Abstract
Rev Bras Ter Intensiva. 2018;30(2):187-194
DOI 10.5935/0103-507X.20180037
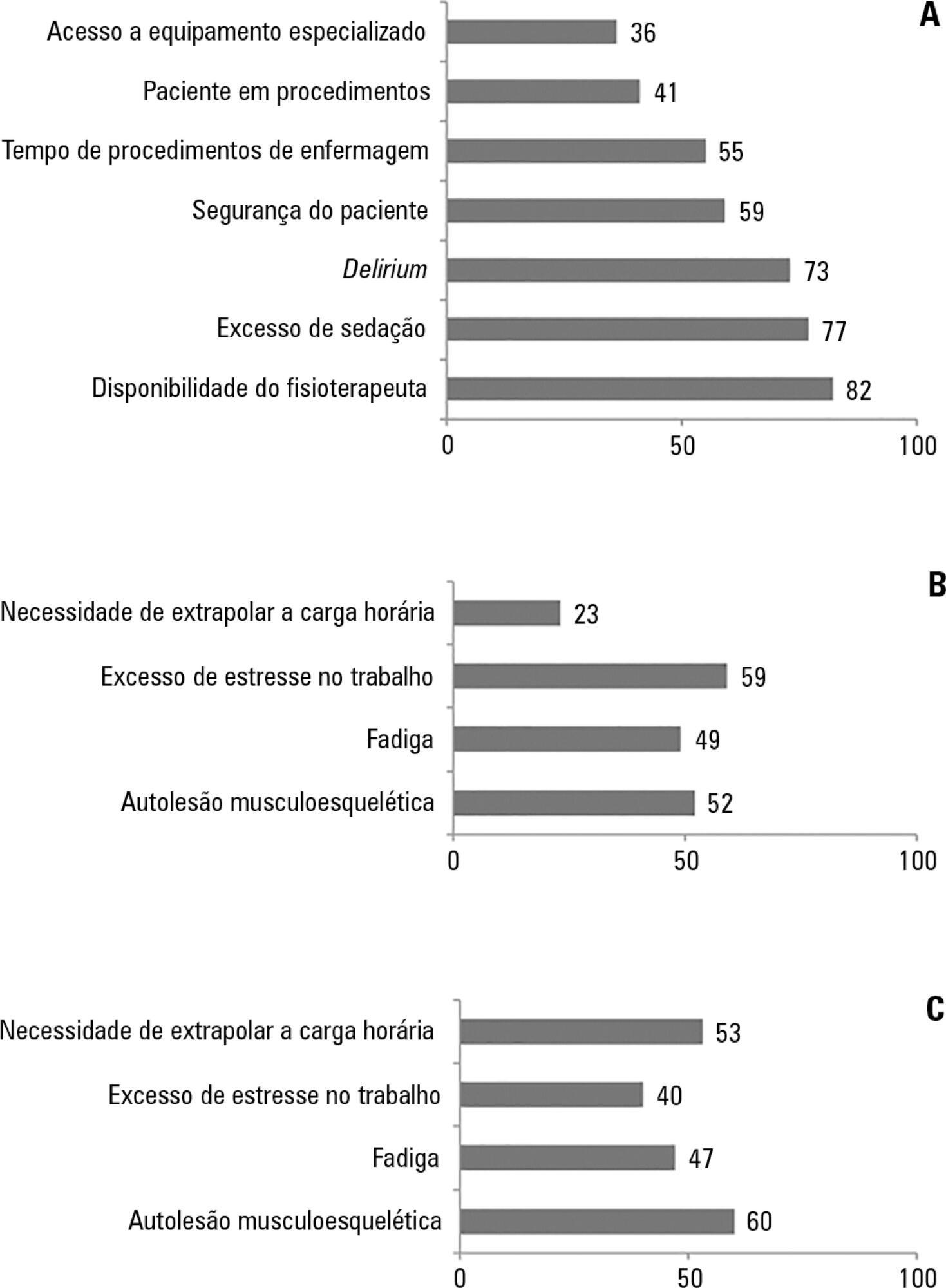
To investigate the knowledge of multi-professional staff members about the early mobilization of critically ill adult patients and identify attitudes and perceived barriers to its application.
A cross-sectional study was conducted during the second semester of 2016 with physicians, nursing professionals and physical therapists from six intensive care units at two teaching hospitals. Questions were answered on a 5-point Likert scale and analyzed as proportions of professionals who agreed or disagreed with statements. The chi-square and Fisher's exact tests were used to investigate differences in the responses according to educational/training level, previous experience with early mobilization and years of experience in intensive care units.
The questionnaire was answered by 98 out of 514 professionals (response rate: 19%). The acknowledged benefits of early mobilization were maintenance of muscle strength (53%) and shortened length of mechanical ventilation (83%). Favorable attitudes toward early mobilization included recognition that its benefits for patients under mechanical ventilation exceed the risks for both patients and staff, that early mobilization should be routinely performed via nursing and physical therapy protocols, and readiness to change the parameters of mechanical ventilation and reduce sedation to facilitate the early mobilization of patients. The main barriers mentioned were the unavailability of professionals and time to mobilize patients, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
The participants were aware of the benefits of early mobilization and manifested attitudes favorable to its application. However, the actual performance of early mobilization was perceived as a challenge, mainly due to the lack of professionals and time, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):427-435
DOI 10.5935/0103-507X.20170067
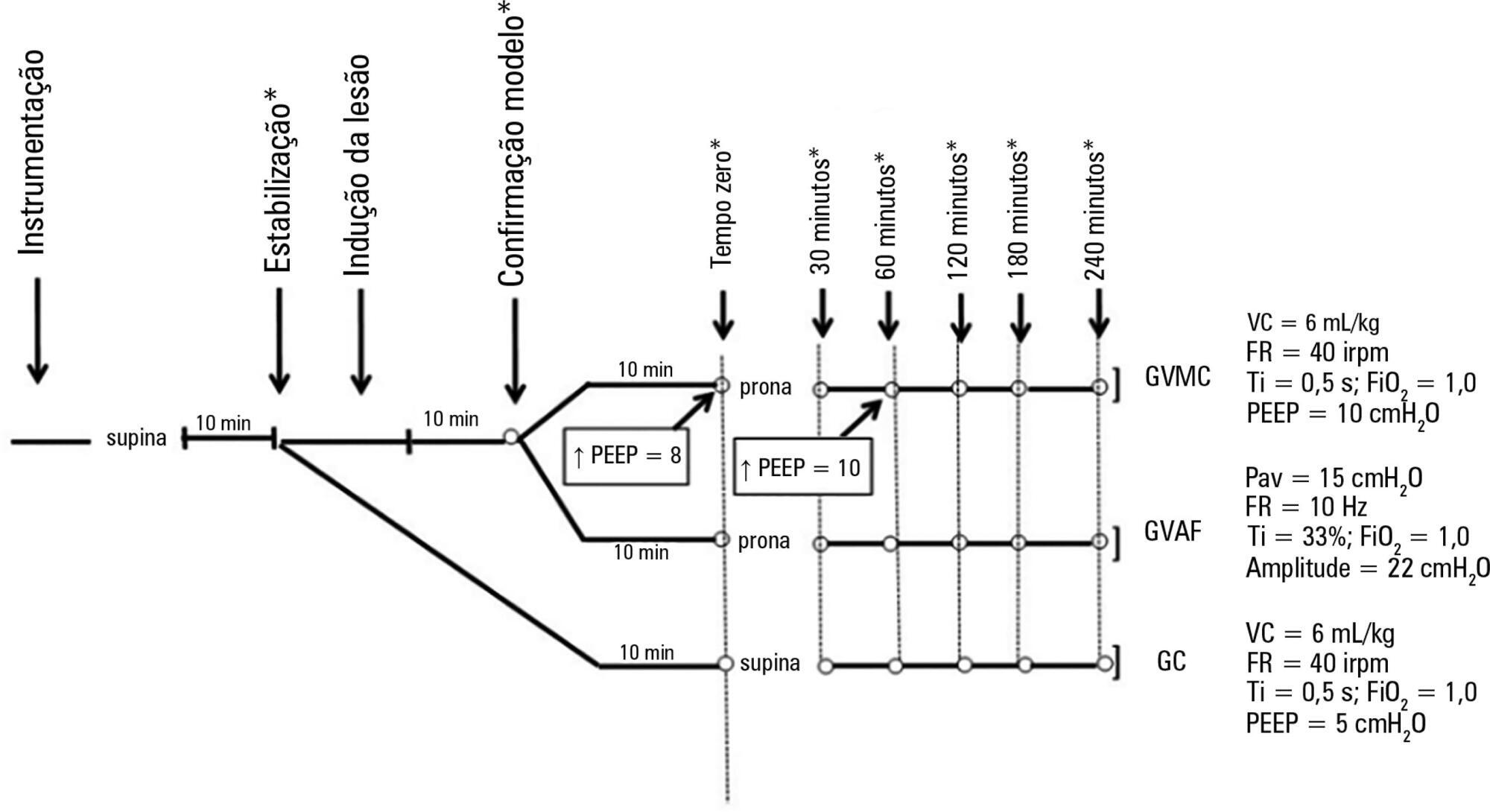
To compare the effects of high-frequency oscillatory ventilation and conventional protective mechanical ventilation associated with the prone position on oxygenation, histology and pulmonary oxidative damage in an experimental model of acute lung injury.
Forty-five rabbits with tracheostomy and vascular access were underwent mechanical ventilation. Acute lung injury was induced by tracheal infusion of warm saline. Three experimental groups were formed: healthy animals + conventional protective mechanical ventilation, supine position (Control Group; n = 15); animals with acute lung injury + conventional protective mechanical ventilation, prone position (CMVG; n = 15); and animals with acute lung injury + high-frequency oscillatory ventilation, prone position (HFOG; n = 15). Ten minutes after the beginning of the specific ventilation of each group, arterial gasometry was collected, with this timepoint being called time zero, after which the animal was placed in prone position and remained in this position for 4 hours. Oxidative stress was evaluated by the total antioxidant performance assay. Pulmonary tissue injury was determined by histopathological score. The level of significance was 5%.
Both groups with acute lung injury showed worsening of oxygenation after induction of injury compared with the Control Group. After 4 hours, there was a significant improvement in oxygenation in the HFOG group compared with CMVG. Analysis of total antioxidant performance in plasma showed greater protection in HFOG. HFOG had a lower histopathological lesion score in lung tissue than CMVG.
High-frequency oscillatory ventilation, associated with prone position, improves oxygenation and attenuates oxidative damage and histopathological lung injury compared with conventional protective mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):466-475
DOI 10.5935/0103-507X.20170063
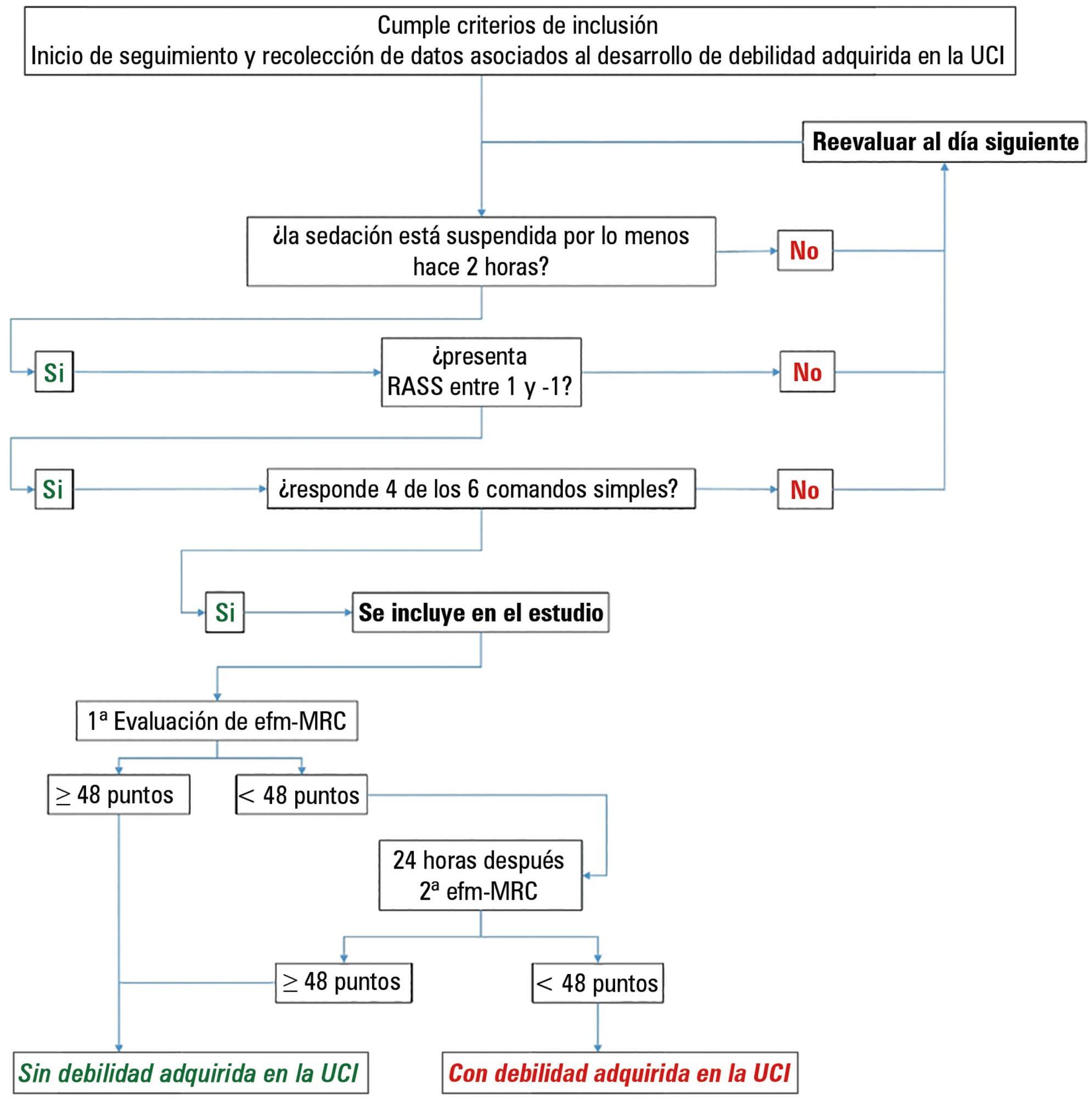
This paper sought to determine the accumulated incidence and analyze the risk factors associated with the development of weakness acquired in the intensive care unit and its relationship to inspiratory weakness.
We conducted a prospective cohort study at a single center, multipurpose medical-surgical intensive care unit. We included adult patients who required mechanical ventilation ≥ 24 hours between July 2014 and January 2016. No interventions were performed. Demographic data, clinical diagnoses, the factors related to the development of intensive care unit -acquired weakness, and maximal inspiratory pressure were recorded.
Of the 111 patients included, 66 developed intensive care unit -acquired weakness, with a cumulative incidence of 40.5% over 18 months. The group with intensive care unit-acquired weakness were older (55.9 ± 17.6 versus 45.8 ± 16.7), required more mechanical ventilation (7 [4 - 10] days versus 4 [2 - 7.3] days), and spent more time in the intensive care unit (15.5 [9.2 - 22.8] days versus 9 [6 - 14] days). More patients presented with delirium (68% versus 39%), hyperglycemia > 3 days (84% versus 59%), and positive balance > 3 days (73.3% versus 37%). All comparisons were significant at p < 0.05. A multiple logistic regression identified age, hyperglycemia ≥ 3 days, delirium, and mechanical ventilation > 5 days as independent predictors of intensive care unit-acquired weakness. Low maximal inspiratory pressure was associated with intensive care unit-acquired weakness (p < 0.001), and the maximum inspiratory pressure cut-off value of < 36cmH2O had sensitivity and specificity values of 31.8% and 95.5%, respectively, when classifying patients with intensive care unit-acquired weakness.
The intensive care unit acquired weakness is a condition with a high incidence in our environment. The development of intensive care unit-acquired weakness was associated with age, delirium, hyperglycemia, and mechanical ventilation > 5 days. The maximum inspiratory pressure value of ≥ 36cmH2O was associated with a high diagnostic value to exclude the presence of intensive care unit -acquired weakness.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):346-353
DOI 10.5935/0103-507X.20170045
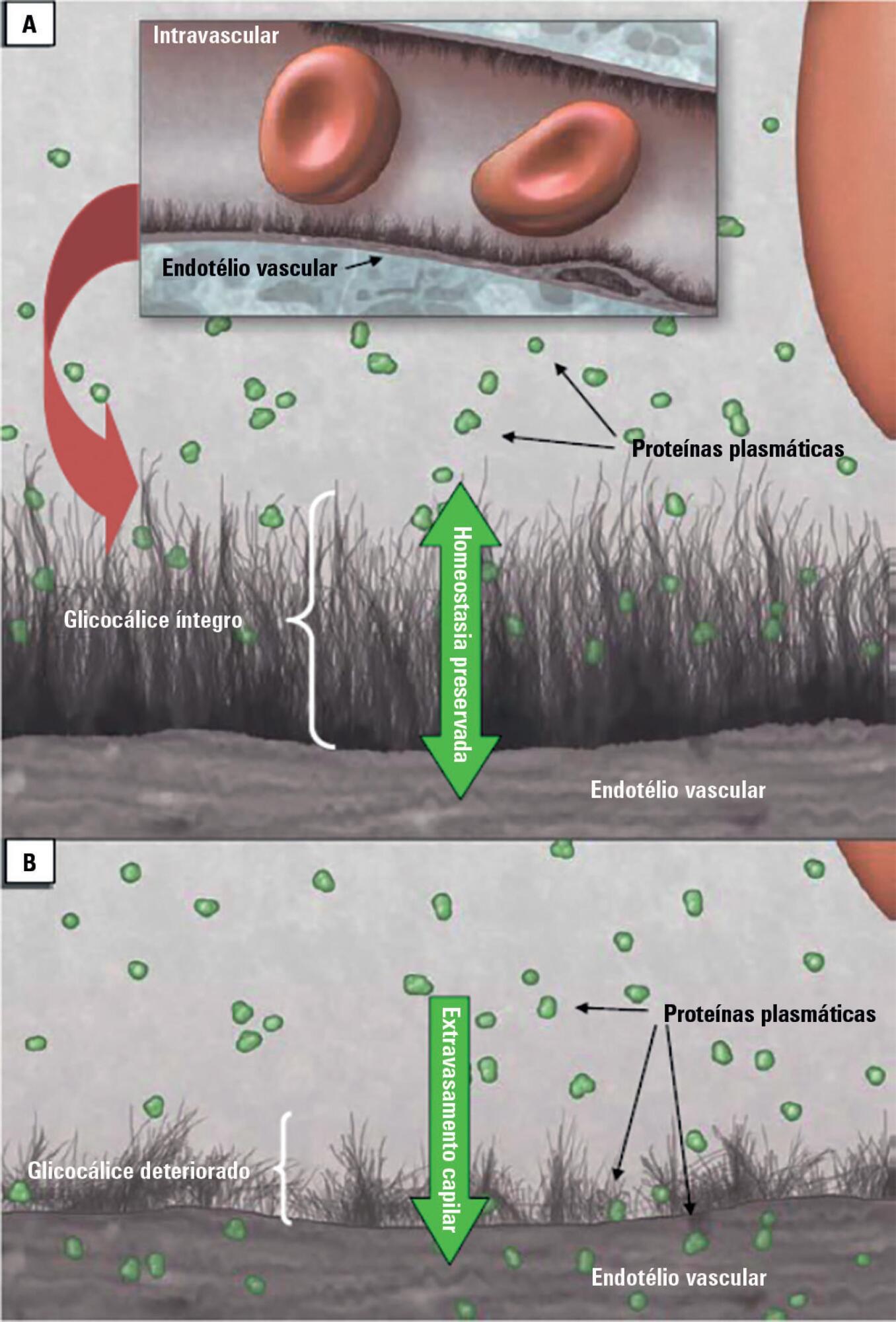
Patients admitted to an intensive care unit are prone to cumulated fluid overload and receive intravenous volumes through the aggressive resuscitation recommended for septic shock treatment, as well as other fluid sources related to medications and nutritional support. The liberal liquid supply strategy has been associated with higher morbidity and mortality. Although there are few prospective pediatric studies, new strategies are being proposed. This non-systematic review discusses the pathophysiology of fluid overload, its consequences, and the available therapeutic strategies. During systemic inflammatory response syndrome, the endothelial glycocalyx is damaged, favoring fluid extravasation and resulting in interstitial edema. Extravasation to the third space results in longer mechanical ventilation, a greater need for renal replacement therapy, and longer intensive care unit and hospital stays, among other changes. Proper hemodynamic monitoring, as well as cautious infusion of fluids, can minimize these damages. Once cumulative fluid overload is established, treatment with long-term use of loop diuretics may lead to resistance to these medications. Strategies that can reduce intensive care unit morbidity and mortality include the early use of vasopressors (norepinephrine) to improve cardiac output and renal perfusion, the use of a combination of diuretics and aminophylline to induce diuresis, and the use of sedation and early mobilization protocols.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):279-286
DOI 10.5935/0103-507X.20170038
We aimed to investigate a potential association between B-lines and weaning failure.
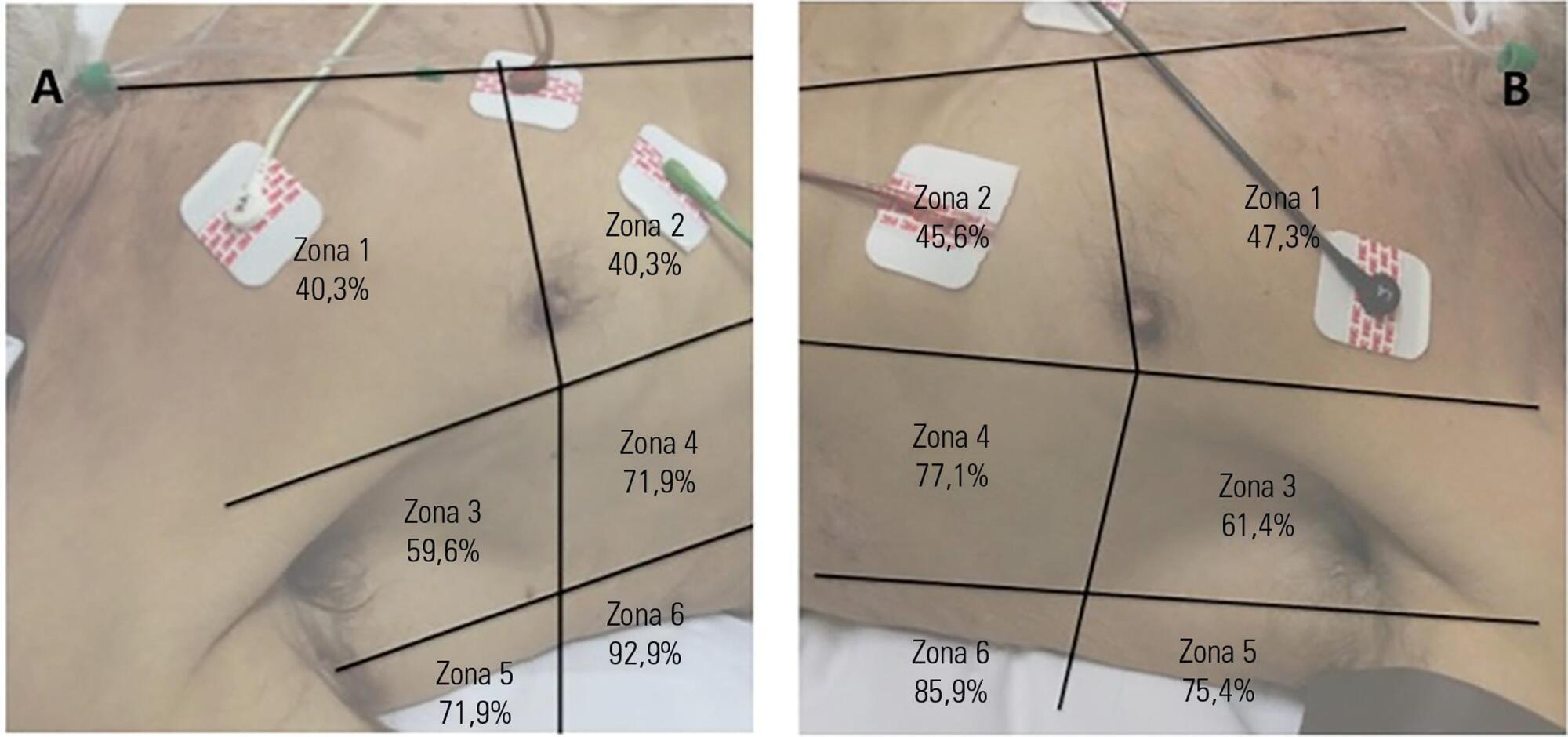
Fifty-seven subjects eligible for ventilation liberation were enrolled. Patients with tracheostomy were excluded. Lung ultrasound assessments of six thoracic zones were performed immediately before and at the exnd of the spontaneous breathing trial. B-predominance was defined as any profile with anterior bilateral B-pattern. Patients were followed up to 48 hours after extubation.
Thirty-eight individuals were successfully extubated; 11 failed the spontaneous breathing trial and 8 needed reintubation within 48 hours of extubation. At the beginning of the T-piece trial, B-pattern or consolidation was already found at the lower and posterior lung regions in more than half of the individuals and remained non-aerated at the end of the trial. A trend toward loss of lung aeration during spontaneous breathing trials was observed only in the spontaneous breathing trial-failure group (p = 0.07), and there was higher B-predominance at the end of the trial (p = 0.01).
A loss of lung aeration during the spontaneous breathing trial in non-dependent lung zones was demonstrated in subjects who failed to wean.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):23-33
DOI 10.5935/0103-507X.20170005
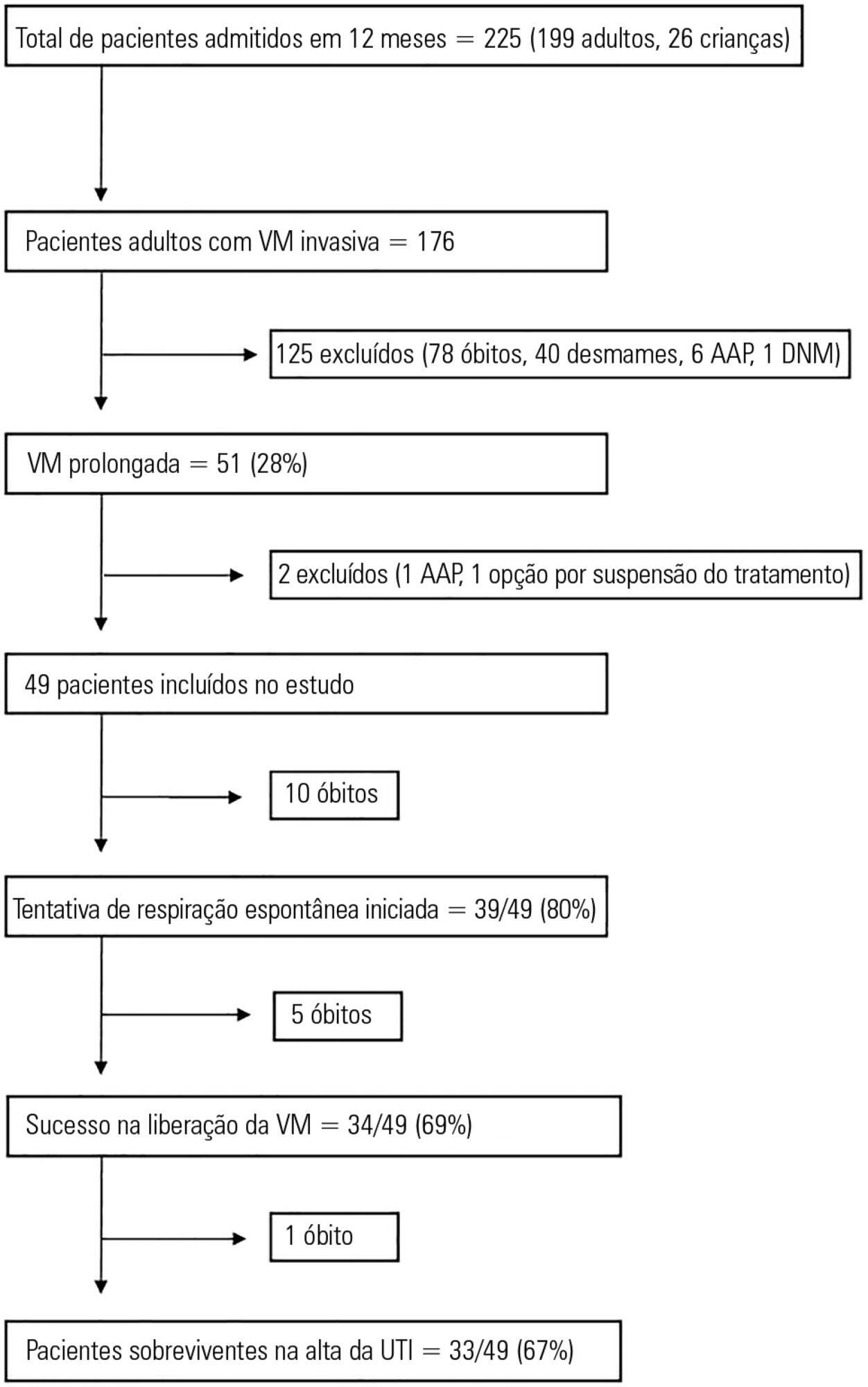
This study aimed to examine the clinical characteristics, weaning pattern, and outcome of patients requiring prolonged mechanical ventilation in acute intensive care unit settings in a resource-limited country.
This was a prospective single-center observational study in India, where all adult patients requiring prolonged ventilation were followed for weaning duration and pattern and for survival at both intensive care unit discharge and at 12 months. The definition of prolonged mechanical ventilation used was that of the National Association for Medical Direction of Respiratory Care.
During the one-year period, 49 patients with a mean age of 49.7 years had prolonged ventilation; 63% were male, and 84% had a medical illness. The median APACHE II and SOFA scores on admission were 17 and 9, respectively. The median number of ventilation days was 37. The most common reason for starting ventilation was respiratory failure secondary to sepsis (67%). Weaning was initiated in 39 (79.5%) patients, with success in 34 (87%). The median weaning duration was 14 (9.5 - 19) days, and the median length of intensive care unit stay was 39 (32 - 58.5) days. Duration of vasopressor support and need for hemodialysis were significant independent predictors of unsuccessful ventilator liberation. At the 12-month follow-up, 65% had survived.
In acute intensive care units, more than one-fourth of patients with invasive ventilation required prolonged ventilation. Successful weaning was achieved in two-thirds of patients, and most survived at the 12-month follow-up.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):39-46
DOI 10.5935/0103-507X.20170007
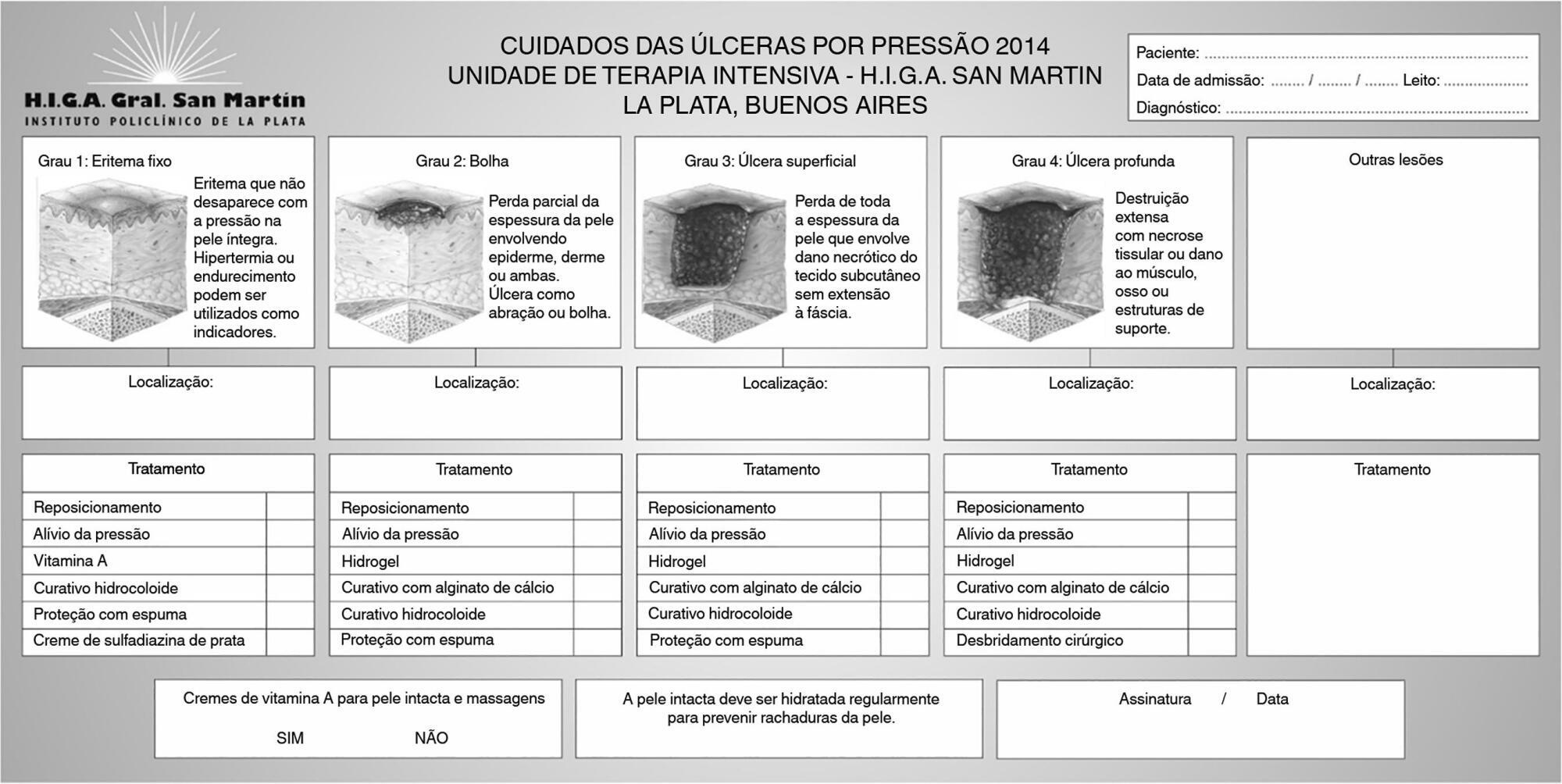
To determine the effectiveness of a quality management program in reducing the incidence and severity of pressure ulcers in critical care patients.
This was a quasi-experimental, before-and-after study that was conducted in a medical-surgical intensive care unit. Consecutive patients who had received mechanical ventilation for ≥ 96 hours were included. A "Process Improvement" team designed a multifaceted interventional process that consisted of an educational session, a pressure ulcer checklist, a smartphone application for lesion monitoring and decision-making, and a "family prevention bundle".
Fifty-five patients were included in Pre-I group, and 69 were included in the Post-I group, and the incidence of pressure ulcers in these groups was 41 (75%) and 37 (54%), respectively. The median time for pressure ulcers to develop was 4.5 [4 - 5] days in the Pre-I group and 9 [6 - 20] days in the Post-I group after admission for each period. The incidence of advanced-grade pressure ulcers was 27 (49%) in the Pre-I group and 7 (10%) in the Post-I group, and finally, the presence of pressure ulcers at discharge was 38 (69%) and 18 (26%), respectively (p < 0.05 for all comparisons). Family participation totaled 9% in the Pre-I group and increased to 57% in the Post-I group (p < 0.05). A logistic regression model was used to analyze the predictors of advanced-grade pressure ulcers. The duration of mechanical ventilation and the presence of organ failure were positively associated with the development of pressure ulcers, while the multifaceted intervention program acted as a protective factor.
A quality program based on both a smartphone application and family participation can reduce the incidence and severity of pressure ulcers in patients on prolonged acute mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):163-170
DOI 10.5935/0103-507X.20170026
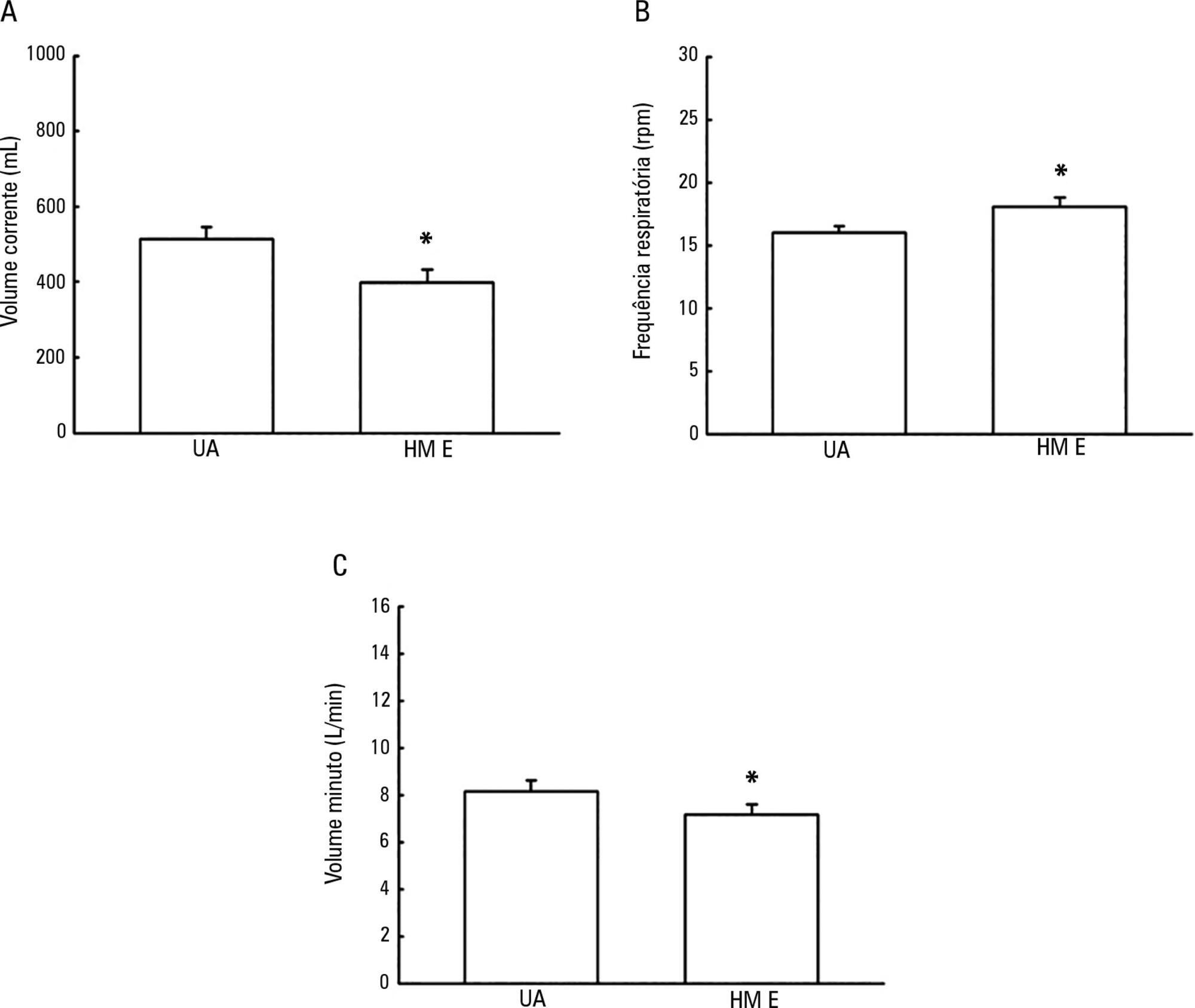
To evaluate the possible changes in tidal volume, minute volume and respiratory rate caused by the use of a heat and moisture exchanger in patients receiving pressure support mechanical ventilation and to quantify the variation in pressure support required to compensate for the effect caused by the heat and moisture exchanger.
Patients under invasive mechanical ventilation in pressure support mode were evaluated using heated humidifiers and heat and moisture exchangers. If the volume found using the heat and moisture exchangers was lower than that found with the heated humidifier, an increase in pressure support was initiated during the use of the heat and moisture exchanger until a pressure support value was obtained that enabled the patient to generate a value close to the initial tidal volume obtained with the heated humidifier. The analysis was performed by means of the paired t test, and incremental values were expressed as percentages of increase required.
A total of 26 patients were evaluated. The use of heat and moisture exchangers increased the respiratory rate and reduced the tidal and minute volumes compared with the use of the heated humidifier. Patients required a 38.13% increase in pressure support to maintain previous volumes when using the heat and moisture exchanger.
The heat and moisture exchanger changed the tidal and minute volumes and respiratory rate parameters. Pressure support was increased to compensate for these changes.