Abstract
Rev Bras Ter Intensiva. 2017;29(1):47-54
DOI 10.5935/0103-507X.20170008
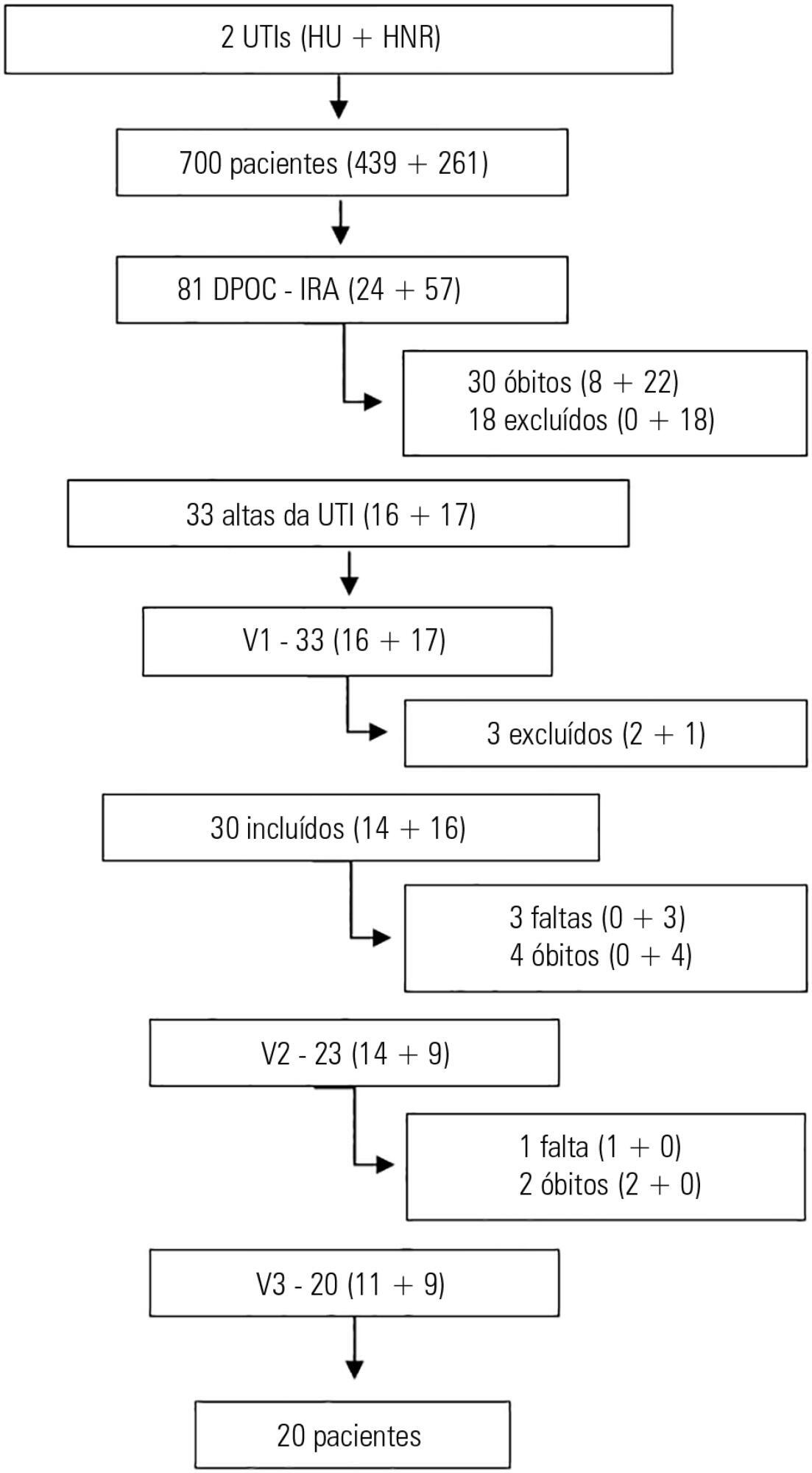
The purpose of this study was to evaluate the clinical/functional aspects and quality of life of chronic obstructive pulmonary disease patients who were discharged after an intensive care unit admission for acute respiratory failure.
This prospective study included chronic obstructive pulmonary disease patients who were admitted to two intensive care units between December of 2010 and August of 2011 and evaluated over three visits after discharge. Thirty patients were included, and 20 patients completed the three-month follow up.
There was a significant improvement in the following: forced expiratory flow in one second (L) (1.1/1.4/1.4; p = 0.019), six-minute walk test (m) (- /232.8 /272.6; p = 0.04), BODE score (7.5/5.0/3.8; p = 0.001), cognition measured by the Mini Mental State Examination (21/23.5/23.5; p = 0.008) and quality of life measured by the total Saint George Respiratory Questionnaire score (63.3/56.8/51, p = 0.02). The mean difference in the total score was 12.3 (between visits 1 and three). Important clinical differences were observed for the symptom score (18.8), activities score (5.2) and impact score (14.3). The majority of participants (80%) reported they would be willing to undergo a new intensive care unit admission.
Despite the disease severity, there was a significant clinical, functional and quality of life improvement at the end of the third month. Most patients would be willing to undergo a new intensive care unit admission.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):154-162
DOI 10.5935/0103-507X.20170025
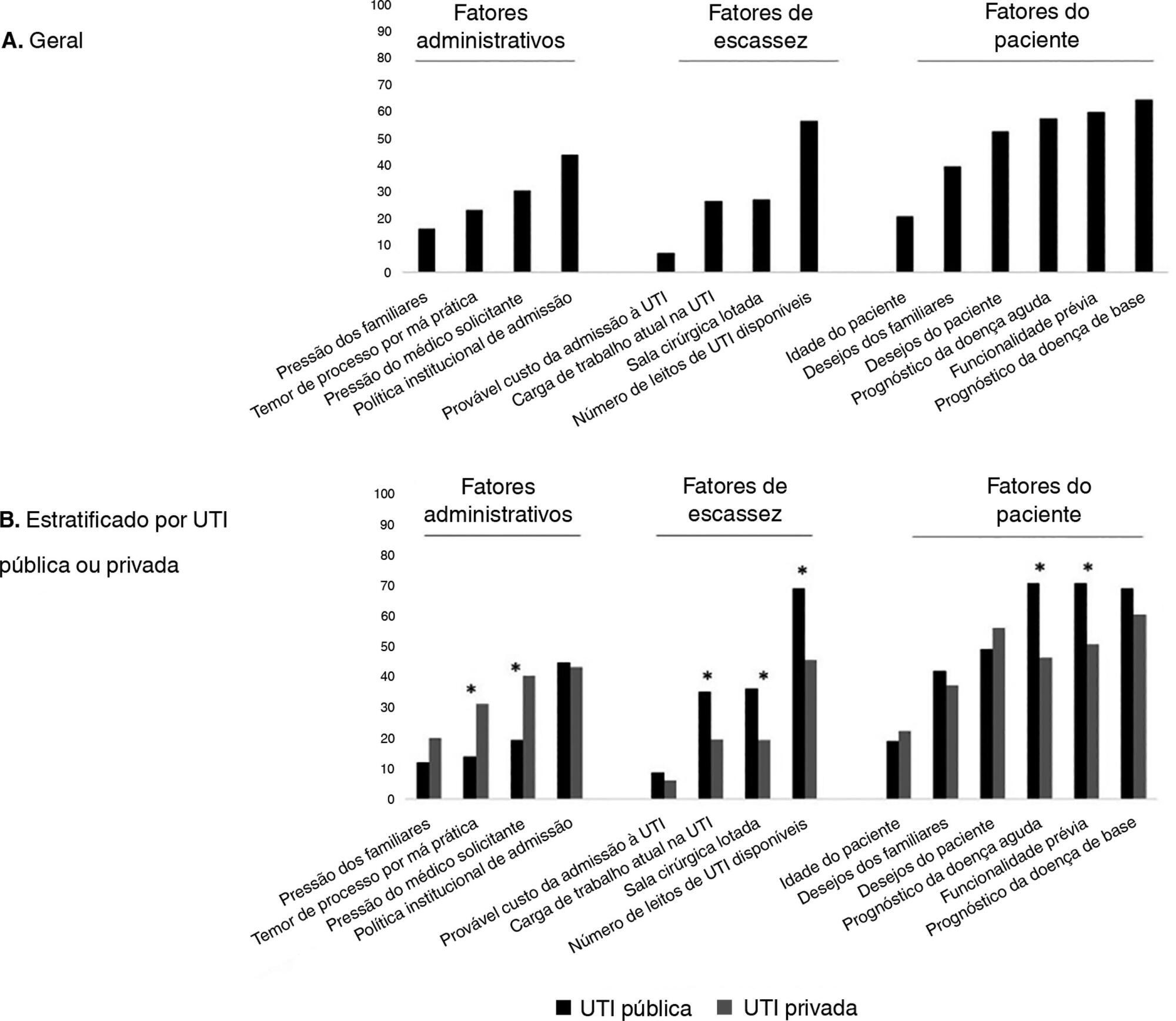
To evaluate the factors potentially associated with the decision of admission to the intensive care unit in Brazil.
An electronic survey of Brazilian physicians working in intensive care units. Fourteen variables that were potentially associated with the decision of admission to the intensive care unit were rated as important (from 1 to 5) by the respondents and were later grouped as "patient-related," "scarcity-related" and "administrative-related" factors. The workplace and physician characteristics were evaluated for correlation with the factor ratings.
During the study period, 125 physicians completed the survey. The scores on patient-related factors were rated higher on their potential to affect decisions than scarcity-related or administrative-related factors, with a mean ± SD of 3.42 ± 0.7, 2.75 ± 0.7 and 2.87 ± 0.7, respectively (p < 0.001). The patient's underlying illness prognosis was rated by 64.5% of the physicians as always or frequently affecting decisions, followed by acute illness prognosis (57%), number of intensive care unit beds available (56%) and patient's wishes (53%). After controlling for confounders, receiving specific training on intensive care unit triage was associated with higher ratings of the patient-related factors and scarcity-related factors, while working in a public intensive care unit (as opposed to a private intensive care unit) was associated with higher ratings of the scarcity-related factors.
Patient-related factors were more frequently rated as potentially affecting intensive care unit admission decisions than scarcity-related or administrative-related factors. Physician and workplace characteristics were associated with different factor ratings.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):55-62
DOI 10.5935/0103-507X.20170009
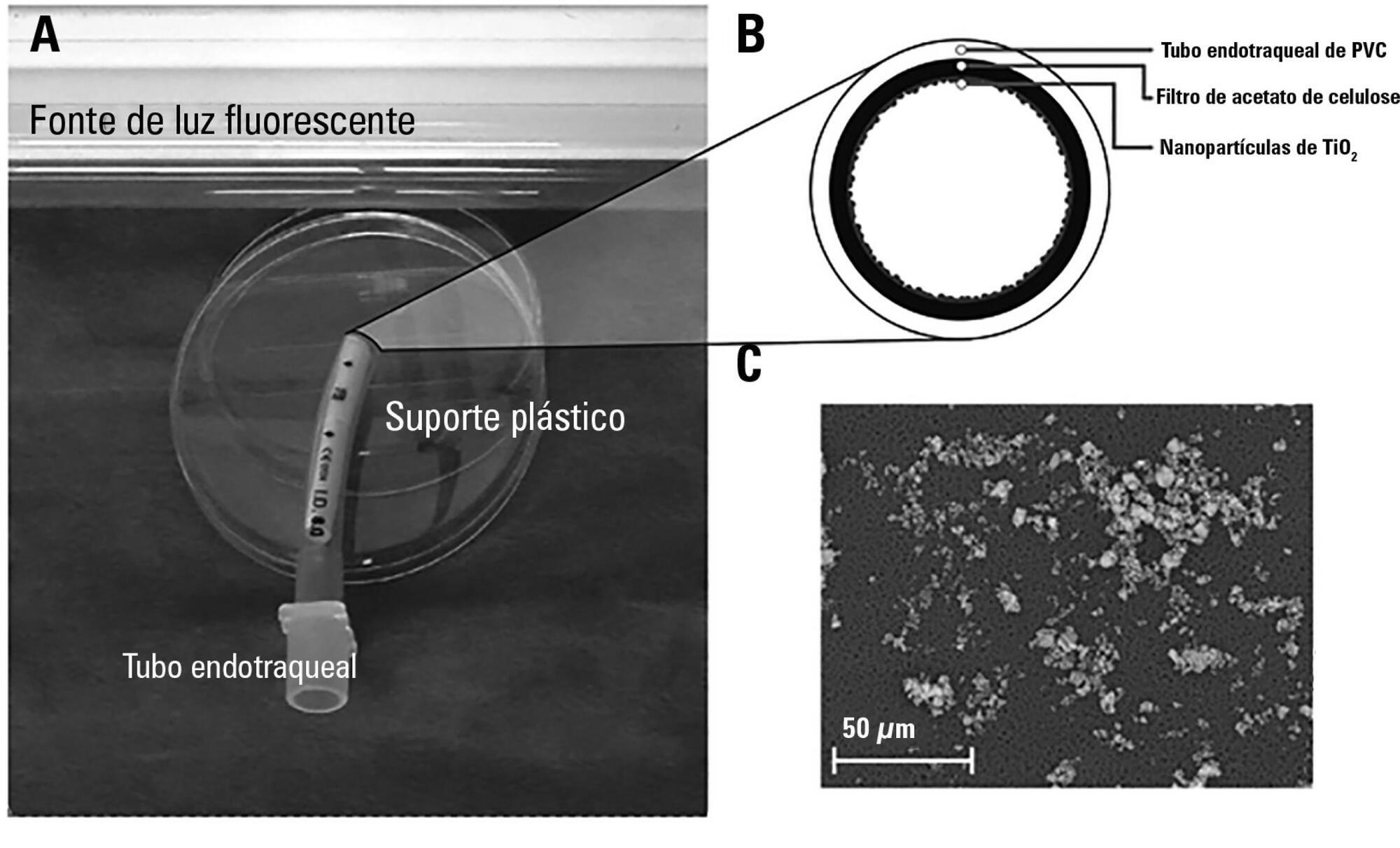
The aim of this study was to assess the antibacterial activity against Staphylococcus aureus and Pseudomonas aeruginosa of two nanoparticle endotracheal tube coatings with visible light-induced photocatalysis.
Two types of titanium dioxide nanoparticles were tested: standard anatase (TiO2) and N-doped TiO2 (N-TiO2). Nanoparticles were placed on the internal surface of a segment of commercial endotracheal tubes, which were loaded on a cellulose acetate filter; control endotracheal tubes were left without a nanoparticle coating. A bacterial inoculum of 150 colony forming units was placed in the endotracheal tubes and then exposed to a fluorescent light source (3700 lux, 300-700 nm wavelength) for 5, 10, 20, 40, 60 and 80 minutes. Colony forming units were counted after 24 hours of incubation at 37°C. Bacterial inactivation was calculated as the percentage reduction of bacterial growth compared to endotracheal tubes not exposed to light.
In the absence of light, no relevant antibacterial activity was shown against neither strain. For P. aeruginosa, both coatings had a higher bacterial inactivation than controls at any time point (p < 0.001), and no difference was observed between TiO2 and N-TiO2. For S. aureus, inactivation was higher than for controls starting at 5 minutes for N-TiO2 (p = 0.018) and 10 minutes for TiO2 (p = 0.014); inactivation with N-TiO2 was higher than that with TiO2 at 20 minutes (p < 0.001), 40 minutes (p < 0.001) and 60 minutes (p < 0.001).
Nanosized commercial and N-doped TiO2 inhibit bacterial growth under visible fluorescent light. N-TiO2 has higher antibacterial activity against S. aureus compared to TiO2.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):63-69
DOI 10.5935/0103-507X.20170010
To determine the impact of the day and time of admission and discharge from the intensive care unit on mortality.
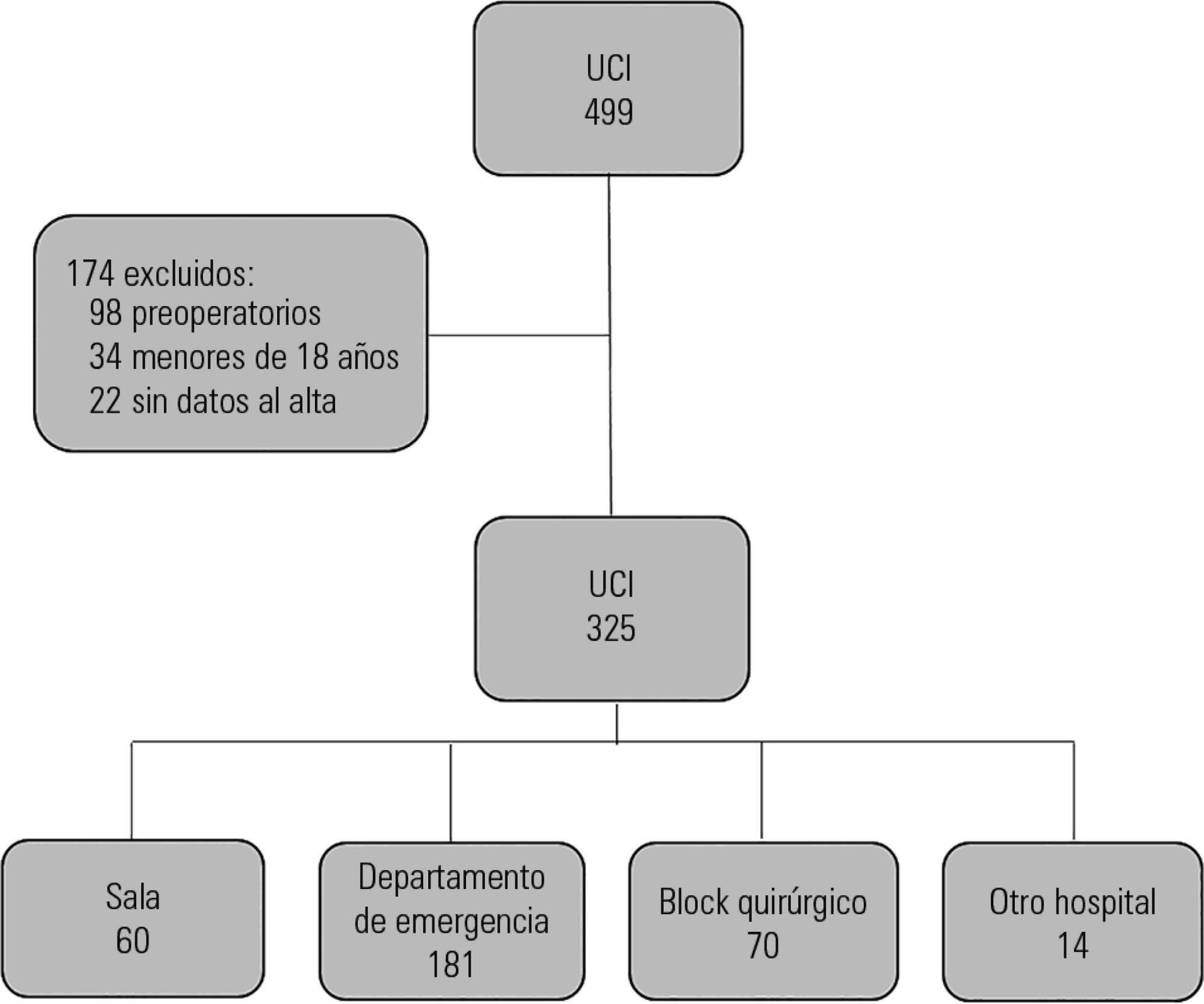
Prospective observational study that included patients admitted to the intensive care unit of the Hospital Maciel in Montevideo between April and November 2014.
We analyzed 325 patients with an average age of 55 (36 - 71) years and a SAPS II value of 43 (29 - 58) points. No differences were found in the mortality of patients in the intensive care unit when time of admission (35% on the weekend versus 31% on weekdays, p = ns) or the hour of entry (35% at night versus 31% in the daytime, p = ns) were compared. The time of discharge was associated with higher hospital mortality rates (57% for weekend discharges versus 14% for weekday discharges, p = 0.000). The factors independently associated with hospital mortality after discharge from the intensive care unit were age > 50 years (OR 2.4, 95%CI, 1.1 - 5.4) and weekend discharge (OR 7.7, 95%CI, 3.8-15.6).
This study identified the time of discharge from the intensive care unit as a factor that was independently associated with hospital mortality.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):163-170
DOI 10.5935/0103-507X.20170026
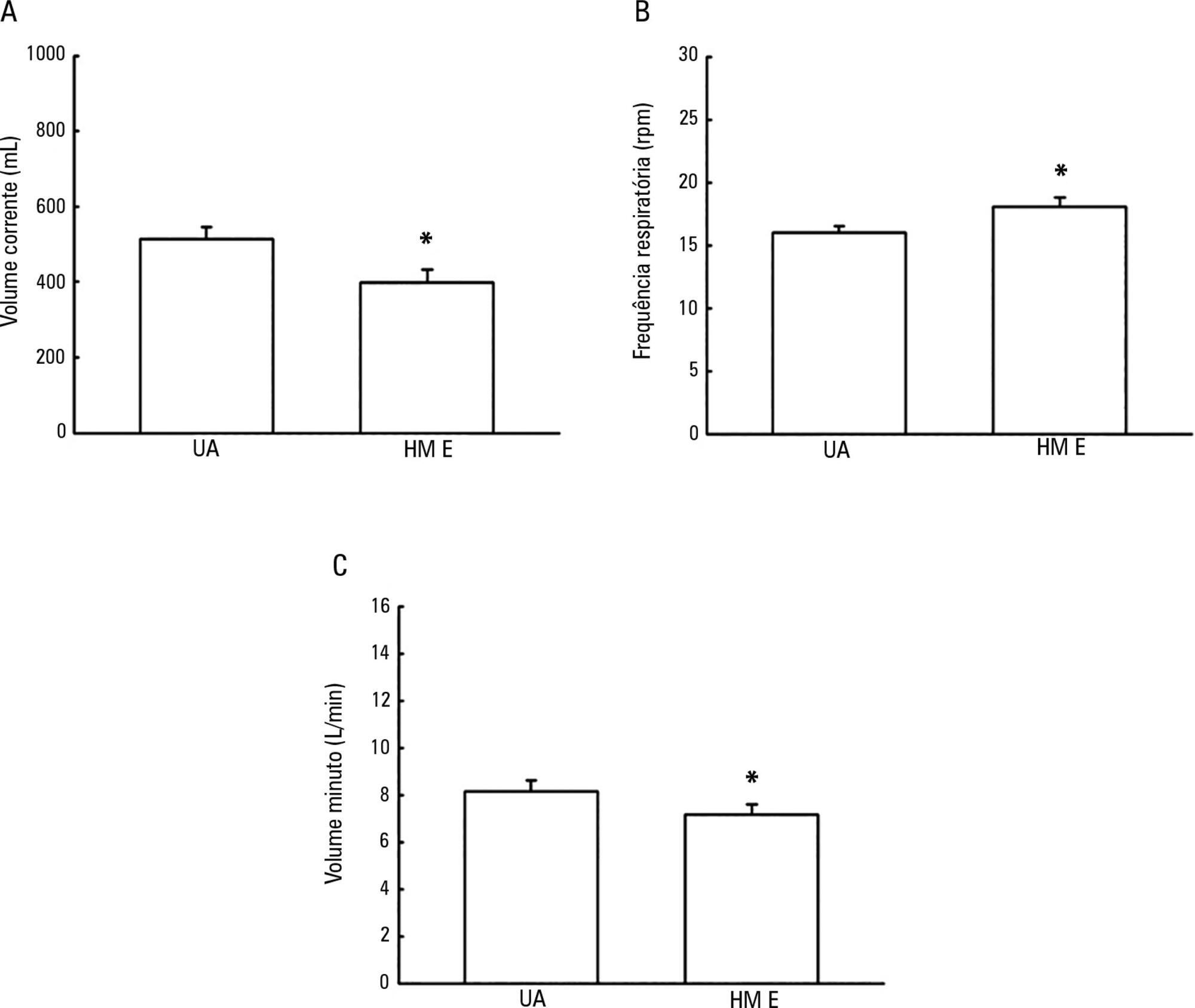
To evaluate the possible changes in tidal volume, minute volume and respiratory rate caused by the use of a heat and moisture exchanger in patients receiving pressure support mechanical ventilation and to quantify the variation in pressure support required to compensate for the effect caused by the heat and moisture exchanger.
Patients under invasive mechanical ventilation in pressure support mode were evaluated using heated humidifiers and heat and moisture exchangers. If the volume found using the heat and moisture exchangers was lower than that found with the heated humidifier, an increase in pressure support was initiated during the use of the heat and moisture exchanger until a pressure support value was obtained that enabled the patient to generate a value close to the initial tidal volume obtained with the heated humidifier. The analysis was performed by means of the paired t test, and incremental values were expressed as percentages of increase required.
A total of 26 patients were evaluated. The use of heat and moisture exchangers increased the respiratory rate and reduced the tidal and minute volumes compared with the use of the heated humidifier. Patients required a 38.13% increase in pressure support to maintain previous volumes when using the heat and moisture exchanger.
The heat and moisture exchanger changed the tidal and minute volumes and respiratory rate parameters. Pressure support was increased to compensate for these changes.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):171-179
DOI 10.5935/0103-507X.20170027
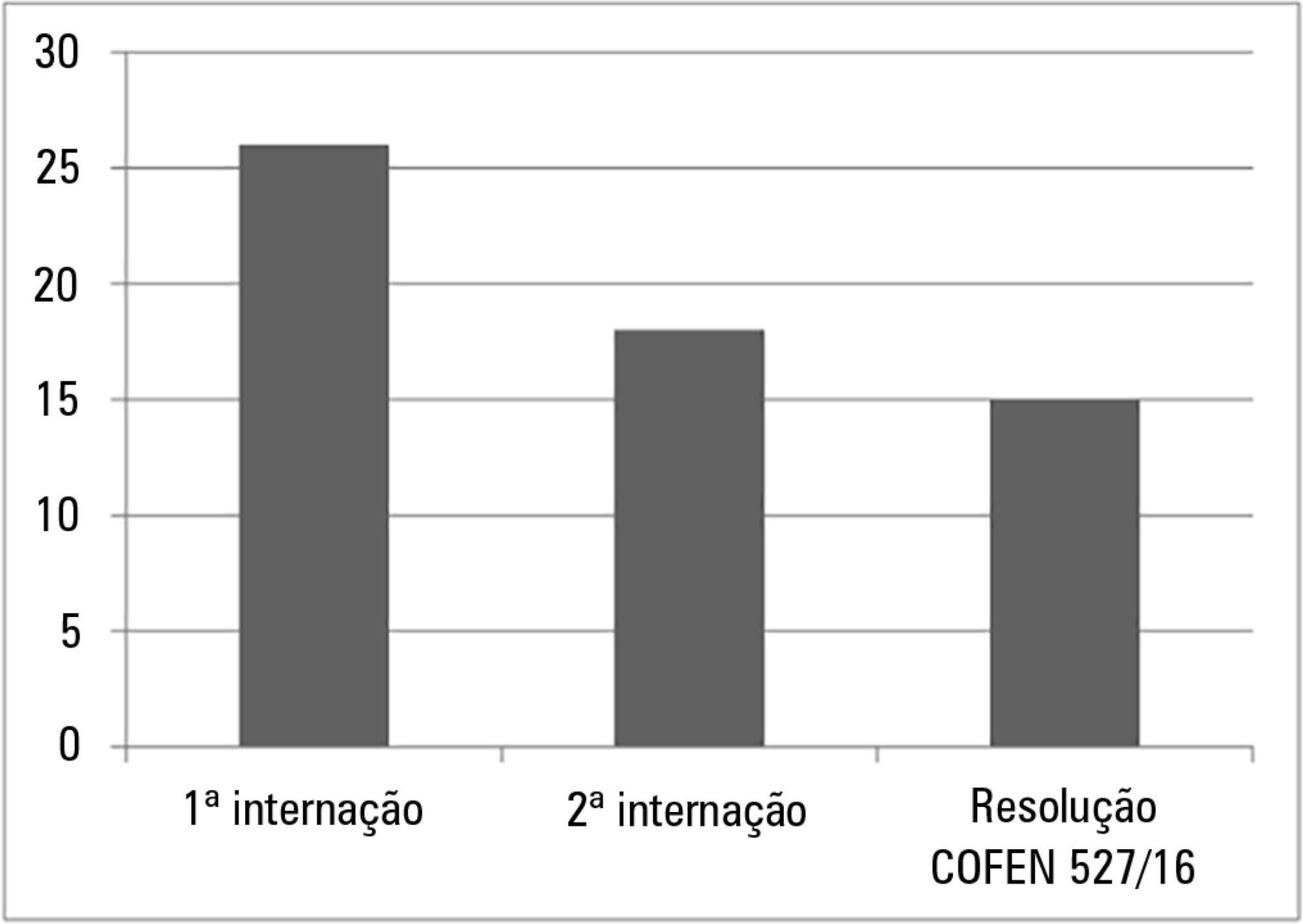
To calculate and compare the nursing staff size associated with self-care promotion at a pediatric semi-intensive care unit.
This was a prospective study in which 31 children and their caregivers participated. The nursing workload associated with each participant was evaluated at two different times (first and second hospital stays) using the Nursing Activities Score instrument. The first hospital stay corresponded to self-care promotion. Staff size was calculated according to the nursing hours recommended by the Nursing Activities Score instrument and by Conselho Federal de Enfermagem (COFEN) resolution no. 527/16, in the two hospital stays, and the results were compared.
The nursing workload in the first hospital stay (14.6 hours) was higher than the nursing workload in the second stay (9.9 hours) (p < 0.001). The Nursing Activities Score revealed that according to the nursing hours, the nursing staff size corresponded to 26 and 18 professionals in the first and second hospital stays, respectively, and to 15 professionals according to COFEN resolution no. 527/16.
The number of personnel responsible for promoting self-care in pediatric semi-intensive care units, according to the nursing hours suggested by the Nursing Activities Score, was higher than that recommended by the existing legislation. This demonstrates the necessity of reconsidering staff size for this healthcare profile.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):293-302
DOI 10.5935/0103-507X.20170055
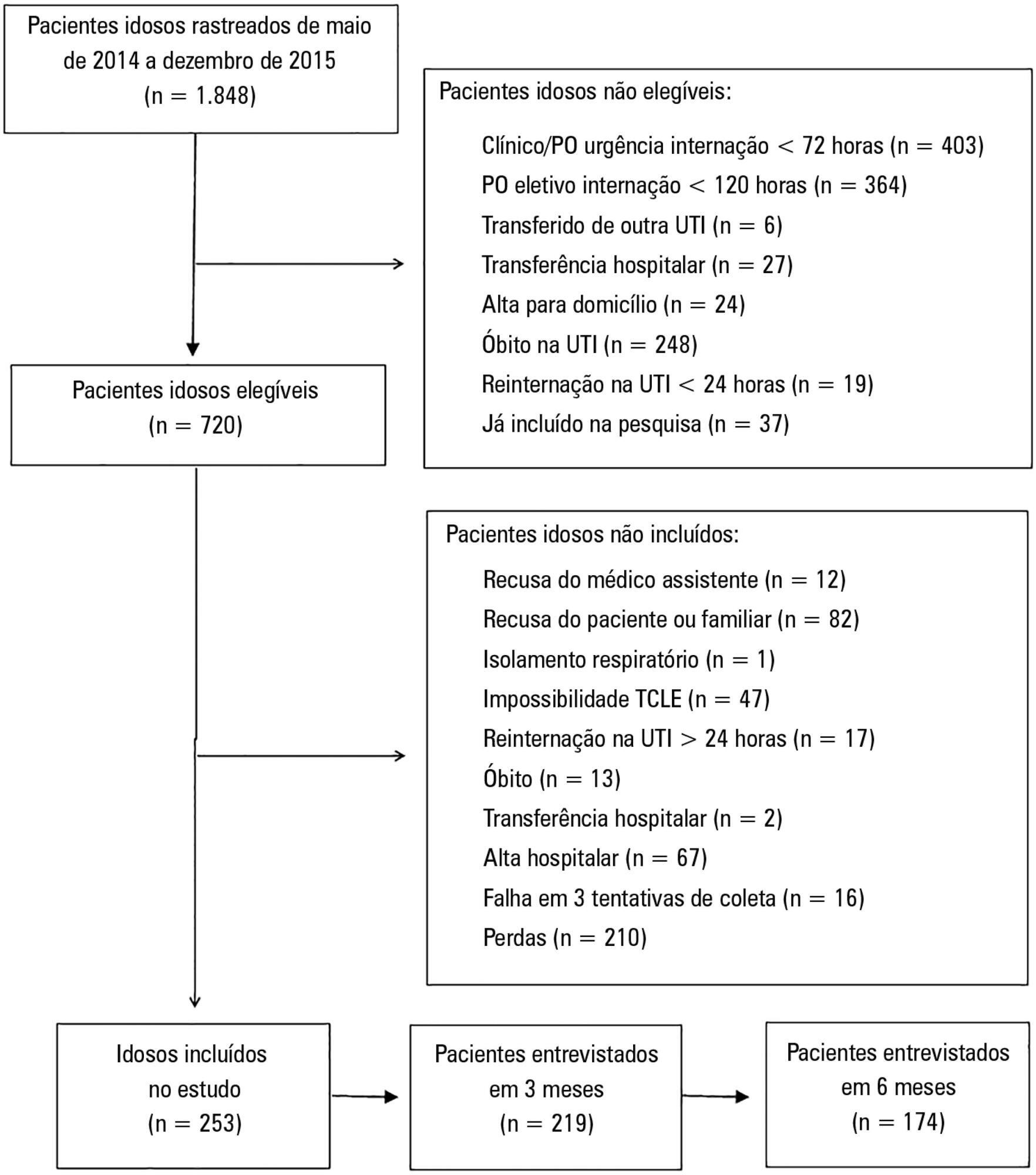
To compare the functional capacity of younger elderly individuals (60 to 79 years old) with that of older elderly individuals (≥ 80 years old) during the first 6 months after discharge from the intensive care unit.
A multicenter prospective cohort study was conducted, in which data on intensive care unit admission and outcomes after hospital discharge (immediate post-discharge, after 3 months and after 6 months) were collected. Muscle strength was evaluated through the protocol of the Medical Research Council and dynamometry (handgrip); the ability to perform activities of daily life and functional independence were assessed by the Barthel index and the usual level of physical activity (International Physical Activity Questionnaire); and quality of life was assessed by the 12-Item Short-Form Health Survey Version 2.
Among the 253 patients included, 167 were younger elderly (between 61 and 79 years old), and 86 were older elderly (≥ 80 years old). During the sixth month of evaluation, the older elderlies presented a higher need for a caregiver (69.0% versus 49, 5%, p = 0.002). Functional capacity prior to intensive care unit admission and in the third month after discharge was lower in older elderlies than in younger ones (Barthel prior to the intensive care unit: 73.0 ± 30.0 versus 86.5 ± 22.6; p <0.001, Barthel in the third month: 63.5 ± 34.0 versus 71.5 ± 35.5, p = 0.03), as was the usual level of physical activity (International Physical Activity Questionnaire in the third month: active/very active 3.4% versus 18.3%, no physical activity 64.4% versus 39.7%, p < 0.001, and International Physical Activity Questionnaire in the sixth month: active/very active 5.8% versus 20.8%, no physical activity 69.2% versus 43.4%, p = 0.005). Older elderlies had lower muscle strength when assessed according to handgrip in both the dominant (14.5 ± 7.7 versus 19.9 ± 9.6, p = 0.008) and non-dominant limb (13.1 ± 6.7 versus 17.5 ± 9.1, p = 0.02). There were no differences in functional capacity loss or reported quality of life between the age groups.
Although there were great functional capacity losses after discharge from the intensive care unit in both age groups, there was no difference in the magnitude of functional capacity loss between younger (60 to 79 years) and older elderly individuals (≥ 80 years old) during the first 6 months after discharge from the intensive care unit.