Abstract
Rev Bras Ter Intensiva. 2017;29(1):87-95
DOI 10.5935/0103-507X.20170013
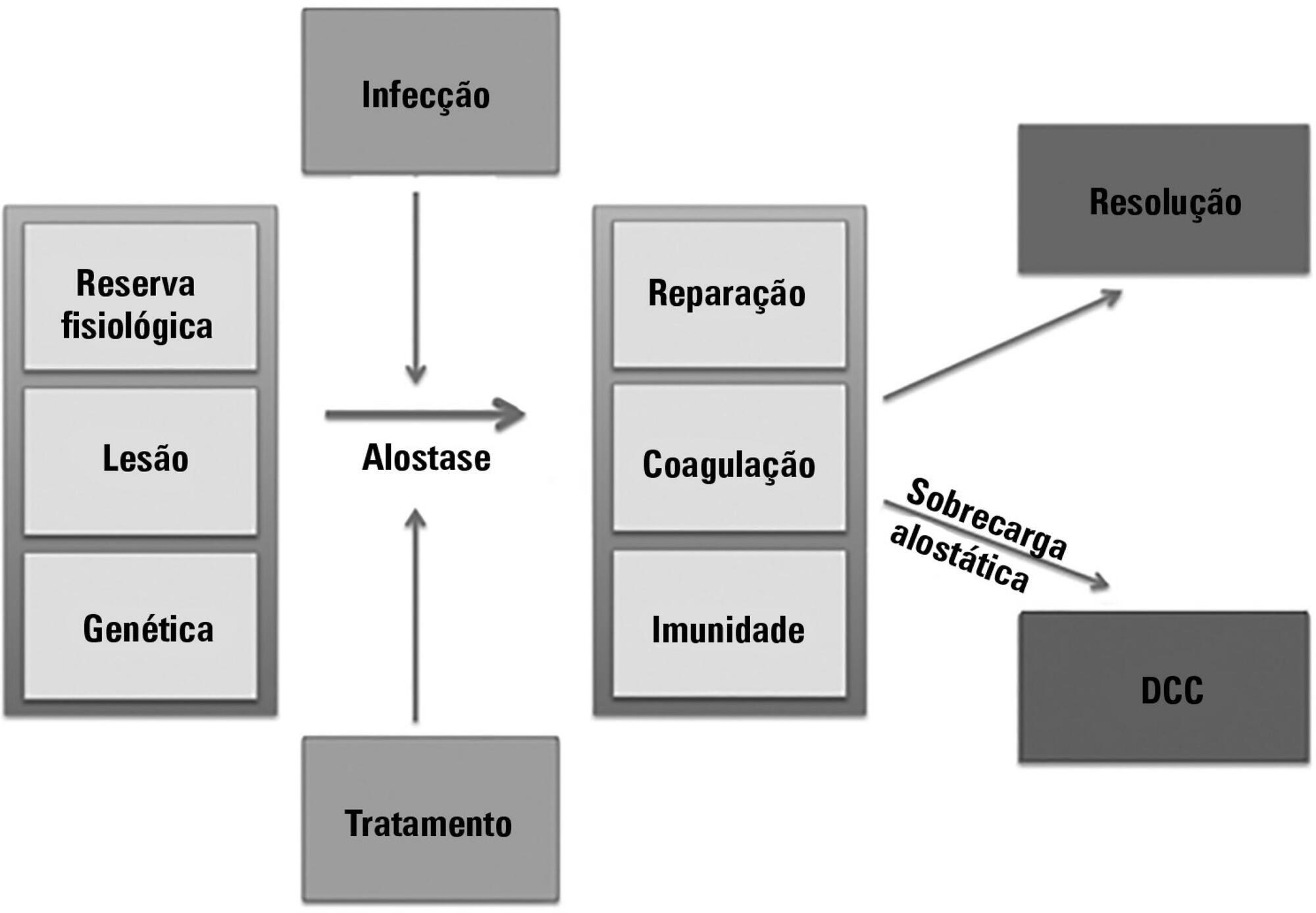
The technological advancements that allow support for organ dysfunction have led to an increase in survival rates for the most critically ill patients. Some of these patients survive the initial acute critical condition but continue to suffer from organ dysfunction and remain in an inflammatory state for long periods of time. This group of critically ill patients has been described since the 1980s and has had different diagnostic criteria over the years. These patients are known to have lengthy hospital stays, undergo significant alterations in muscle and bone metabolism, show immunodeficiency, consume substantial health resources, have reduced functional and cognitive capacity after discharge, create a sizable workload for caregivers, and present high long-term mortality rates. The aim of this review is to report on the most current evidence in terms of the definition, pathophysiology, clinical manifestations, treatment, and prognosis of persistent critical illness.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):213-221
DOI 10.5935/0103-507X.20170030
The aim of this pilot study was to evaluate the feasibility of surface electromyographic signal derived indexes for the prediction of weaning outcomes among mechanically ventilated subjects after cardiac surgery.
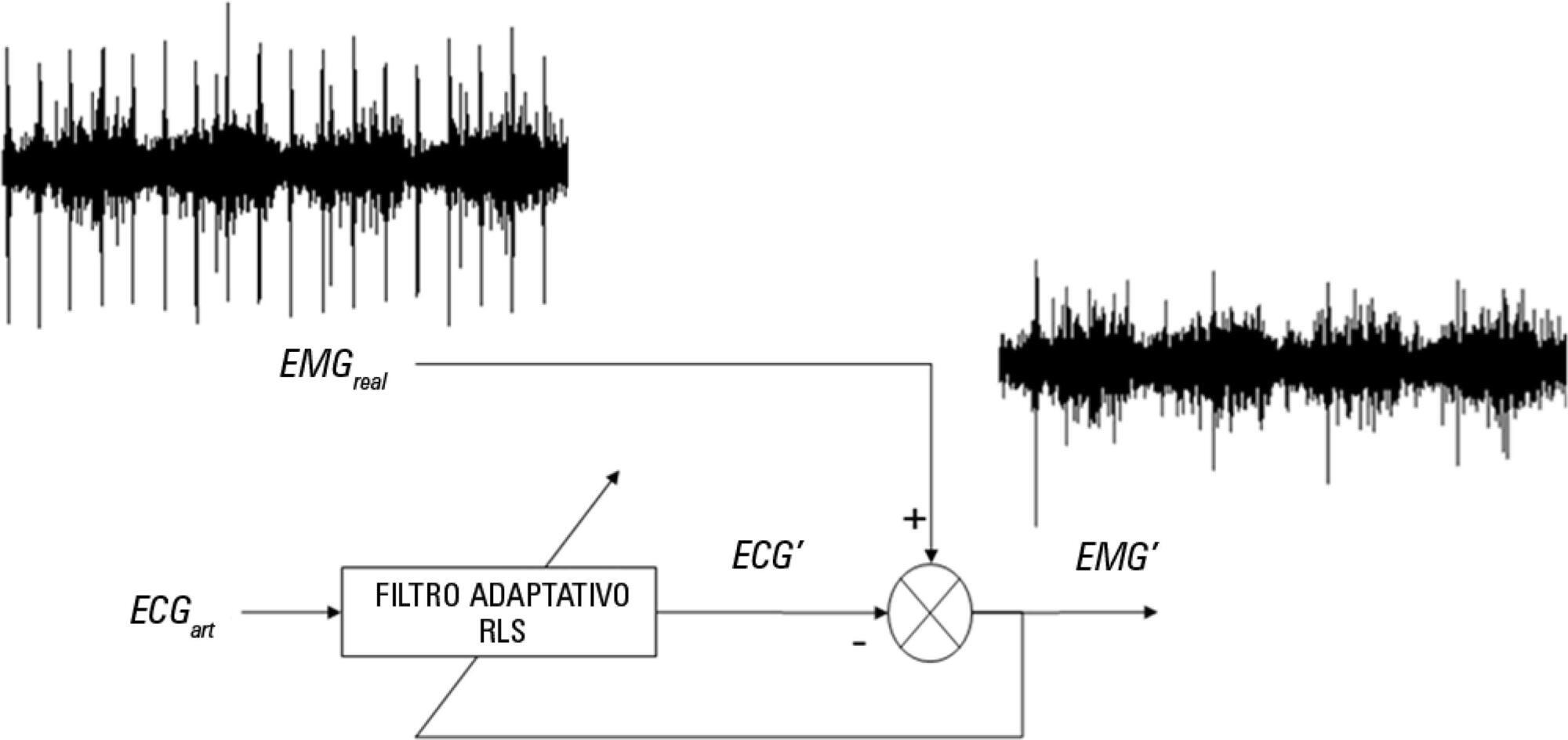
A sample of 10 postsurgical adult subjects who received cardiovascular surgery that did not meet the criteria for early extubation were included. Surface electromyographic signals from diaphragm and ventilatory variables were recorded during the weaning process, with the moment determined by the medical staff according to their expertise. Several indexes of respiratory muscle expenditure from surface electromyography using linear and non-linear processing techniques were evaluated. Two groups were compared: successfully and unsuccessfully weaned patients.
The obtained indexes allow estimation of the diaphragm activity of each subject, showing a correlation between high expenditure and weaning test failure.
Surface electromyography is becoming a promising procedure for assessing the state of mechanically ventilated patients, even in complex situations such as those that involve a patient after cardiovascular surgery.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):231-237
DOI 10.5935/0103-507X.20170032
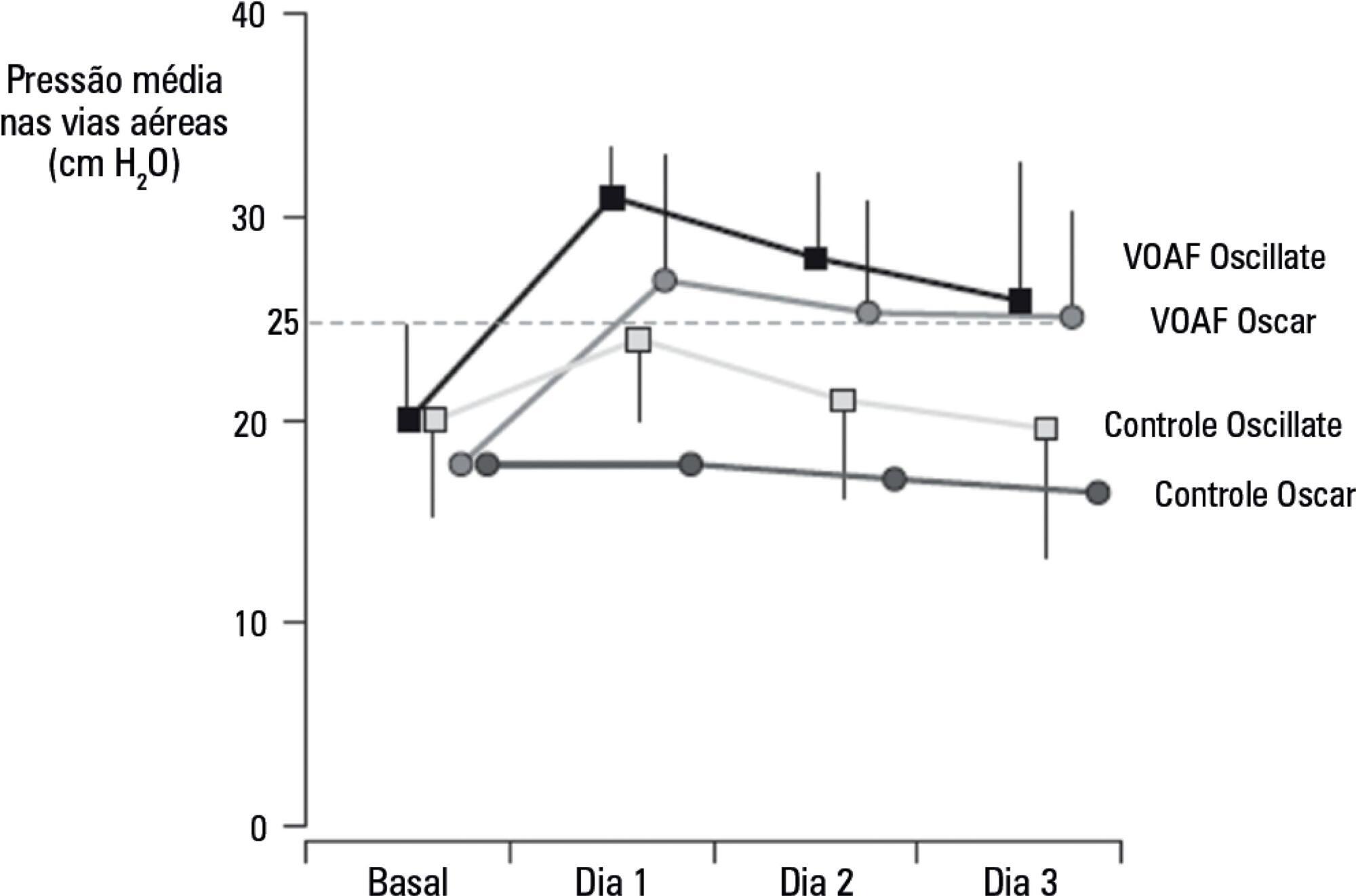
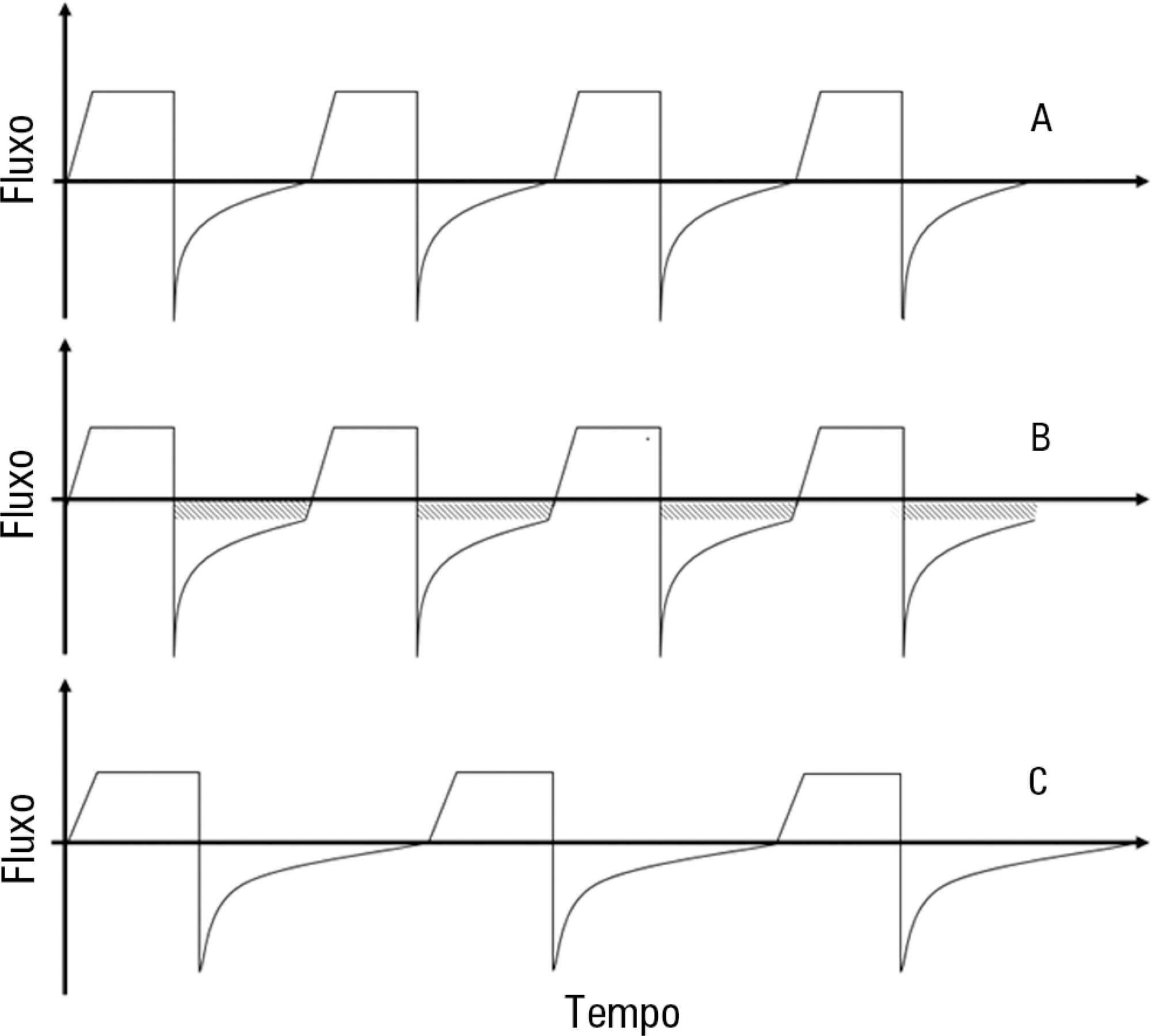
Overdistention and intratidal alveolar recruitment have been advocated as the main physical mechanisms responsible for ventilator-induced lung injury. Limiting tidal volume has a demonstrated survival benefit in patients with acute respiratory distress syndrome and is recognized as the cornerstone of protective ventilation. In contrast, the use of high positive end-expiratory pressure levels in clinical trials has yielded conflicting results and remains controversial. In the present review, we will discuss the benefits and limitations of the open lung approach and will discuss some recent experimental and clinical trials on the use of high versus low/moderate positive end-expiratory pressure levels. We will also distinguish dynamic (tidal volume) from static strain (positive end-expiratory pressure and mean airway pressure) and will discuss their roles in inducing ventilator-induced lung injury. High positive end-expiratory pressure strategies clearly decrease refractory hypoxemia in patients with acute respiratory distress syndrome, but they also increase static strain, which in turn may harm patients, especially those with lower levels of lung recruitability. In patients with severe respiratory failure, titrating positive end-expiratory pressure against the severity of hypoxemia, or providing it in a decremental fashion after a recruitment maneuver, is recommended. If high plateau, driving or mean airway pressures are observed, prone positioning or ultraprotective ventilation may be indicated to improve oxygenation without additional stress and strain in the lung.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):337-345
DOI 10.5935/0103-507X.20170058
To establish the prevalence of delirium in a general intensive care unit and to identify associated factors, clinical expression and the influence on outcomes.
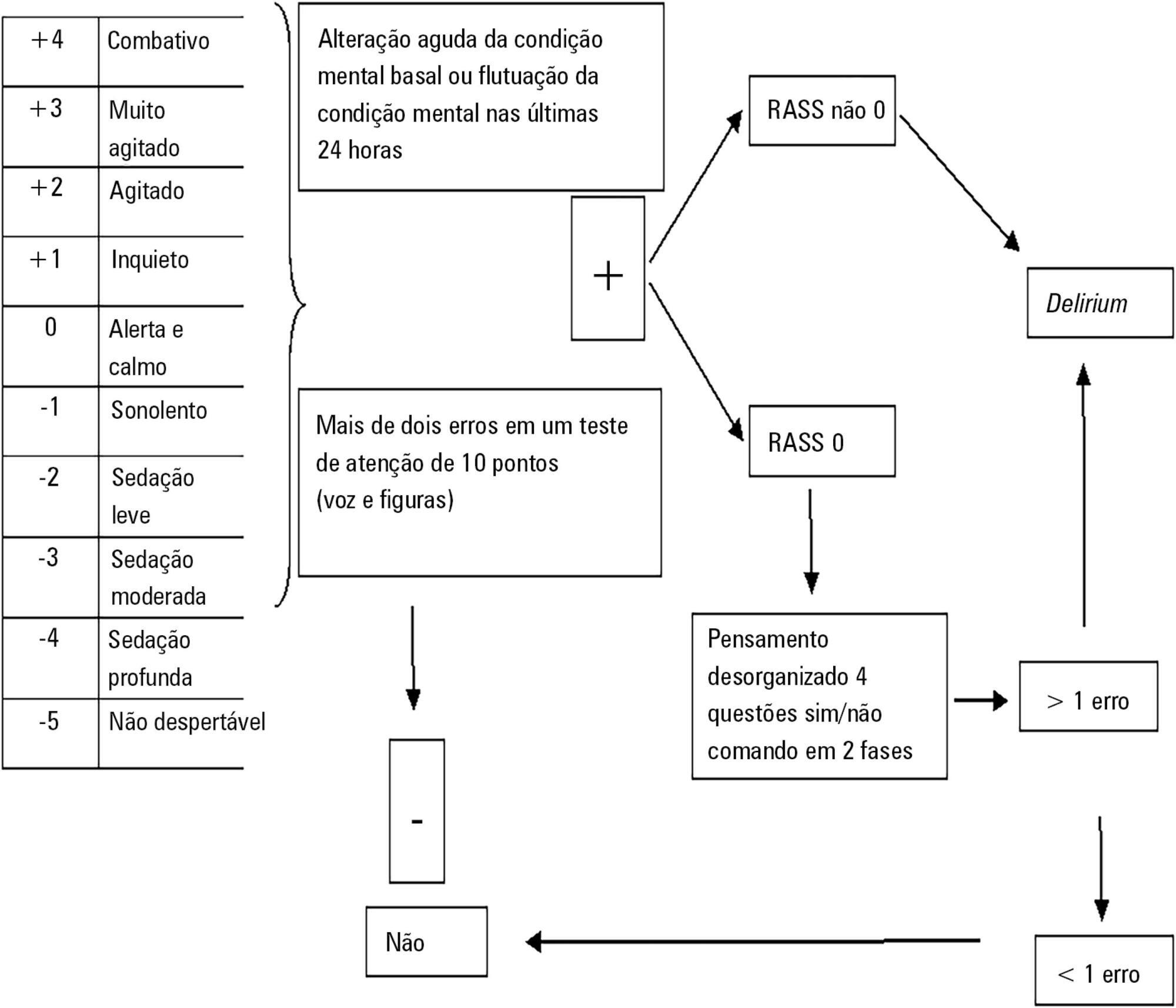
This was a prospective cohort study in a medical surgical intensive care unit. The Richmond Agitation-Sedation Scale and Confusion Assessment Method for the Intensive Care Unit were used daily to identify delirium in mechanically ventilated patients.
In this series, delirium prevalence was 80% (N = 184 delirious patients out of 230 patients). The number of patients according to delirium psychomotor subtypes was as follows: 11 hyperactive patients (6%), 9 hypoactive patients (5%) and 160 mixed patients (89%). Multiple logistic regression modeling using delirium as the dependent outcome variable (to study the risk factors for delirium) revealed that age > 65 years, history of alcohol consumption, and number of mechanical ventilation days were independent variables associated with the development of delirium. The multiple logistic regression model using hospital mortality as the dependent outcome variable (to study the risk factors for death) showed that severity of illness, according to the Acute Physiology and Chronic Health Evaluation II, mechanical ventilation for more than 7 days, and sedation days were all independent predictors for excess hospital mortality.
This Latin American prospective cohort investigation confirmed specific factors important for the development of delirium and the outcome of death among general intensive care unit patients. In both analyses, we found that the duration of mechanical ventilation was a predictor of untoward outcomes.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):509-519
DOI 10.5935/0103-507X.20170076
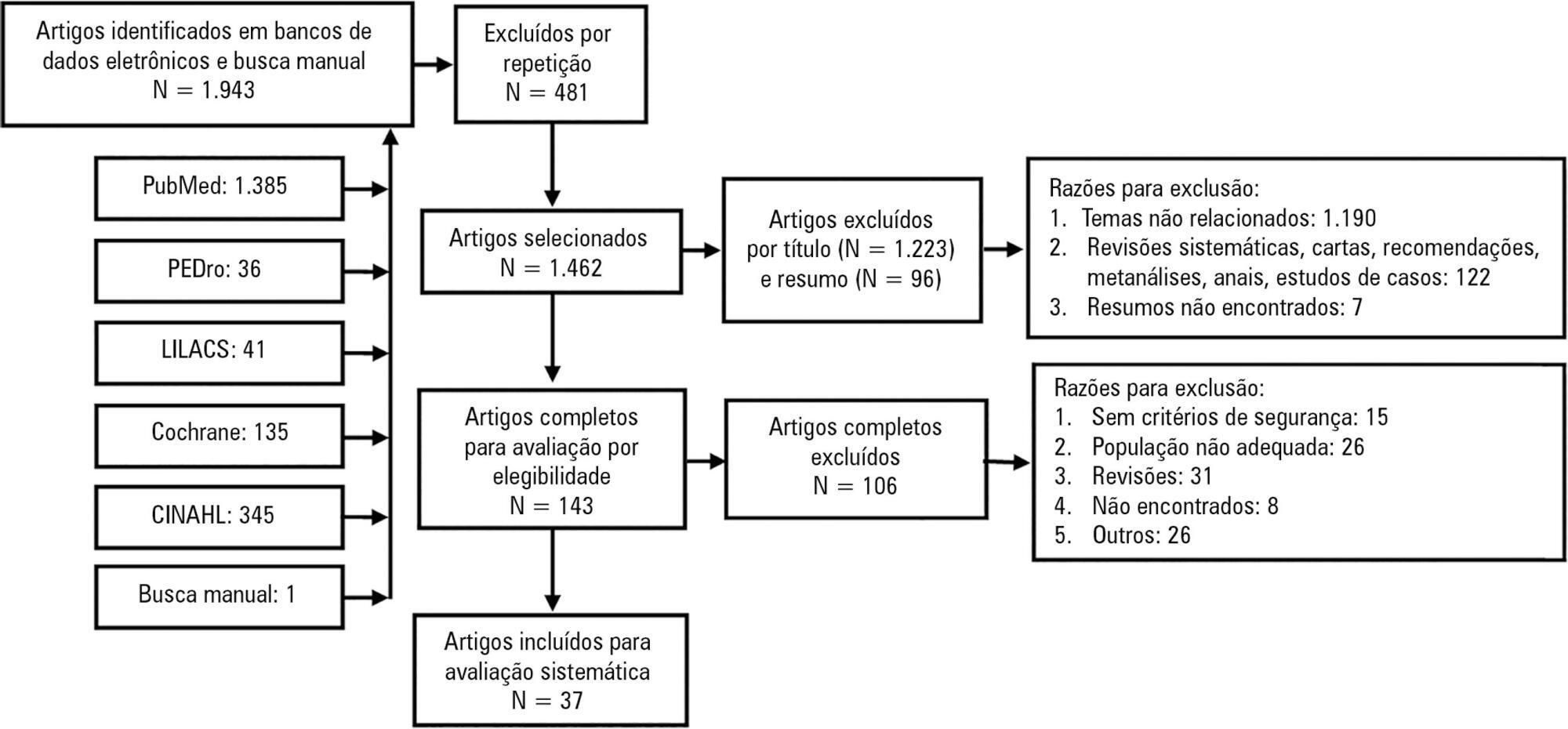
Mobilization of critically ill patients admitted to intensive care units should be performed based on safety criteria. The aim of the present review was to establish which safety criteria are most often used to start early mobilization for patients under mechanical ventilation admitted to intensive care units. Articles were searched in the PubMed, PEDro, LILACS, Cochrane and CINAHL databases; randomized and quasi-randomized clinical trials, cohort studies, comparative studies with or without simultaneous controls, case series with 10 or more consecutive cases and descriptive studies were included. The same was performed regarding prospective, retrospective or cross-sectional studies where safety criteria to start early mobilization should be described in the Methods section. Two reviewers independently selected potentially eligible studies according to the established inclusion criteria, extracted data and assessed the studies' methodological quality. Narrative description was employed in data analysis to summarize the characteristics and results of the included studies; safety criteria were categorized as follows: cardiovascular, respiratory, neurological, orthopedic and other. A total of 37 articles were considered eligible. Cardiovascular safety criteria exhibited the largest number of variables. However, respiratory safety criteria exhibited higher concordance among studies. There was greater divergence among the authors regarding neurological criteria. There is a need to reinforce the recognition of the safety criteria used to start early mobilization for critically ill patients; the parameters and variables found might contribute to inclusion into service routines so as to start, make progress and guide clinical practice.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):373-379
DOI 10.5935/0103-507X.20160067
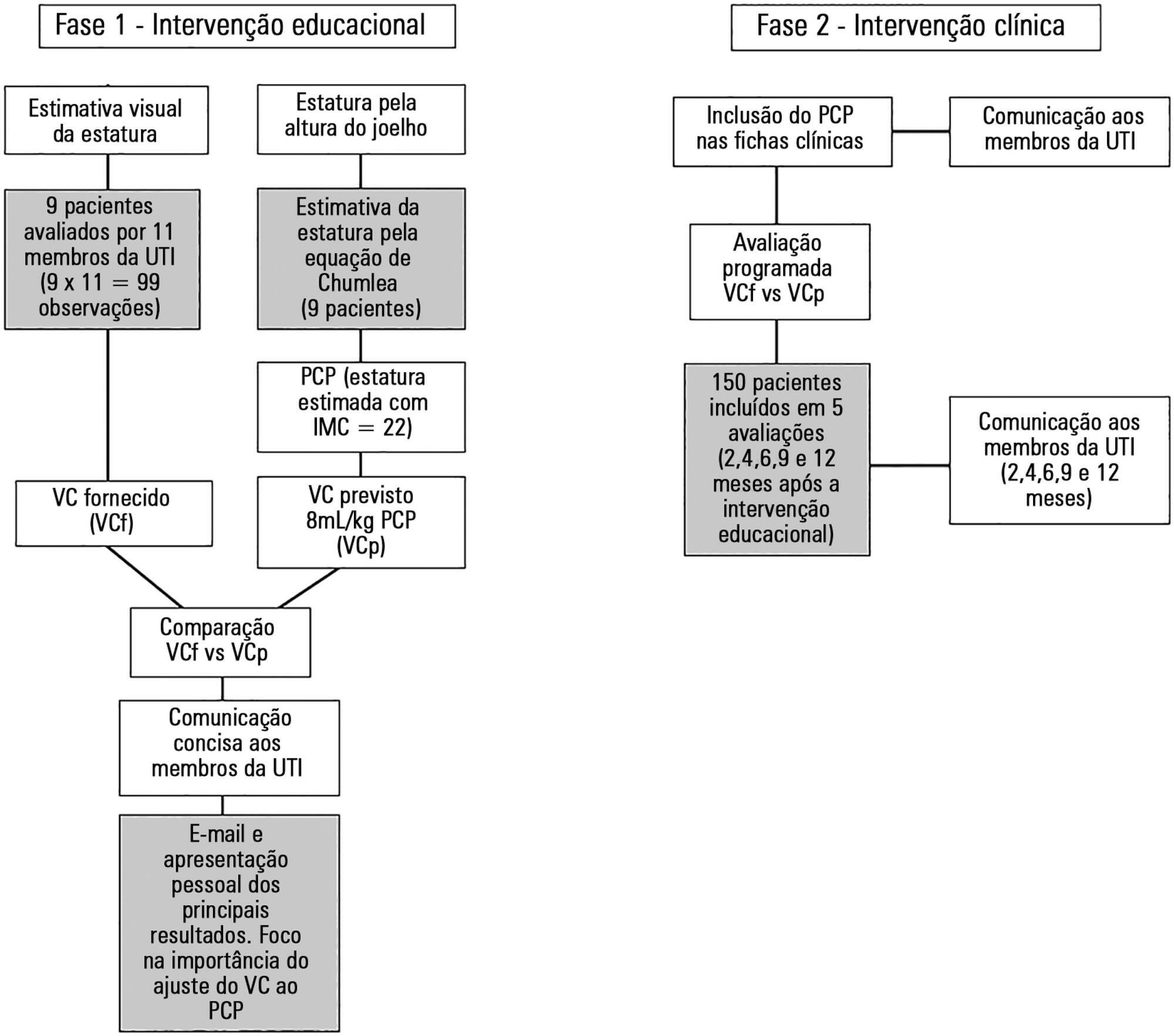
To determine the effect of feedback and education regarding the use of predicted body weight to adjust tidal volume in a lung-protective mechanical ventilation strategy.
The study was performed from October 2014 to November 2015 (12 months) in a single university polyvalent intensive care unit. We developed a combined intervention (education and feedback), placing particular attention on the importance of adjusting tidal volumes to predicted body weight bedside. In parallel, predicted body weight was estimated from knee height and included in clinical charts.
One hundred fifty-nine patients were included. Predicted body weight assessed by knee height instead of visual evaluation revealed that the delivered tidal volume was significantly higher than predicted. After the inclusion of predicted body weight, we observed a sustained reduction in delivered tidal volume from a mean (standard error) of 8.97 ± 0.32 to 7.49 ± 0.19mL/kg (p < 0.002). Furthermore, the protocol adherence was subsequently sustained for 12 months (delivered tidal volume 7.49 ± 0.54 versus 7.62 ± 0.20mL/kg; p = 0.103).
The lack of a reliable method to estimate the predicted body weight is a significant impairment for the application of a worldwide standard of care during mechanical ventilation. A combined intervention based on education and repeated feedbacks promoted sustained tidal volume education during the study period (12 months).
Abstract
Rev Bras Ter Intensiva. 2016;28(2):167-178
DOI 10.5935/0103-507X.20160020
Asthma is the most common chronic illness in childhood. Although the vast majority of children with acute asthma exacerbations do not require critical care, some fail to respond to standard treatment and require escalation of support. Children with critical or near-fatal asthma require close monitoring for deterioration and may require aggressive treatment strategies. This review examines the available evidence supporting therapies for critical and near-fatal asthma and summarizes the contemporary clinical care of these children. Typical treatment includes parenteral corticosteroids and inhaled or intravenous beta-agonist drugs. For children with an inadequate response to standard therapy, inhaled ipratropium bromide, intravenous magnesium sulfate, methylxanthines, helium-oxygen mixtures, and non-invasive mechanical support can be used. Patients with progressive respiratory failure benefit from mechanical ventilation with a strategy that employs large tidal volumes and low ventilator rates to minimize dynamic hyperinflation, barotrauma, and hypotension. Sedatives, analgesics and a neuromuscular blocker are often necessary in the early phase of treatment to facilitate a state of controlled hypoventilation and permissive hypercapnia. Patients who fail to improve with mechanical ventilation may be considered for less common approaches, such as inhaled anesthetics, bronchoscopy, and extracorporeal life support. This contemporary approach has resulted in extremely low mortality rates, even in children requiring mechanical support.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):11-18
DOI 10.5935/0103-507X.20160006
The aim of this study was to explore the factors associated with blood oxygen partial pressure and carbon dioxide partial pressure.
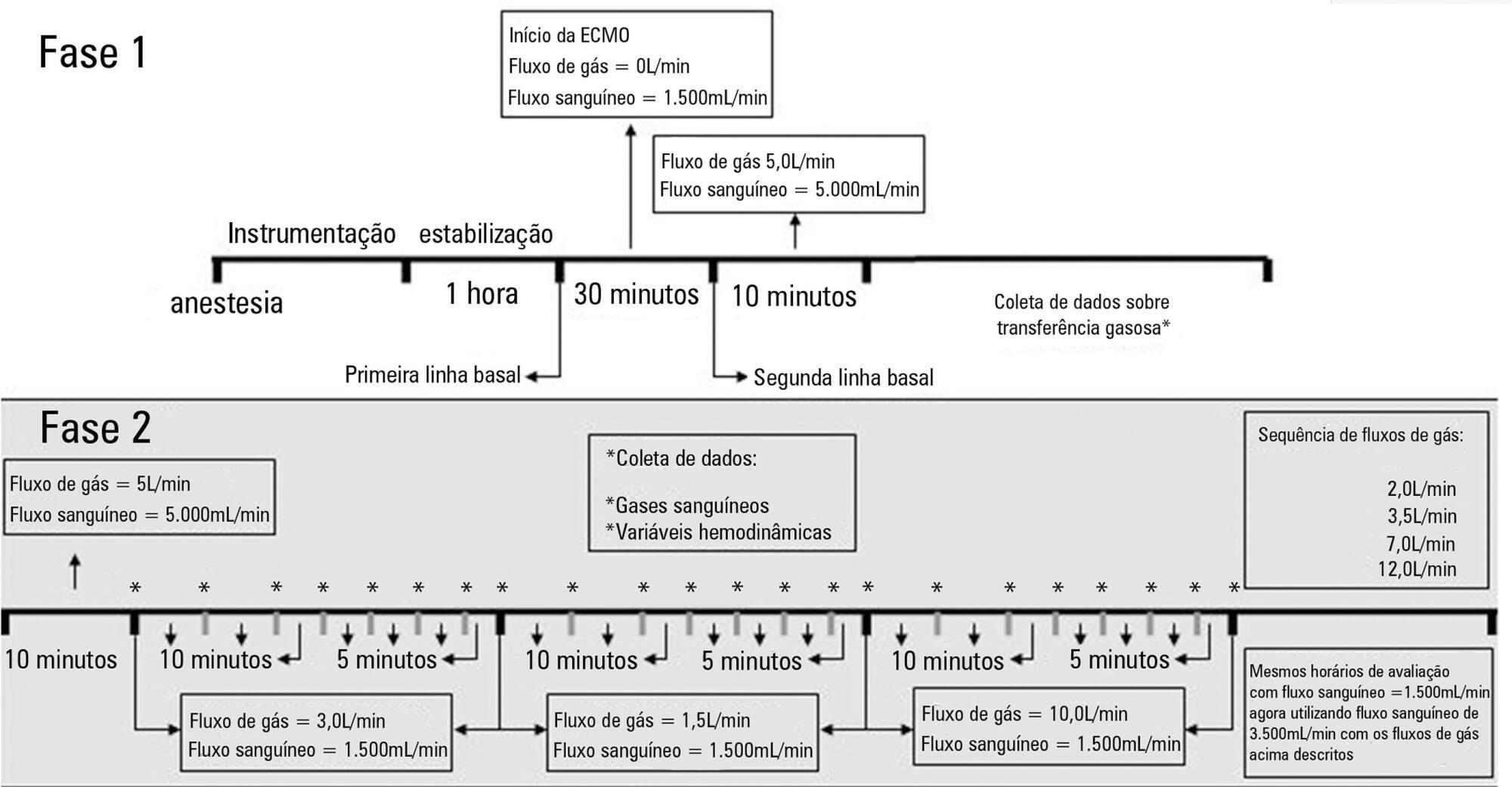
The factors associated with oxygen - and carbon dioxide regulation were investigated in an apneic pig model under veno-venous extracorporeal membrane oxygenation support. A predefined sequence of blood and sweep flows was tested.
Oxygenation was mainly associated with extracorporeal membrane oxygenation blood flow (beta coefficient = 0.036mmHg/mL/min), cardiac output (beta coefficient = -11.970mmHg/L/min) and pulmonary shunting (beta coefficient = -0.232mmHg/%). Furthermore, the initial oxygen partial pressure and carbon dioxide partial pressure measurements were also associated with oxygenation, with beta coefficients of 0.160 and 0.442mmHg/mmHg, respectively. Carbon dioxide partial pressure was associated with cardiac output (beta coefficient = 3.578mmHg/L/min), sweep gas flow (beta coefficient = -2.635mmHg/L/min), temperature (beta coefficient = 4.514mmHg/ºC), initial pH (beta coefficient = -66.065mmHg/0.01 unit) and hemoglobin (beta coefficient = 6.635mmHg/g/dL).
In conclusion, elevations in blood and sweep gas flows in an apneic veno-venous extracorporeal membrane oxygenation model resulted in an increase in oxygen partial pressure and a reduction in carbon dioxide partial pressure 2, respectively. Furthermore, without the possibility of causal inference, oxygen partial pressure was negatively associated with pulmonary shunting and cardiac output, and carbon dioxide partial pressure was positively associated with cardiac output, core temperature and initial hemoglobin.