Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
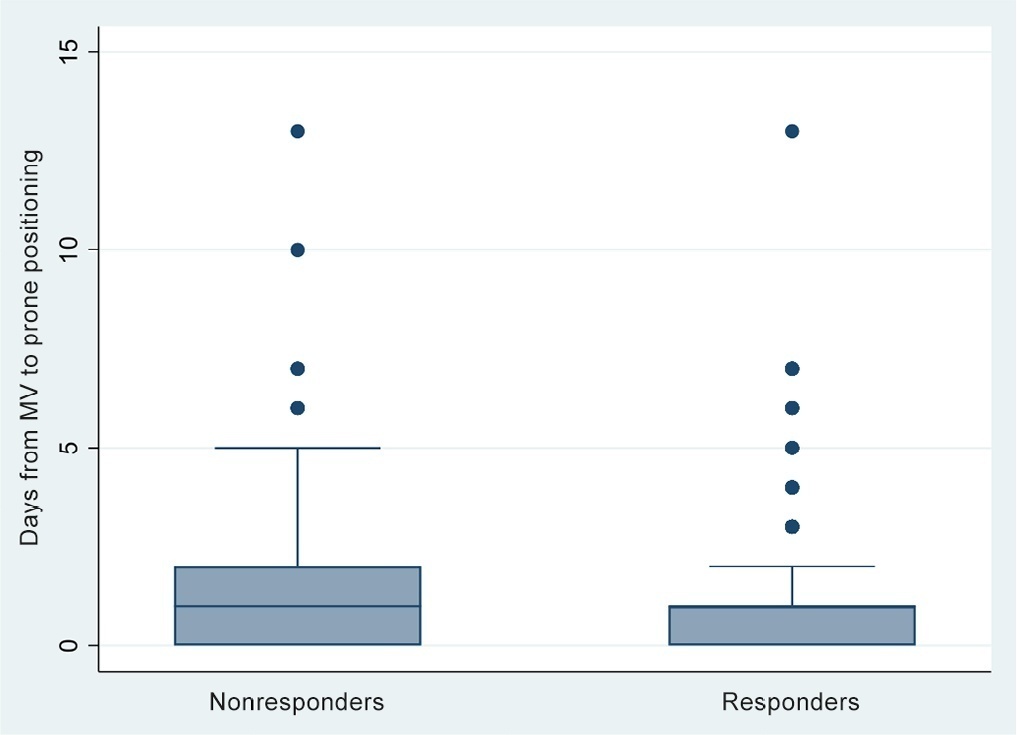
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Abstract
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
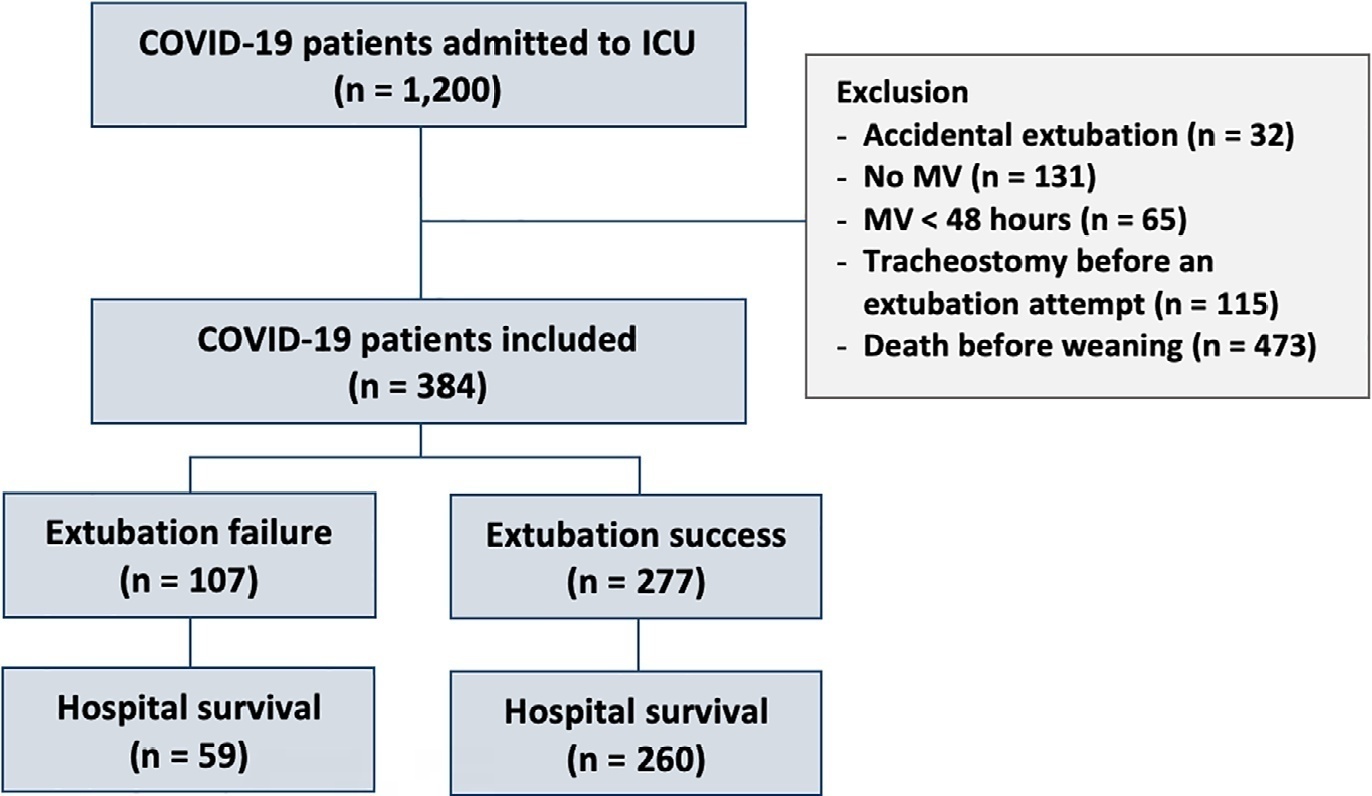
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Abstract
Crit Care Sci. 2023;35(2):168-176
DOI 10.5935/2965-2774.20230410-pt
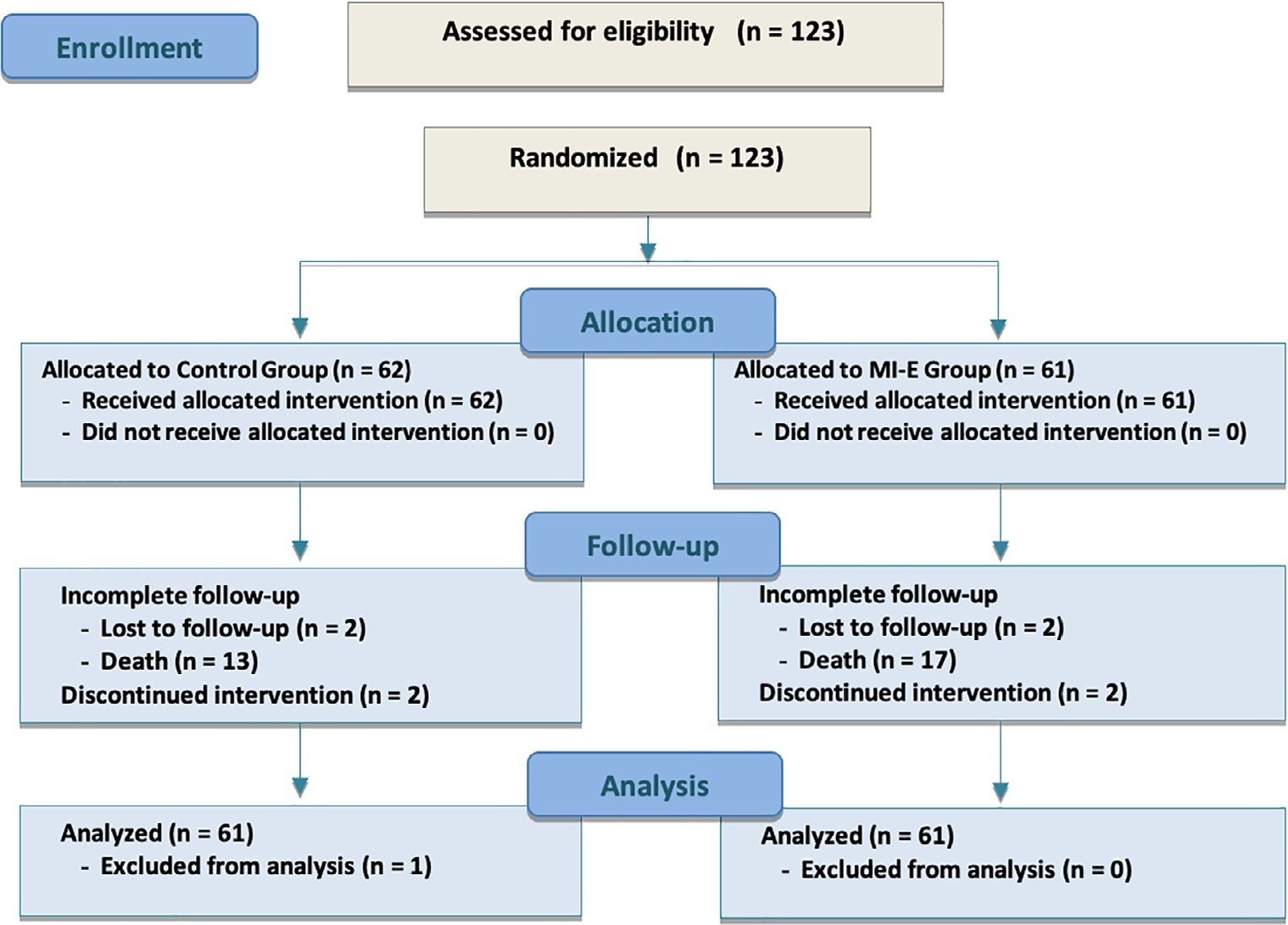
We hypothesized that the use of mechanical insufflation-exsufflation can reduce the incidence of acute respiratory failure within the 48-hour post-extubation period in intensive care unit-acquired weakness patients.
This was a prospective randomized controlled open-label trial. Patients diagnosed with intensive care unit-acquired weakness were consecutively enrolled based on a Medical Research Council score ≤ 48/60. The patients randomly received two daily sessions; in the control group, conventional chest physiotherapy was performed, while in the intervention group, chest physiotherapy was associated with mechanical insufflation-exsufflation. The incidence of acute respiratory failure within 48 hours of extubation was evaluated. Similarly, the reintubation rate, intensive care unit length of stay, mortality at 28 days, and survival probability at 90 days were assessed. The study was stopped after futility results in the interim analysis.
We included 122 consecutive patients (n = 61 per group). There was no significant difference in the incidence of acute respiratory failure between treatments (11.5% control group versus 16.4%, intervention group; p = 0.60), the need for reintubation (3.6% versus 10.7%; p = 0.27), mean length of stay (3 versus 4 days; p = 0.33), mortality at Day 28 (9.8% versus 15.0%; p = 0.42), or survival probability at Day 90 (21.3% versus 28.3%; p = 0.41).
Mechanical insufflation-exsufflation combined with chest physiotherapy seems to have no impact in preventing postextubation acute respiratory failure in intensive care unit-acquired weakness patients. Similarly, mortality and survival probability were similar in both groups. Nevertheless, given the early termination of the trial, further clinical investigation is strongly recommended.
Abstract
Crit Care Sci. 2023;35(2):177-186
DOI 10.5935/2965-2774.20230348-pt
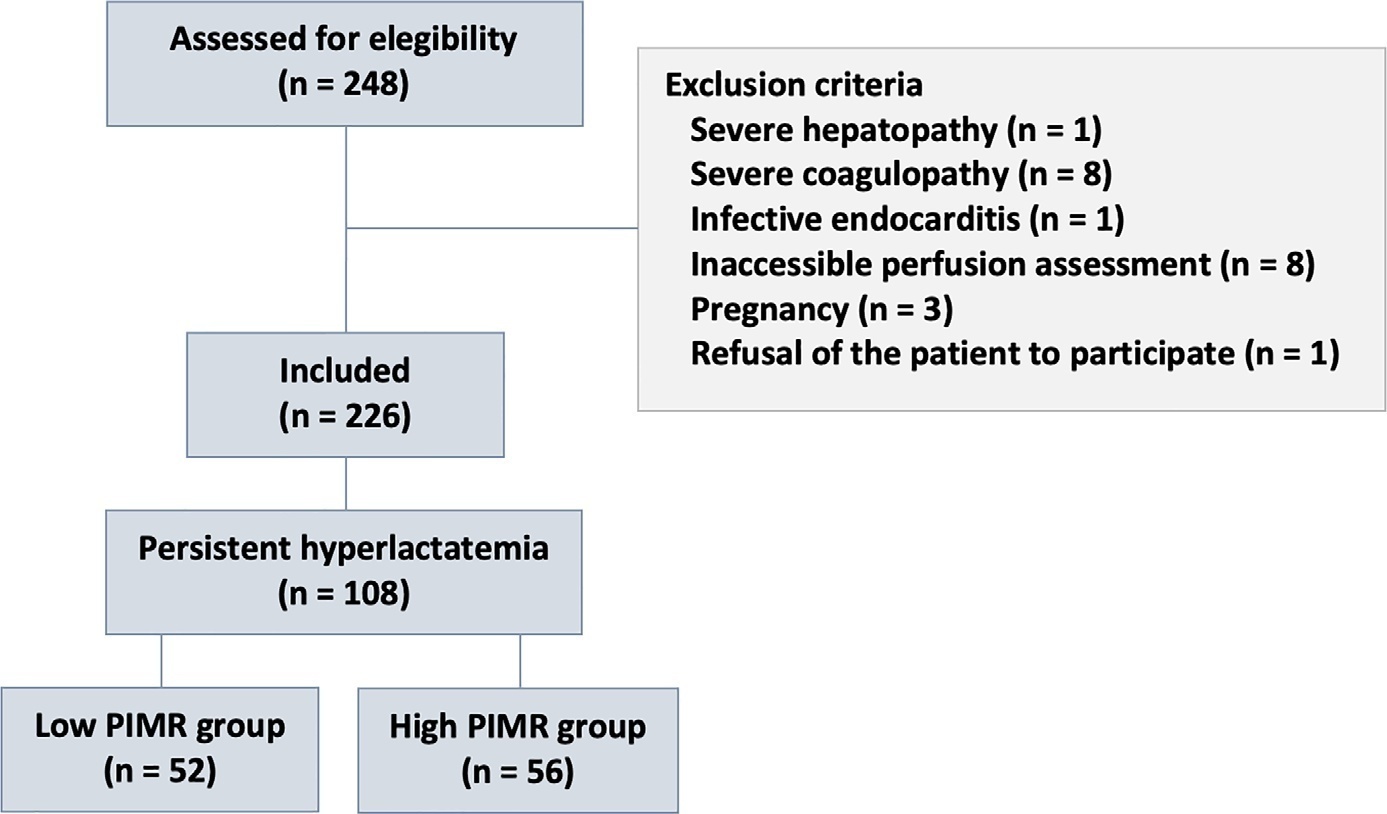
To measure the prognostic value of peripheral ischemic microvascular reserve in the context of persistent sepsis-induced hyperlactatemia and measure its influence on the temporal dynamics of lactate and the strength of association between these variables.
This post hoc analysis of the peripheral perfusion index/postocclusive reactive hyperemia trial, an observational cohort study that enrolled patients with sepsis who persisted with lactate levels ≥ 2mmol/L after fluid resuscitation (with or without shock). Peripheral ischemic microvascular reserve was evaluated using the association of the peripheral perfusion index and postocclusive reactive hyperemia techniques. The cutoff point of ∆ peripheral perfusion index peak values (%) defined the groups with low (≤ 62%) and high peripheral ischemic microvascular reserve (> 62%).
A total of 108 consecutive patients with persistent sepsis-induced hyperlactatemia were studied. The high peripheral ischemic microvascular reserve group showed higher 28-day mortality than the low peripheral ischemic microvascular reserve group (p < 0.01). The temporal dynamics of lactate within the first 48 hours showed a rapid decrease in lactate levels in the low peripheral ischemic microvascular reserve group (p < 0.01). However, this result was not reproduced in the linear mixed effects model. A weak correlation between peripheral ischemic microvascular reserve (%) and lactate level (mmol/L) was observed within the first 24 hours (r = 0.23; p < 0.05).
The prognostic value of high peripheral ischemic microvascular reserve was confirmed in the context of persistent sepsis-induced hyperlactatemia. Although there was a weak positive correlation between peripheral ischemic microvascular reserve value and lactate level within the first 24 hours of sepsis diagnosis, the low peripheral ischemic microvascular reserve group appeared to have a faster decrease in lactate over the 48 hours of follow-up.
Abstract
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
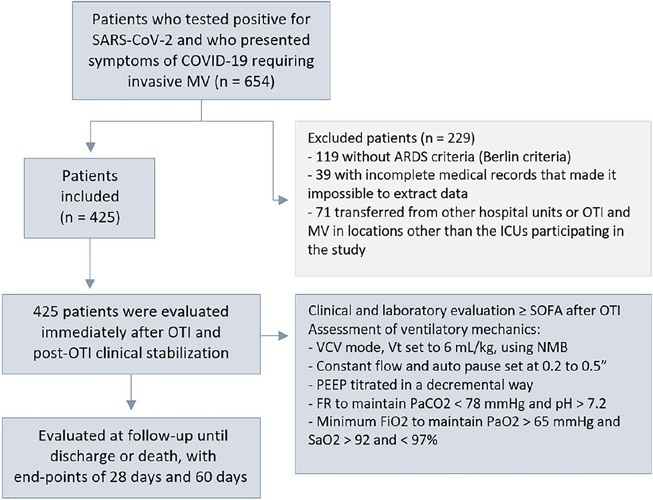
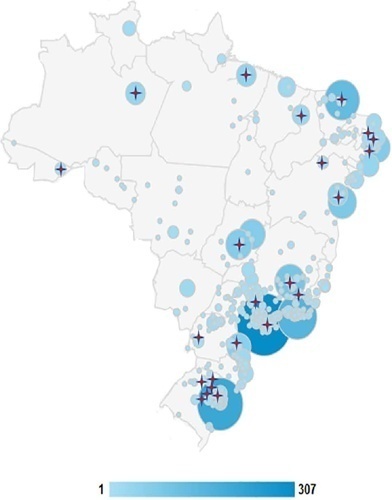
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Body mass index (RR 1.17; 95%CI 1.11 - 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Abstract
Crit Care Sci. 2023;35(1):31-36
DOI 10.5935/2965-2774.20230113-pt
To evaluate the impact of an educational website on satisfaction and symptoms of anxiety and depression among family members of critically ill adult patients.
We embedded an analysis of website access in a cohort study conducted in intensive care units with flexible visiting hours in Brazil. Family members were guided to access an educational website designed to help them understand the processes and emotions associated with an intensive care unit stay. Subjects were evaluated for baseline data within the first 48 hours following enrollment and outcome assessment at up to 7 days after patient discharge from the intensive care unit, death, or until the 30th day of the study. The main outcomes were satisfaction using the Critical Care Family Needs Inventory and the presence of anxiety and depression symptoms using the Hospital Anxiety and Depression Scale.
A total of 532 family members were evaluated during the study period. Of these, 61 (11.5%) accessed the website. After adjustments, family members who accessed the website had significantly better mean Critical Care Family Needs Inventory scores (152.8 versus 145.2, p = 0.01) and a lower prevalence of probable clinical anxiety (prevalence ratio 0.35; 95%CI 0.14 - 0.89) than family members who did not access the website. There were no differences regarding symptoms of depression.
Access to an educational website was associated with higher family satisfaction with care and a lower prevalence of clinical anxiety.
Abstract
Crit Care Sci. 2023;35(1):37-43
DOI 10.5935/2965-2774.20230275-pt
To compare the diagnostic performance of maximal expiratory pressure with maximal expiratory pressure during induced cough for predicting extubation failure within 72 hours in patients who completed a spontaneous breathing trial (SBT).
The study was conducted between October 2018 and September 2019. All patients aged over 18 years admitted to the intensive care unit who required invasive mechanical ventilation for over 48 hours and successfully completed a spontaneous breathing trial were included. The maximal expiratory pressure was assessed with a unidirectional valve for 40 seconds, and verbal encouragement was given. The maximal expiratory pressure during induced cough was measured with slow instillation of 2mL of a 0.9% saline solution. The primary outcome variable was extubation failure.
Eighty patients were included, of which 43 (54%) were male. Twenty-two patients [27.5% (95%CI 18.9 - 38.1)] failed extubation within 72 hours. Differences were observed in the maximal expiratory pressure during induced cough between the group who failed extubation, with a median of 0cmH2O (P25-75: 0 - 90), and the group without extubation failure, with a median of 120cmH2O (P25-75: 73 - 120); p < 0.001.
In patients who completed a spontaneous breathing trial, the maximal expiratory pressure during induced cough had a higher diagnostic performance for predicting extubation failure within 72 hours.

Abstract
Crit Care Sci. 2023;35(1):44-56
DOI 10.5935/2965-2774.20230340-pt
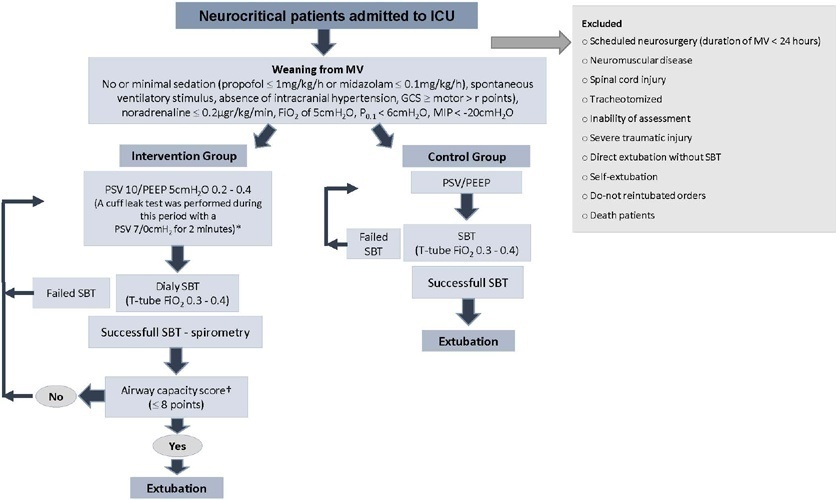
To investigate whether protocol-directed weaning in neurocritical patients would reduce the rate of extubation failure (as a primary outcome) and the associated complications (as a secondary outcome) compared with conventional weaning.
A quasi-experimental study was conducted in a medical-surgical intensive care unit from January 2016 to December 2018. Patients aged 18 years or older with an acute neurological disease who were on mechanical ventilation > 24 hours were included. All patients included in the study were ready to wean, with no or minimal sedation, Glasgow coma score ≥ 9, spontaneous ventilatory stimulus, noradrenaline ≤ 0.2μgr/kg/ minute, fraction of inspired oxygen ≤ 0.5, positive end-expiratory pressure ≤ 5cmH2O, maximal inspiratory pressure < -20cmH2O, and occlusion pressure < 6cmH2O.
Ninety-four of 314 patients admitted to the intensive care unit were included (50 in the Intervention Group and 44 in the Control Group). There was no significant difference in spontaneous breathing trial failure (18% in the Intervention Group versus 34% in the Control Group, p = 0.12). More patients in the Intervention Group were extubated than in the Control Group (100% versus 79%, p = 0.01). The rate of extubation failure was not signifiantly diffrent between the groups (18% in the Intervention Group versus 17% in the Control Group; relative risk 1.02; 95%CI 0.64 - 1.61; p = 1.00). The reintubation rate was lower in the Control Group (16% in the Intervention Group versus 11% in the Control Group; relative risk 1.15; 95%CI 0.74 - 1.82; p = 0.75). The need for tracheotomy was lower in the Intervention Group [4 (8%) versus 11 (25%) in the Control Group; relative risk 0.32; 95%CI 0.11 - 0.93; p = 0.04]. At Day 28, the patients in the Intervention Group had more ventilator-free days than those in the Control Group [28 (26 - 28) days versus 26 (19 - 28) days; p = 0.01]. The total duration of mechanical ventilation was shorter in the Intervention Group than in the Control Group [5 (2 - 13) days versus 9 (3 - 22) days; p = 0.01]. There were no diffrences in the length of intensive care unit stay, 28-day free from mechanical ventilation, hospital stay or 90-day mortality.
Considering the limitations of our study, the application of a weaning protocol for neurocritical patients led to a high percentage of extubation, a reduced need for tracheotomy and a shortened duration of mechanical ventilation. However, there was no reduction in extubation failure or the 28-day free of from mechanical ventilation compared with the Control Group.