the same intensive care unit. The questionnaire contained questions concerning demographics, intention to donate organs and knowledge of current legislation regarding brain death and donation after cardiac death.
In total, 543 questionnaires were collected, including 442 from family members and 101 from health professionals. There was a predominance of women and Catholics in both groups. More females intended to donate. Health professionals performed better in the knowledge comparison. The intention to donate organs was significantly higher in the health professionals group (p = 0.01). There was no significant difference in the intention to donate in terms of education level or income. There was a greater acceptance of donation after uncontrolled cardiac death among Catholics than among evangelicals (p < 0.001).
Most of the general population intended to donate, with greater intentions expressed by females. Education and income did not affect the decision. The type of transplant that used a donation after uncontrolled cardiac death was not well accepted in the study population, indicating the need for more clarification for its use in our setting.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):294-300
DOI 10.5935/0103-507X.20160042
To estimate the incidence of limitations to Advanced Life Support in critically ill patients admitted to an intensive care unit with integrated palliative care.
This retrospective cohort study included patients in the palliative care program of the intensive care unit of Hospital Paulistano over 18 years of age from May 1, 2011, to January 31, 2014. The limitations to Advanced Life Support that were analyzed included do-not-resuscitate orders, mechanical ventilation, dialysis and vasoactive drugs. Central tendency measures were calculated for quantitative variables. The chi-squared test was used to compare the characteristics of patients with or without limits to Advanced Life Support, and the Wilcoxon test was used to compare length of stay after Advanced Life Support. Confidence intervals reflecting p ≤ 0.05 were considered for statistical significance.
A total of 3,487 patients were admitted to the intensive care unit, of whom 342 were included in the palliative care program. It was observed that after entering the palliative care program, it took a median of 2 (1 - 4) days for death to occur in the intensive care unit and 4 (2 - 11) days for hospital death to occur. Many of the limitations to Advanced Life Support (42.7%) took place on the first day of hospitalization. Cardiopulmonary resuscitation (96.8%) and ventilatory support (73.6%) were the most adopted limitations.
The contribution of palliative care integrated into the intensive care unit was important for the practice of orthothanasia, i.e., the non-extension of the life of a critically ill patient by artificial means.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):310-314
DOI 10.5935/0103-507X.20160041
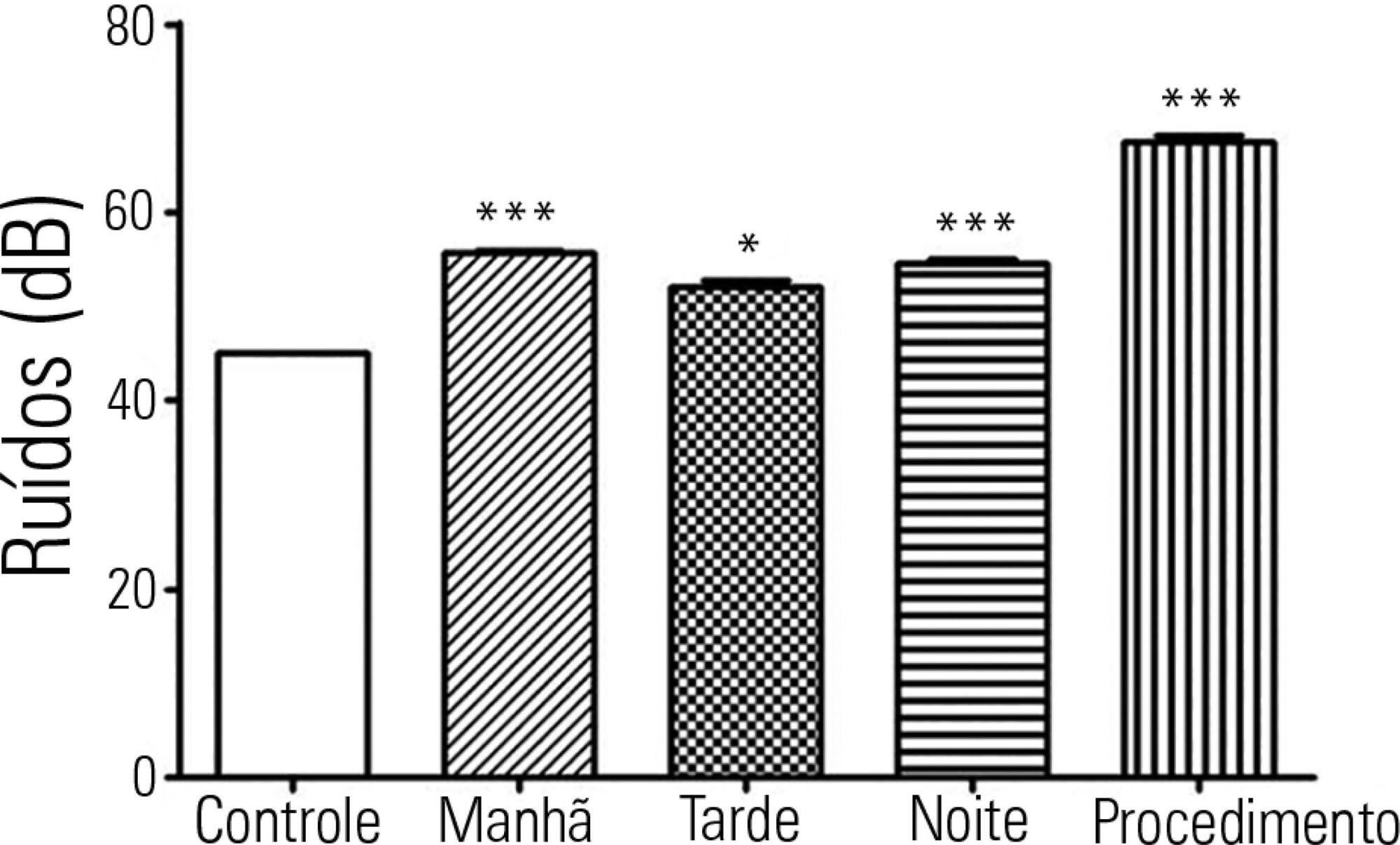
To investigate possible stressors to which newborns are exposed in the neonatal intensive care unit.
The levels of continuous noise were checked by a decibel meter positioned near the ear of the newborn, brightness was observed by a light meter positioned in the incubator in front of the newborn's eyes, and temperature was checked through the incubator display. The evaluations were performed in three periods of the day, with ten measurements taken at one-minute intervals during each shift for the subsequent statistical analysis.
All shifts showed noise above acceptable levels. Morning (p < 0.001), afternoon (p < 0.05) and night (p < 0.001) showed a significant increase compared to the control. The brightness significantly exceeded the normal range (p < 0.01) in the morning. We observed that only one of the incubators was within the normal temperature limits.
The noise, brightness and temperature intensities were not in accordance with regulatory standards and thus might be possible stressors to newborns.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):315-322
DOI 10.5935/0103-507X.20160044
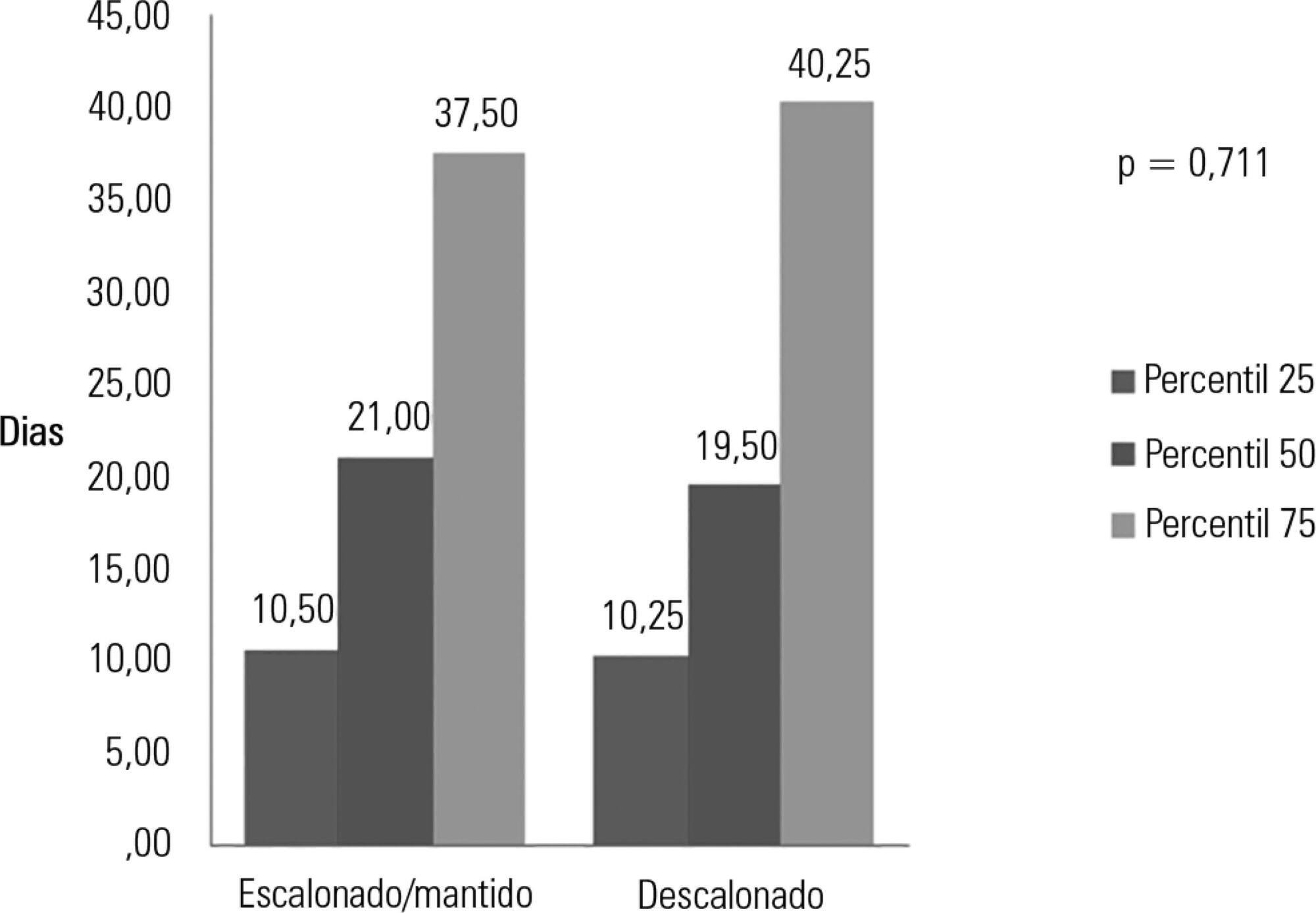
To evaluate the prevalence of antibiotic de-escalation in patients diagnosed with severe sepsis or septic shock at a public academic tertiary hospital and to evaluate antibiotic adequacy and culture positivity.
The prevalence of antibiotic de-escalation, the adequacy of antibiotic treatment and the rates of culture positivity were analyzed in patients with severe sepsis and septic shock between April and December 2013 at an intensive care unit in a tertiary university hospital.
Among the 224 patients included in the study, de-escalation was appropriate in 66 patients (29.4%) but was implemented in 44 patients (19.6%). Among the patients who underwent de-escalation, half experienced narrowing of the antimicrobial spectrum. The mortality rate was 56.3%, with no differences between the patients with or without de-escalation (56.8% versus 56.1%; p = 0.999) nor in the length of hospital stay. Empirical antibiotic therapy was appropriate in 89% of cases. Microorganisms were isolated from total cultures in 30% of cases and from blood cultures in 26.3% of cases.
The adequacy rate of empirical antibiotic therapy was high, reflecting an active institutional policy of monitoring epidemiological profiles and institutional protocols on antimicrobial use. However, antibiotic de-escalation could have been implemented in a greater number of patients. De-escalation did not affect mortality rates.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):49-54
DOI 10.5935/0103-507X.20160013
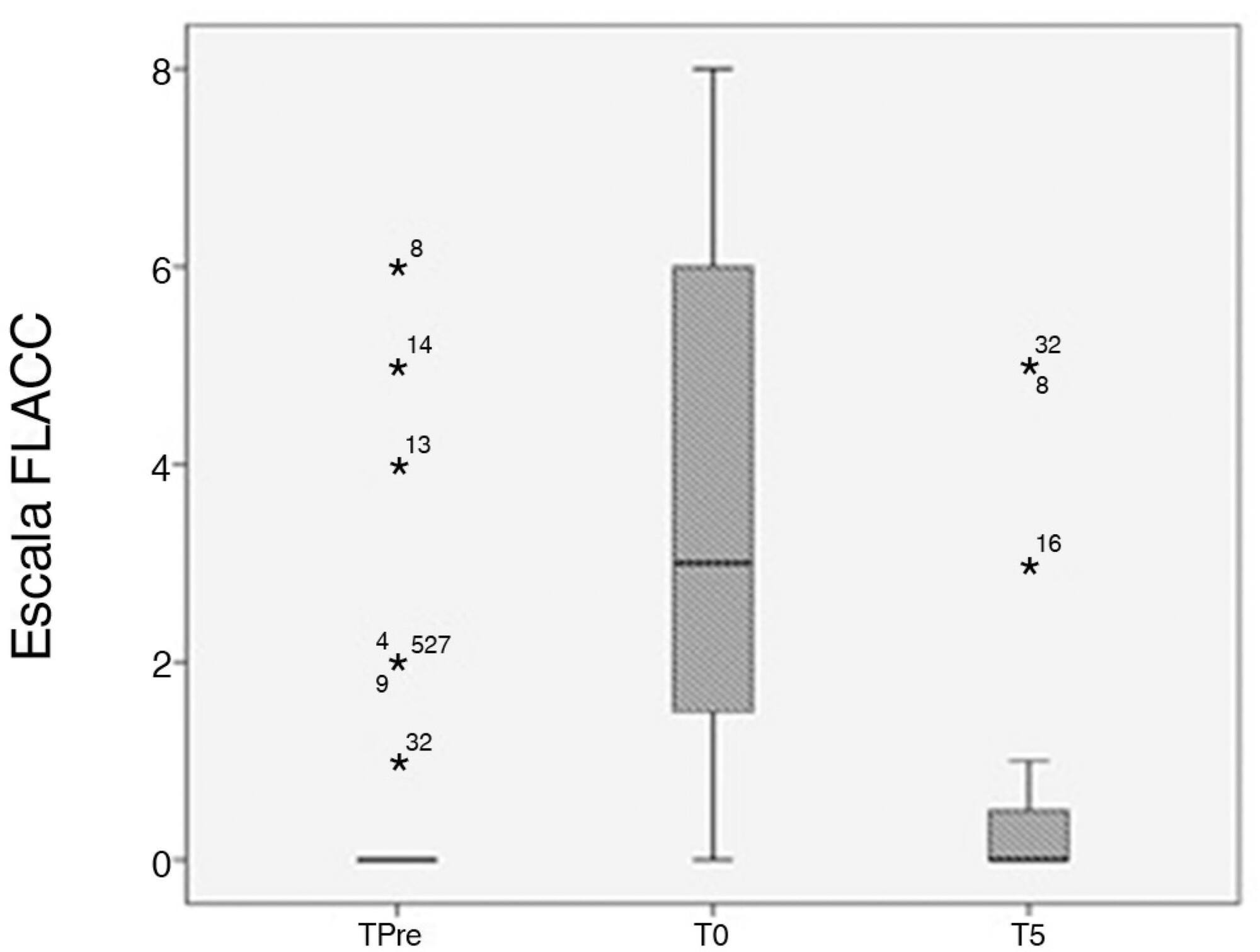
This study assessed pain and observed physiological parameters in sedated and mechanically ventilated children during a routine procedure.
This observational study was performed in a pediatric intensive care unit. Thirty-five children between 1 month and 12 years of age were assessed before, during, and five minutes after an arterial blood collection for gas analysis (painful procedure). Face, Legs, Activity, Cry and Consolability scale was used to assess pain. In addition, patients' heart rate, respiratory rate, peripheral saturation of oxygen and blood pressure (diastolic and systolic) were recorded. COMFORT-B scale was applied before the pain and physiological parameter assessments to verify sedation level of the subjects.
There was an increase in Face, Legs, Activity, Cry and Consolability score (p = 0.0001) during painful stimuli. There was an increase in heart rate (p = 0.03), respiratory rate (p = 0.001) and diastolic blood pressure (p = 0.006) due to pain caused by the routine procedure.
This study suggests that assessments of pain using standard scales, such as Face, Legs, Activity, Cry and Consolability score, and other physiological parameters should be consistently executed to optimize pain management in pediatric intensive care units.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):55-61
DOI 10.5935/0103-507X.20160003
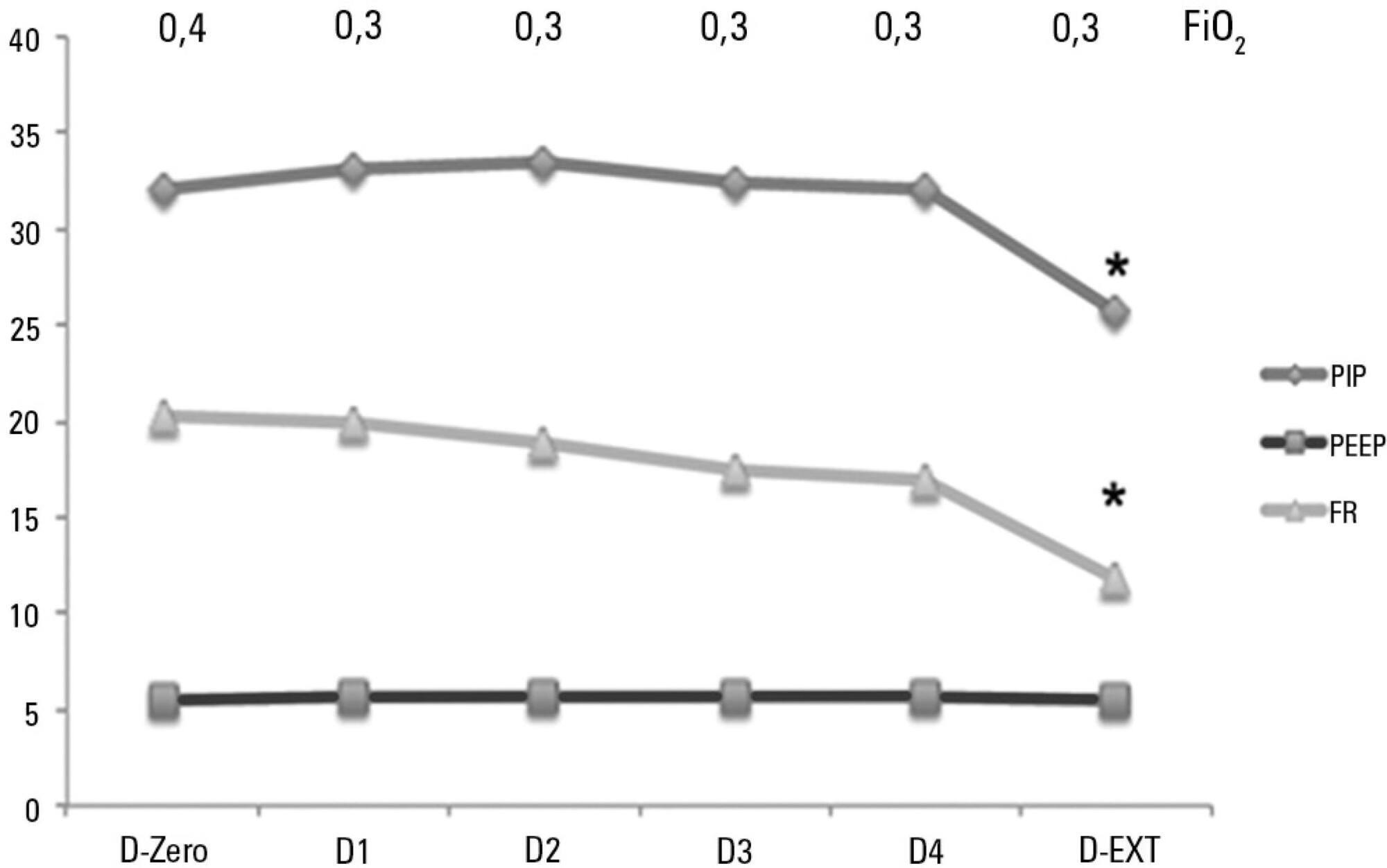
To analyze the characteristics of children with acute viral bronchiolitis subjected to mechanical ventilation for three consecutive years and to correlate their progression with mechanical ventilation parameters and fluid balance.
Longitudinal study of a series of infants (< one year old) subjected to mechanical ventilation for acute viral bronchitis from January 2012 to September 2014 in the pediatric intensive care unit. The children's clinical records were reviewed, and their anthropometric data, mechanical ventilation parameters, fluid balance, clinical progression, and major complications were recorded.
Sixty-six infants (3.0 ± 2.0 months old and with an average weight of 4.7 ± 1.4kg) were included, of whom 62% were boys; a virus was identified in 86%. The average duration of mechanical ventilation was 6.5 ± 2.9 days, and the average length of stay in the pediatric intensive care unit was 9.1 ± 3.5 days; the mortality rate was 1.5% (1/66). The peak inspiratory pressure remained at 30cmH2O during the first four days of mechanical ventilation and then decreased before extubation (25 cmH2O; p < 0.05). Pneumothorax occurred in 10% of the sample and extubation failure in 9%, which was due to upper airway obstruction in half of the cases. The cumulative fluid balance on mechanical ventilation day four was 402 ± 254mL, which corresponds to an increase of 9.0 ± 5.9% in body weight. Thirty-seven patients (56%) exhibited a weight gain of 10% or more, which was not significantly associated with the ventilation parameters on mechanical ventilation day four, extubation failure, duration of mechanical ventilation or length of stay in the pediatric intensive care unit.
The rate of mechanical ventilation for acute viral bronchiolitis remains constant, being associated with low mortality, few adverse effects, and positive cumulative fluid balance during the first days. Better fluid control might reduce the duration of mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):330-334
DOI 10.5935/0103-507X.20160056
To identify and evaluate the correct positioning of the most commonly used medical devices as visualized in thoracic radiograms of patients in the intensive care unit of our center.
A literature search was conducted for the criteria used to evaluate the correct positioning of medical devices on thoracic radiograms. All the thoracic radiograms performed in the intensive care unit of our center over an 18-month period were analyzed. All admissions in which at least one thoracic radiogram was performed in the intensive care unit and in which at least one medical device was identifiable in the thoracic radiogram were included. One radiogram per admission was selected for analysis. The radiograms were evaluated by an independent observer.
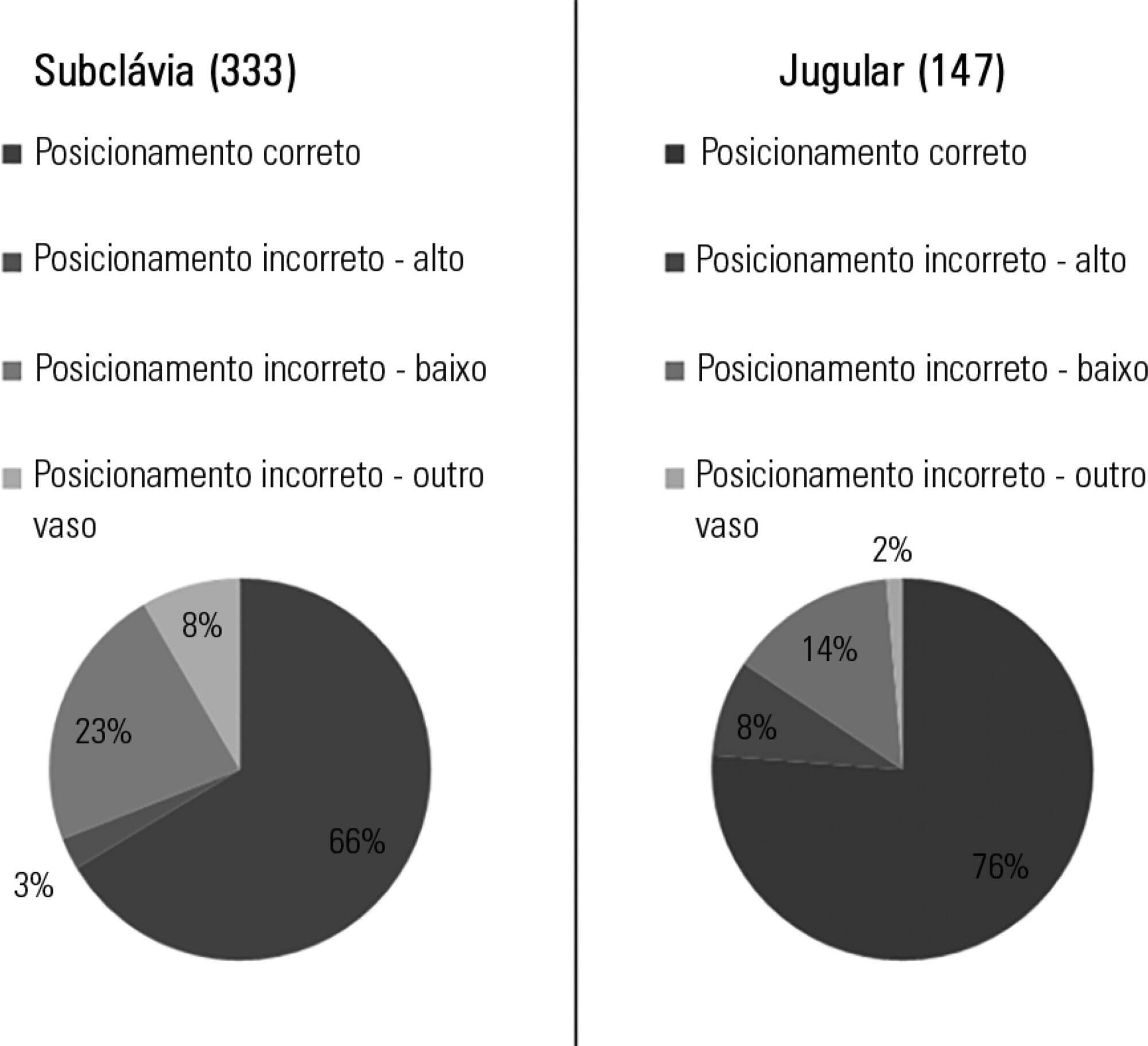
Out of the 2,312 thoracic radiograms analyzed, 568 were included in this study. Several medical devices were identified, including monitoring leads, endotracheal and tracheostomy tubes, central venous catheters, pacemakers and prosthetic cardiac valves. Of the central venous catheters that were identified, 33.6% of the subclavian and 23.8% of the jugular were malpositioned. Of the endotracheal tubes, 19.9% were malpositioned, while all the tracheostomy tubes were correctly positioned.
Malpositioning of central venous catheters and endotracheal tubes is frequently identified in radiograms of patients in an intensive care unit. This is relevant because malpositioned devices may be related to adverse events. In future studies, an association between malpositioning and adverse events should be investigated.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):335-340
DOI 10.5935/0103-507X.20160057
To evaluate the perceptions of physicians, nurses and nursing technicians of their participation in the decision-making process surrounding life support limitation in terminally ill pediatric patients, with comparisons by professional category.
A cross-sectional study was conducted in the pediatric intensive care unit of a tertiary public university hospital with the participation of physicians, nurses and nursing technicians. The MacArthur Admission Experience Survey Voice Scale was used to assess and quantify the perceptions of professionals who assisted 17 pediatric patients with life support limitation within 24 hours after the outcome of each patient was determined. All professionals working in the unit (n = 117) who were potentially eligible for the study received a free and informed consent form prior to the occurrence of the cases studied.
Study participants included 25/40 (62.5%) physicians, 10/17 (58.8%) nurses and 41/60 (68.3%) nursing technicians, representing 65% of the eligible professionals identified. The questionnaire return rate was higher for physicians than technicians (p = 0.0258). A perceived lack of voice was reported in all three professional categories at varying rates that were lower for physicians than for nurses and nursing technicians (p < 0.00001); there was no difference between the latter (p = 0.7016). In the three professional categories studied, three subscale items were reported. For two of the three statements, there were significant differences between physicians and nurses (p = 0.004) and between physicians and nursing technicians (p = 0.001). For one of the statements, there was no difference among the three professional categories.
Respondents perceived a lack of voice in the decision-making process at varying rates across the three categories of studied professionals who assisted terminally ill pediatric patients with life support limitation, with physicians expressing lowered rates of perceived coercion.