Abstract
Rev Bras Ter Intensiva. 2017;29(2):180-187
DOI 10.5935/0103-507X.20170028
To analyze patients after cardiac surgery that needed endotracheal reintubation and identify factors associated with death and its relation with the severity scores.
Retrospective analysis of information of 1,640 patients in the postoperative period of cardiac surgery between 2007 and 2015.
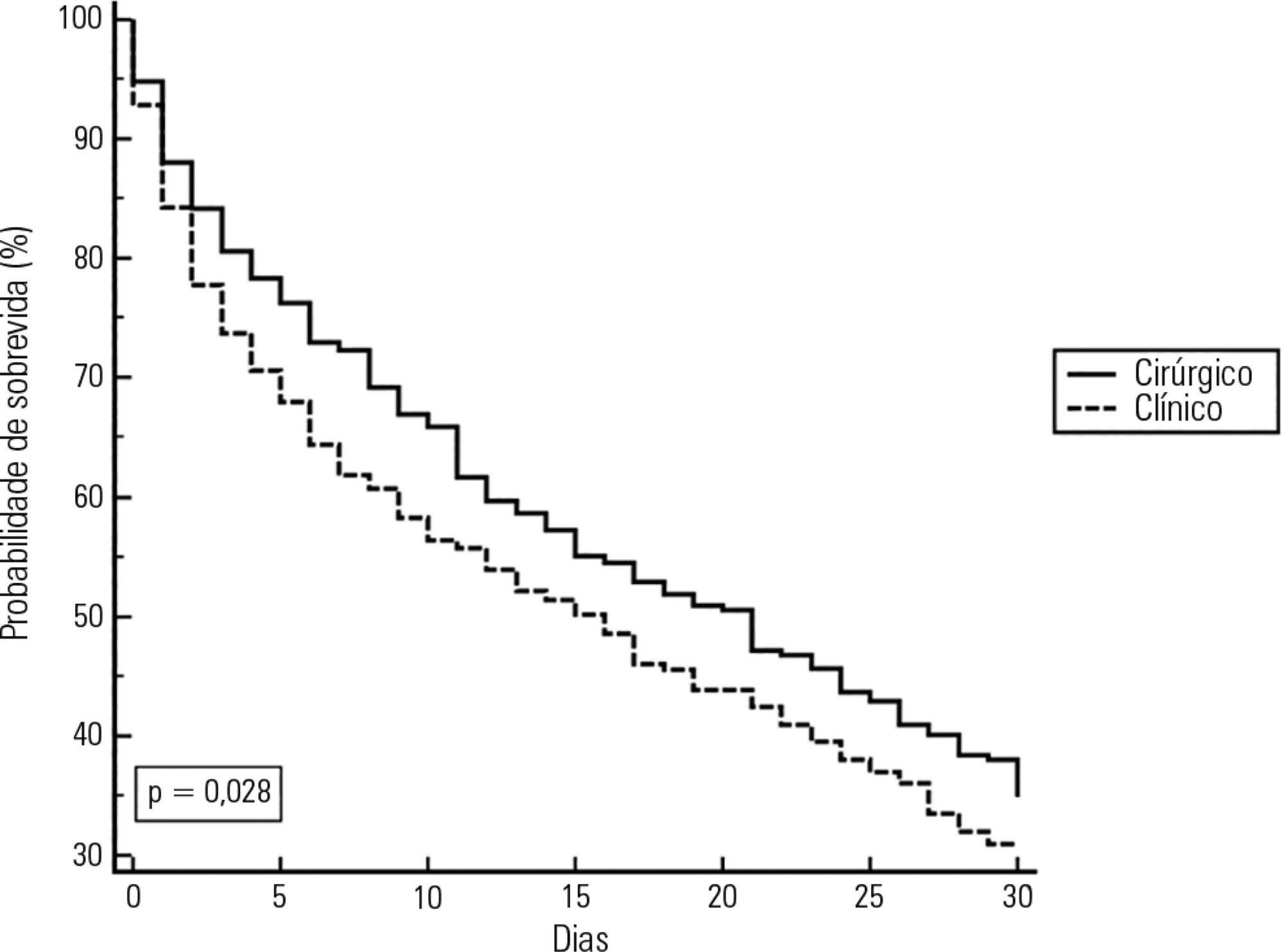
The reintubation rate was 7.26%. Of those who were reintubated, 36 (30.3%) underwent coronary artery bypass surgery, 27 (22.7%) underwent valve replacement, 25 (21.0%) underwent correction of an aneurysm, and 8 (6.7%) underwent a heart transplant. Among those with comorbidities, 54 (51.9%) were hypertensive, 22 (21.2%) were diabetic, and 10 (9.6%) had lung diseases. Among those who had complications, 61 (52.6%) had pneumonia, 50 (42.4%) developed renal failure, and 49 (51.0%) had a moderate form of the transient disturbance of gas exchange. Noninvasive ventilation was performed in 53 (44.5%) patients. The death rate was 40.3%, and mortality was higher in the group that did not receive noninvasive ventilation before reintubation (53.5%). Within the reintubated patients who died, the SOFA and APACHE II values were 7.9 ± 3.0 and 16.9 ± 4.5, respectively. Most of the reintubated patients (47.5%) belonged to the high-risk group, EuroSCORE (> 6 points).
The reintubation rate was high, and it was related to worse SOFA, APACHE II and EuroSCORE scores. Mortality was higher in the group that did not receive noninvasive ventilation before reintubation.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):206-212
DOI 10.5935/0103-507X.20170029
To assess the frequency of primary multiple organ failure and the role of sepsis as a causative agent in critically ill pediatric patients; and calculate and evaluate the accuracy of the Pediatric Risk of Mortality III (PRISM III) and Pediatric Logistic Organ Dysfunction (PELOD) scores to predict the outcomes of critically ill children.
Retrospective study, which evaluated data from patients admitted from January to December 2011 in the pediatric intensive care unit of the Children's Hospital of the University of Cairo.
Out of 237 patients in the study, 72% had multiple organ dysfunctions, and 45% had sepsis with multiple organ dysfunctions. The mortality rate in patients with multiple organ dysfunction was 73%. Independent risk factors for death were mechanical ventilation and neurological failure [OR: 36 and 3.3, respectively]. The PRISM III score was more accurate than the PELOD score in predicting death, with a Hosmer-Lemeshow X2 (Chi-square value) of 7.3 (df = 8, p = 0.5). The area under the curve was 0.723 for PRISM III and 0.78 for PELOD.
A multiple organ dysfunctions was associated with high mortality. Sepsis was the major cause. Pneumonia, diarrhea and central nervous system infections were the major causes of sepsis. PRISM III had a better calibration than the PELOD for prognosis of the patients, despite the high frequency of the multiple organ dysfunction syndrome.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):213-221
DOI 10.5935/0103-507X.20170030
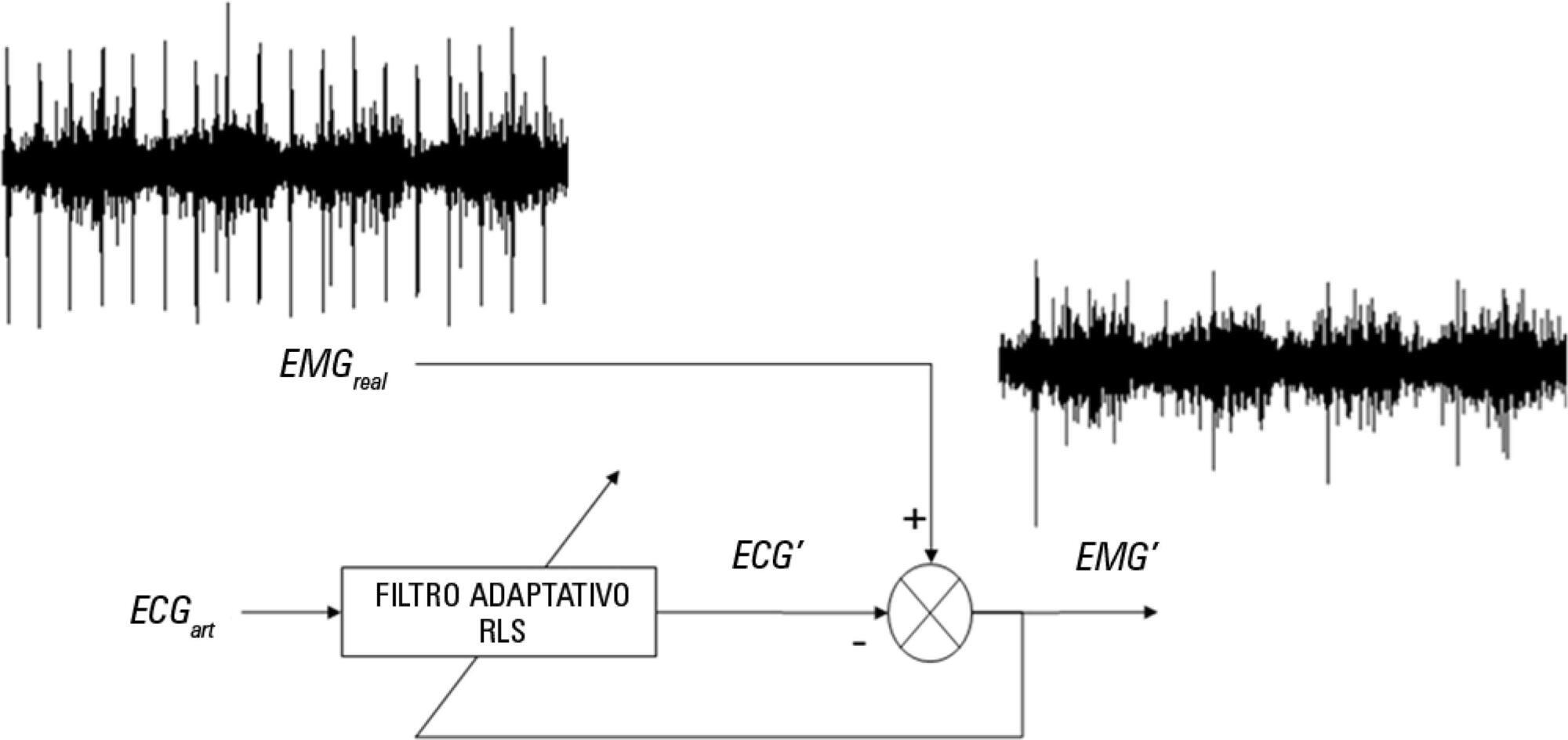
The aim of this pilot study was to evaluate the feasibility of surface electromyographic signal derived indexes for the prediction of weaning outcomes among mechanically ventilated subjects after cardiac surgery.
A sample of 10 postsurgical adult subjects who received cardiovascular surgery that did not meet the criteria for early extubation were included. Surface electromyographic signals from diaphragm and ventilatory variables were recorded during the weaning process, with the moment determined by the medical staff according to their expertise. Several indexes of respiratory muscle expenditure from surface electromyography using linear and non-linear processing techniques were evaluated. Two groups were compared: successfully and unsuccessfully weaned patients.
The obtained indexes allow estimation of the diaphragm activity of each subject, showing a correlation between high expenditure and weaning test failure.
Surface electromyography is becoming a promising procedure for assessing the state of mechanically ventilated patients, even in complex situations such as those that involve a patient after cardiovascular surgery.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):337-345
DOI 10.5935/0103-507X.20170058
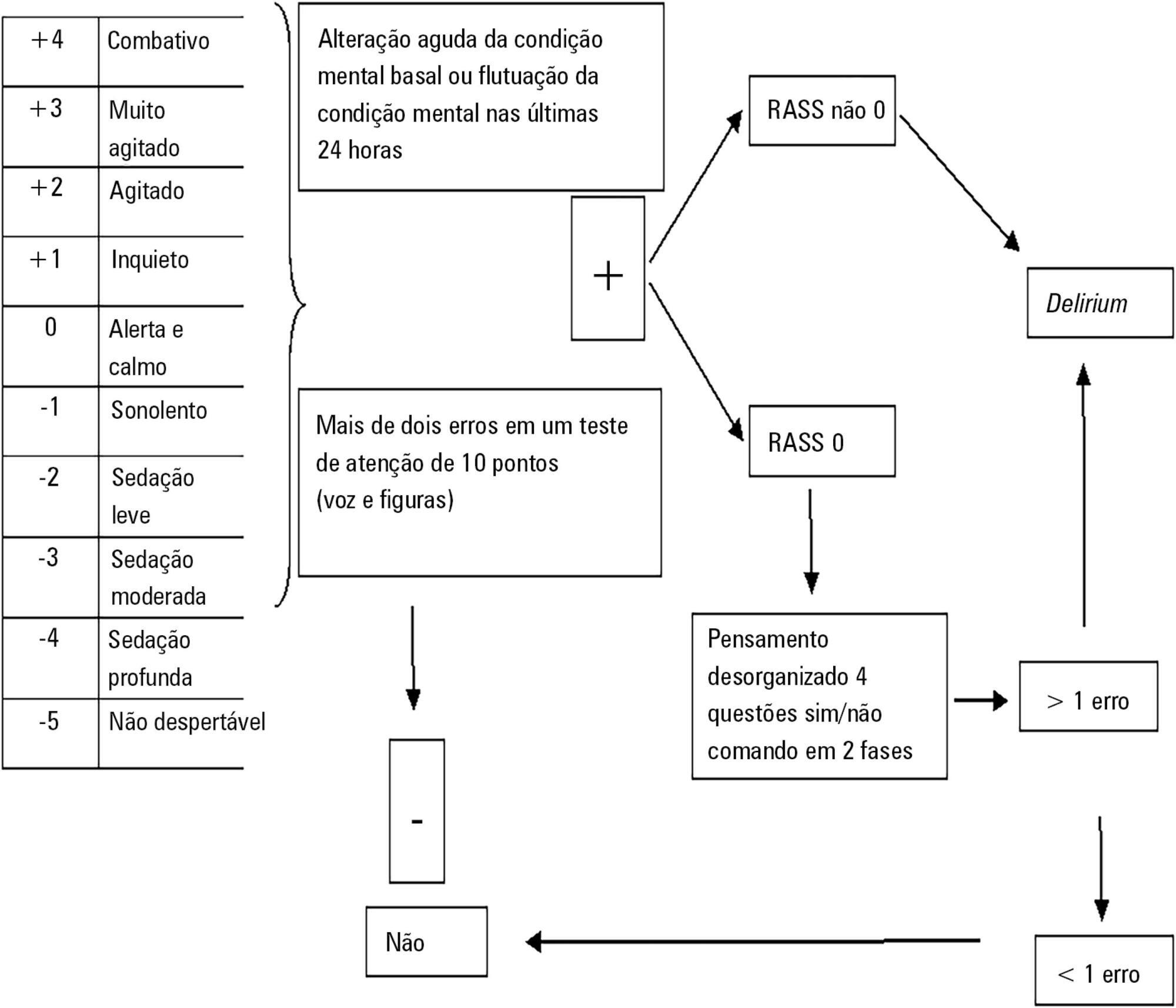
To establish the prevalence of delirium in a general intensive care unit and to identify associated factors, clinical expression and the influence on outcomes.
This was a prospective cohort study in a medical surgical intensive care unit. The Richmond Agitation-Sedation Scale and Confusion Assessment Method for the Intensive Care Unit were used daily to identify delirium in mechanically ventilated patients.
In this series, delirium prevalence was 80% (N = 184 delirious patients out of 230 patients). The number of patients according to delirium psychomotor subtypes was as follows: 11 hyperactive patients (6%), 9 hypoactive patients (5%) and 160 mixed patients (89%). Multiple logistic regression modeling using delirium as the dependent outcome variable (to study the risk factors for delirium) revealed that age > 65 years, history of alcohol consumption, and number of mechanical ventilation days were independent variables associated with the development of delirium. The multiple logistic regression model using hospital mortality as the dependent outcome variable (to study the risk factors for death) showed that severity of illness, according to the Acute Physiology and Chronic Health Evaluation II, mechanical ventilation for more than 7 days, and sedation days were all independent predictors for excess hospital mortality.
This Latin American prospective cohort investigation confirmed specific factors important for the development of delirium and the outcome of death among general intensive care unit patients. In both analyses, we found that the duration of mechanical ventilation was a predictor of untoward outcomes.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):436-443
DOI 10.5935/0103-507X.20170070
To define the frequency of cytomegalovirus disease among kidney transplant patients in an intensive care unit in which this complication was suspected and to identify predisposing factors and their possible impact on clinical outcome.
Retrospective observational study in which kidney transplant patients over the age of 18 years were hospitalized for any reason in an intensive care unit with at least one collection of samples to test for the presence of antigenemia or cytomegalovirus via polymerase chain reaction during hospitalization. Cytomegalovirus disease was defined as positive antigenemia or polymerase chain reaction above 500 copies/mL in the presence of symptoms and in the appropriate clinical setting, as judged by the attending physician.
A total of 99 patients were included (age: 53.4 ± 12.8 years, 71.6% male). Cytomegalovirus disease was diagnosed in 39 patients (39.4%). Respiratory symptoms (51%), non-specific clinical worsening (20%) or gastrointestinal symptoms (14%) were the main reasons for exam collection. Transplant time was lower in those with cytomegalovirus disease than in those without this diagnosis (6.5 months and 31.2 months, p = 0.001), along with pulse therapy in the last 6 months (41% and 16.9%, p = 0.008) and previous use of thymoglobulin in the last year (35.9% and 6.8%, p < 0.001). In the logistic regression model, only the transplant time and the use of thymoglobulin were associated with a higher frequency of cytomegalovirus. There was no difference in clinical evolution between patients with and without cytomegalovirus disease.
In kidney transplant patients suspected of cytomegalovirus disease, the prevalence was high. Transplant time less than 6 months, and the use of thymoglobulin in the last year should increase the intensivist's suspicion for this complication.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):453-459
DOI 10.5935/0103-507X.20170069
To assess the performance of the Pediatric Index of Mortality (PIM) 2 and the Risk Adjustment for Congenital Heart Surgery (RACHS) in the postoperative period of congenital heart disease patients.
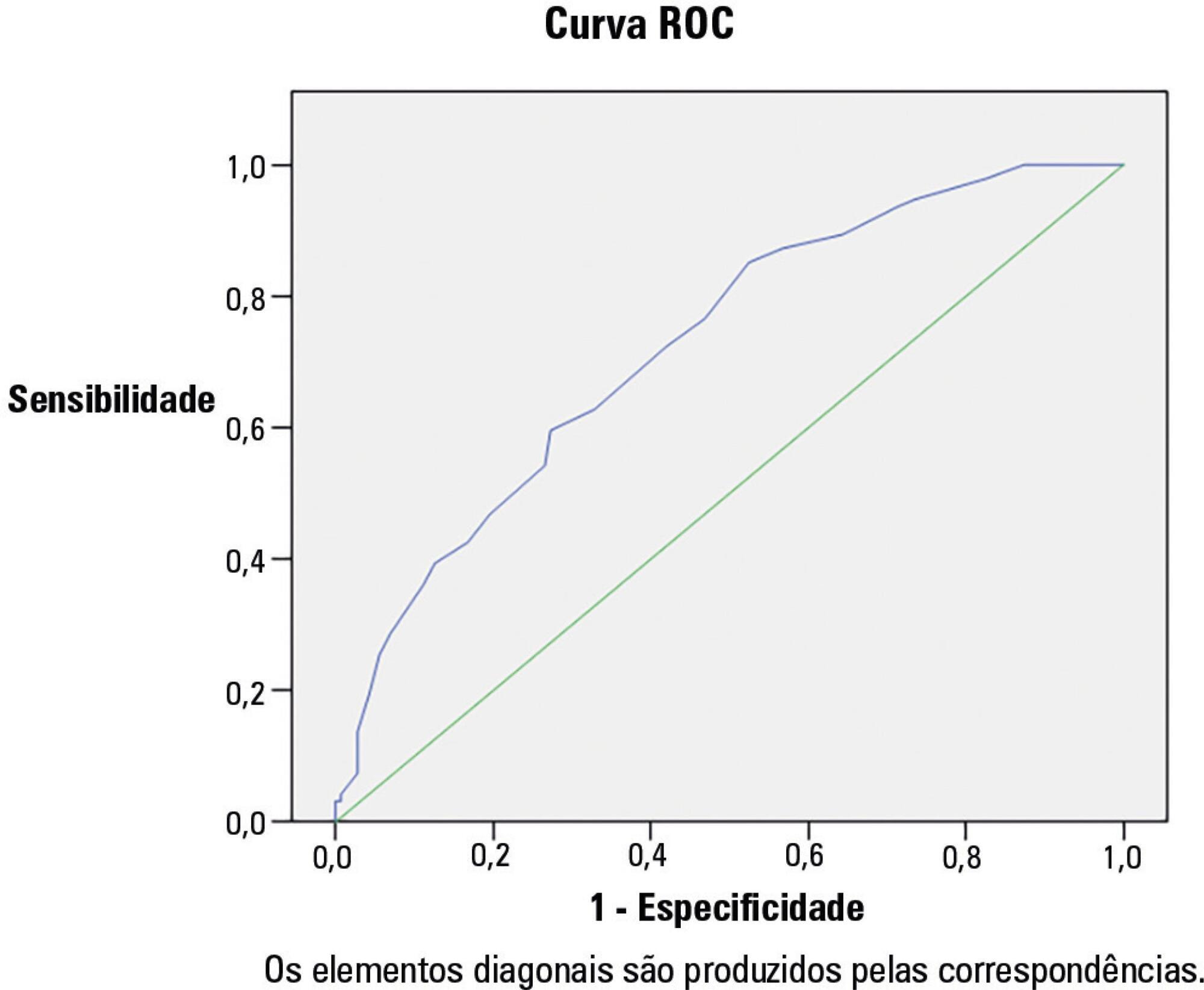
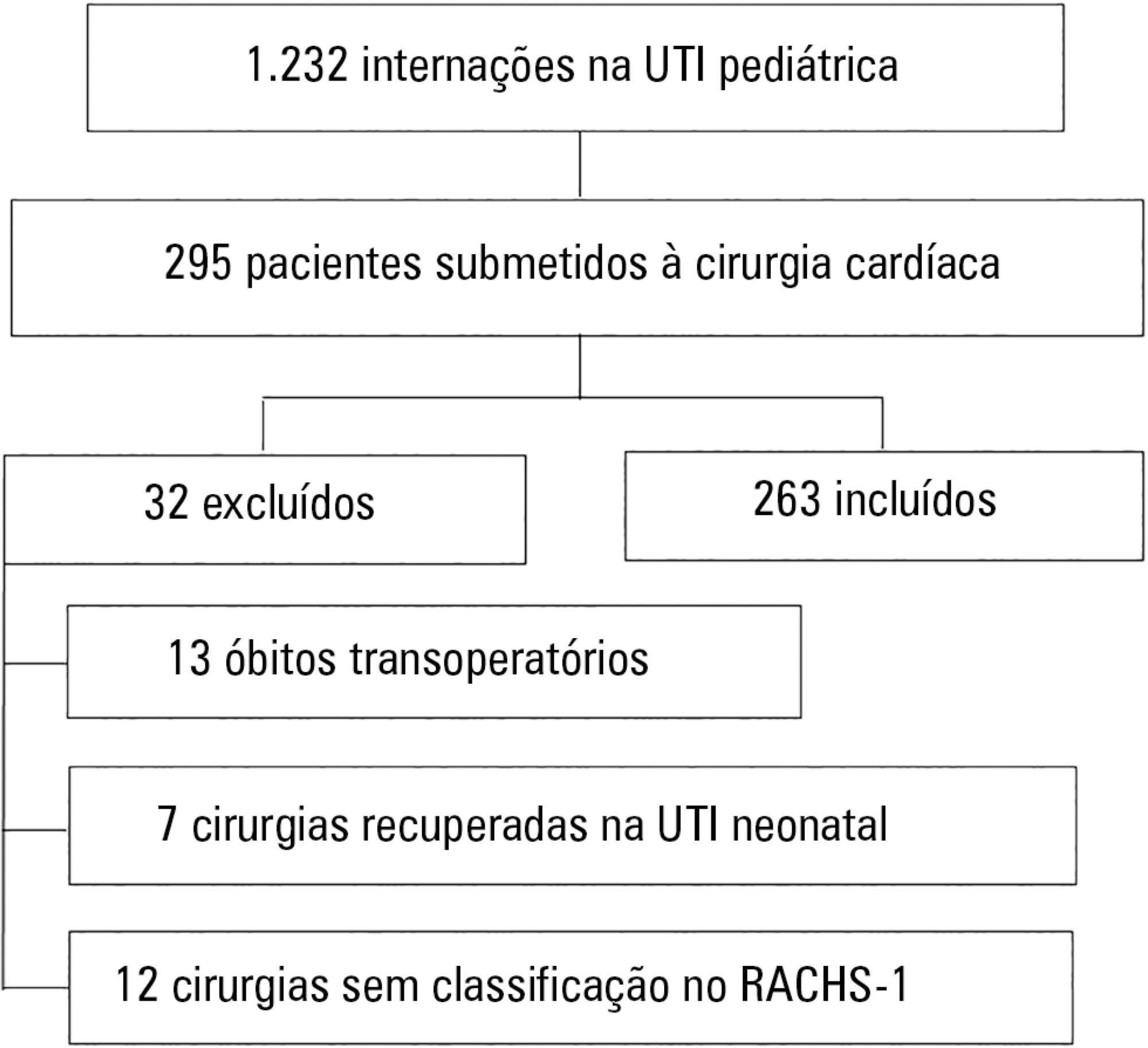
Retrospective cross-sectional study. Data were collected from patient records to generate the scores and predictions using recommended techniques, demographic data and outcomes. The Mann-Whitney test, Hosmer-Lemeshow test, standardized mortality rate, area under the receiver operating characteristic (ROC) curve, chi square test, Poisson regression with robust variance and Spearman's test were used for statistical analysis.
A total of 263 patients were evaluated, and 72 died (27.4%). These patients presented significantly higher PIM-2 values than survivors (p < 0.001). In the RACHS-1 classification, mortality was progressively higher according to the complexity of the procedure, with a 3.24-fold increase in the comparison between groups 6 and 2. The area under the ROC curve for PIM-2 was 0.81 (95%CI 0.75 - 0.87), while for RACHS-1, it was 0.70 (95%CI 0.63 - 0.77). The RACHS presented better calibration power in the sample analyzed. A significantly positive correlation was found between the results of both scores (rs = 0.532; p < 0.001).
RACHS presented good calibration power, and RACHS-1 and PIM-2 demonstrated good performance with regard to their discriminating capacities between survivors and non-survivors. Moreover, a positive correlation was found between the results of the two risk scores.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):476-480
DOI 10.5935/0103-507X.20170071
To evaluate the intra- and inter-reliability and the ease of measuring the quadriceps muscle thickness using bedside ultrasound.
This is a prospective, observational study. The assessment of quadriceps muscle thickness was performed at two reference points and was quantified using portable B-mode ultrasound in two healthy volunteers. For standardization of measurements and validation of image collections, the team was trained through theoretical and practical classes, with a 6-hour workload.
A total of 112 images were examined by the coach and compared with the trainees. Pearson's correlation analysis found an excellent relationship between the coach and all trainees (R2 > 0.90). The best association was between the coach and the dietitians (R2: 0.99; p < 0.001), and the worst association was between the coach and the medical trainees (R2: 0.92; p < 0.001). In the Bland-Altman comparison, the highest error rate found between coach and trainees was 5.12% (95% confidence interval [CI] 3.64-12.37), and the lowest was 1.01% (95%CI 0.72 - 2.58); the highest bias of the values described was -0.12 ± 0.19, and the lowest was -0.01 ± 0.04.
The data analyzed showed a good correlation between the measurements made by the coach and trainees, indicating that ultrasound of the quadriceps muscle is a viable and easily applicable tool.

Abstract
Rev Bras Ter Intensiva. 2016;28(3):278-284
DOI 10.5935/0103-507X.20160045
To evaluate the implementation of a multidisciplinary rapid response team led by an intensive care physician at a university hospital.
This retrospective cohort study analyzed assessment forms that were completed during the assessments made by the rapid response team of a university hospital between March 2009 and February 2014.
Data were collected from 1,628 assessments performed by the rapid response team for 1,024 patients and included 1,423 code yellow events and 205 code blue events. The number of assessments was higher in the first year of operation of the rapid response team. The multivariate analysis indicated that age (OR 1.02; 95%CI 1.02 - 1.03; p < 0.001), being male (OR 1.48; 95%CI 1.09 - 2.01; p = 0.01), having more than one assessment (OR 3.31; 95%CI, 2.32 - 4.71; p < 0.001), hospitalization for clinical care (OR 1.77; 95%CI 1.29 - 2.42; p < 0.001), the request of admission to the intensive care unit after the code event (OR 4.75; 95%CI 3.43 - 6.59; p < 0.001), and admission to the intensive care unit before the code event (OR 2.13; 95%CI 1.41 - 3.21; p = 0.001) were risk factors for hospital mortality in patients who were seen for code yellow events.
The hospital mortality rates were higher than those found in previous studies. The number of assessments was higher in the first year of operation of the rapid response team. Moreover, hospital mortality was higher among patients admitted for clinical care.