Abstract
Rev Bras Ter Intensiva. 2019;31(1):47-56
DOI 10.5935/0103-507X.20190011
To determine the association between the primary site of infection and in-hospital mortality as the main outcome, or the need for admission to the intensive care unit as a secondary outcome, in patients with sepsis admitted to the emergency department.
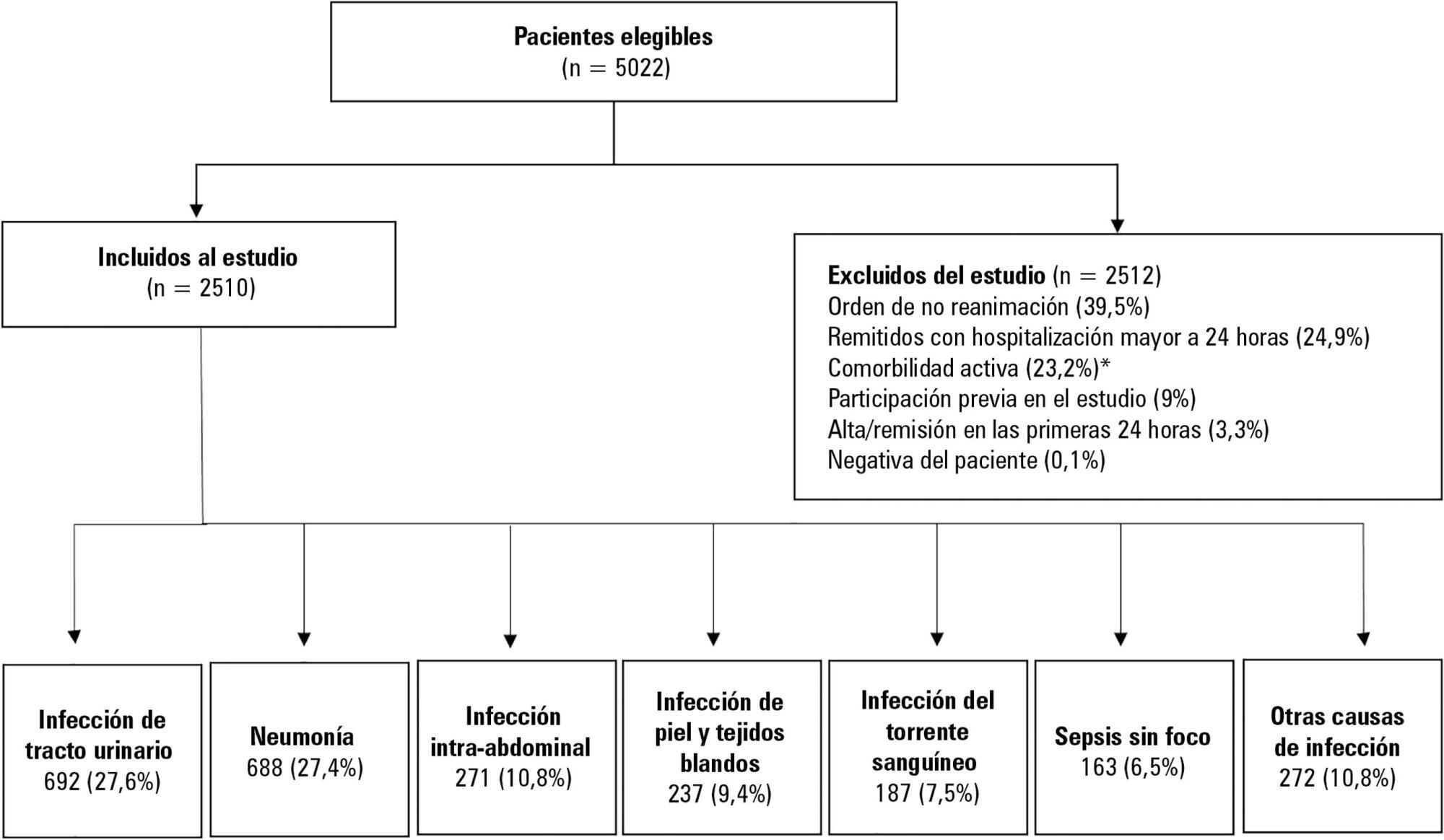
This was a secondary analysis of a multicenter prospective cohort. Patients included in the study were older than 18 years with a diagnosis of severe sepsis or septic shock who were admitted to the emergency departments of three tertiary care hospitals. Of the 5022 eligible participants, 2510 were included. Multiple logistic regression analysis was performed for mortality.
The most common site of infection was the urinary tract, present in 27.8% of the cases, followed by pneumonia (27.5%) and intra-abdominal focus (10.8%). In 5.4% of the cases, no definite site of infection was identified on admission. Logistic regression revealed a significant association between the following sites of infection and in-hospital mortality when using the urinary infection group as a reference: pneumonia (OR 3.4; 95%CI, 2.2 - 5.2; p < 0.001), skin and soft tissues (OR 2.6; 95%CI, 1.4 - 5.0; p = 0.003), bloodstream (OR 2.0; 95%CI, 1.1 - 3.6; p = 0.018), without specific focus (OR 2.0; 95%CI, 1.1 - 3.8; p = 0.028), and intra-abdominal focus (OR 1.9; 95%CI, 1.1 - 3.3; p = 0.024).
There is a significant association between the different sites of infection and in-hospital mortality or the need for admission to an intensive care unit in patients with sepsis or septic shock. Urinary tract infection shows the lowest risk, which should be considered in prognostic models of these conditions.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):64-70
DOI 10.5935/0103-507X.20180012
To describe a cohort of patients with acute liver failure and to analyze the demographic and clinical factors associated with mortality.
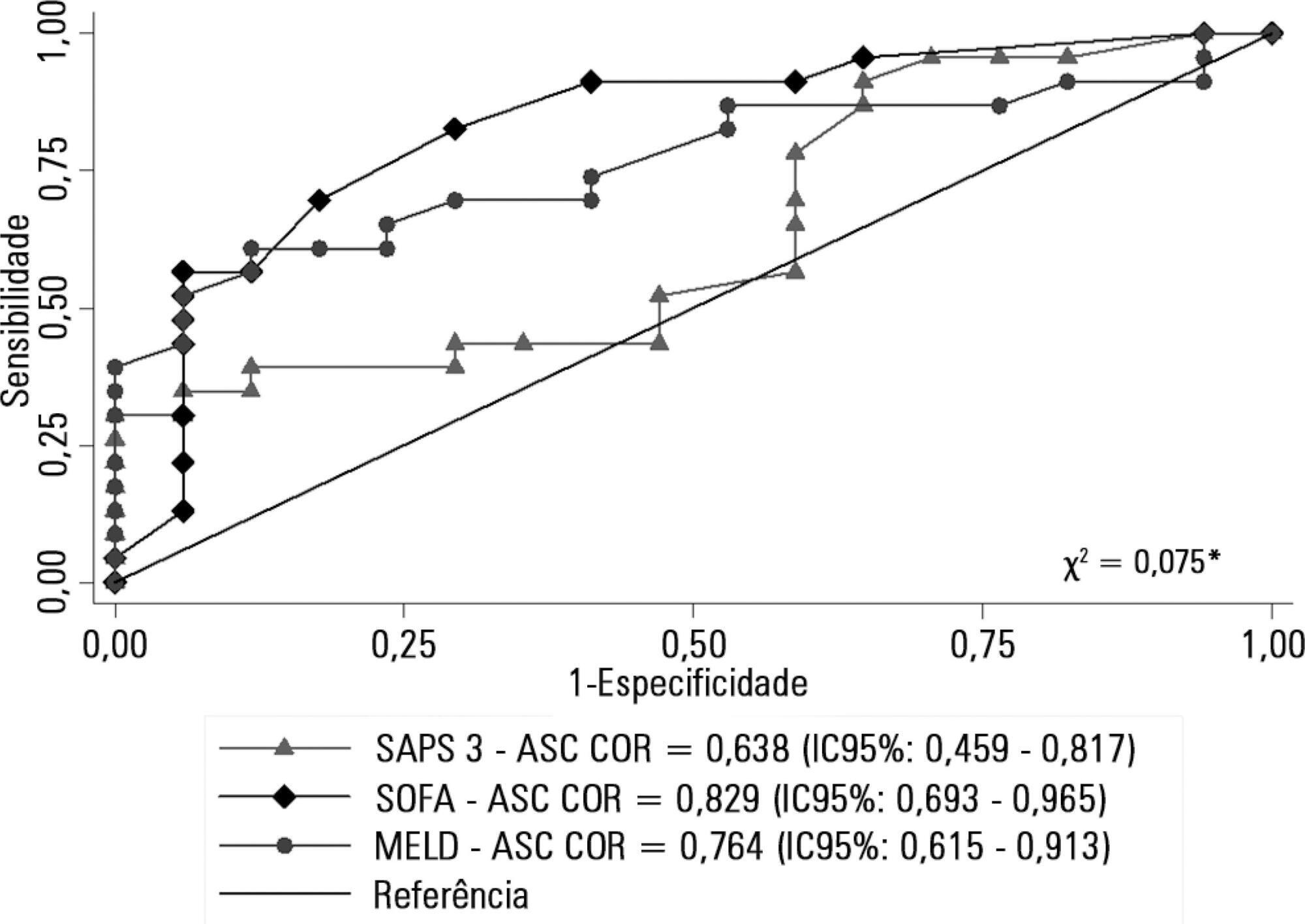
Retrospective cohort study in which all patients admitted for acute liver failure from July 28, 2012, to August 31, 2017, were included. Clinical and demographic data were collected using the Epimed System. The SAPS 3, SOFA, and MELD scores were measured. The odds ratios and 95% confidence intervals were estimated. Receiver operating characteristics curves were obtained for the prognostic scores, along with the Kaplan-Meier survival curve for the score best predicting mortality.
The majority of the 40 patients were female (77.5%), and the most frequent etiology was hepatitis B (n = 13). Only 35% of the patients underwent liver transplantation. The in-hospital mortality rate was 57.5% (95%CI: 41.5 - 73.5). Among the scores investigated, only SOFA remained associated with risk of death (OR = 1.37; 95%CI 1.11 - 1.69; p < 0.001). After SOFA stratification into < 12 and ≥ 12 points, survival was higher in patients with SOFA <12 (log-rank p < 0.001).
SOFA score in the first 24 hours was the best predictor of fatal outcome.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):153-159
DOI 10.5935/0103-507X.20180030
To investigate prognostic factors among critically ill patients with community-acquired bacterial meningitis and acute kidney injury.
A retrospective study including patients admitted to a tertiary infectious disease hospital in Fortaleza, Brazil diagnosed with community-acquired bacterial meningitis complicated with acute kidney injury. Factors associated with death, mechanical ventilation and use of vasopressors were investigated.
Forty-one patients were included, with a mean age of 41.6 ± 15.5 years; 56% were males. Mean time between intensive care unit admission and acute kidney injury diagnosis was 5.8 ± 10.6 days. Overall mortality was 53.7%. According to KDIGO criteria, 10 patients were classified as stage 1 (24.4%), 18 as stage 2 (43.9%) and 13 as stage 3 (31.7%). KDIGO 3 significantly increased mortality (OR = 6.67; 95%CI = 1.23 - 36.23; p = 0.028). Thrombocytopenia was not associated with higher mortality, but it was a risk factor for KDIGO 3 (OR = 5.67; 95%CI = 1.25 - 25.61; p = 0.024) and for mechanical ventilation (OR = 6.25; 95%CI = 1.33 - 29.37; p = 0.02). Patients who needed mechanical ventilation by 48 hours from acute kidney injury diagnosis had higher urea (44.6 versus 74mg/dL, p = 0.039) and sodium (138.6 versus 144.1mEq/L; p = 0.036).
Mortality among critically ill patients with community-acquired bacterial meningitis and acute kidney injury is high. Acute kidney injury severity was associated with even higher mortality. Thrombocytopenia was associated with severer acute kidney injury. Higher urea was an earlier predictor of severer acute kidney injury than was creatinine.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):160-165
DOI 10.5935/0103-507X.20180034
To compare the prevalence of malnutrition during two time periods in a pediatric intensive care unit.
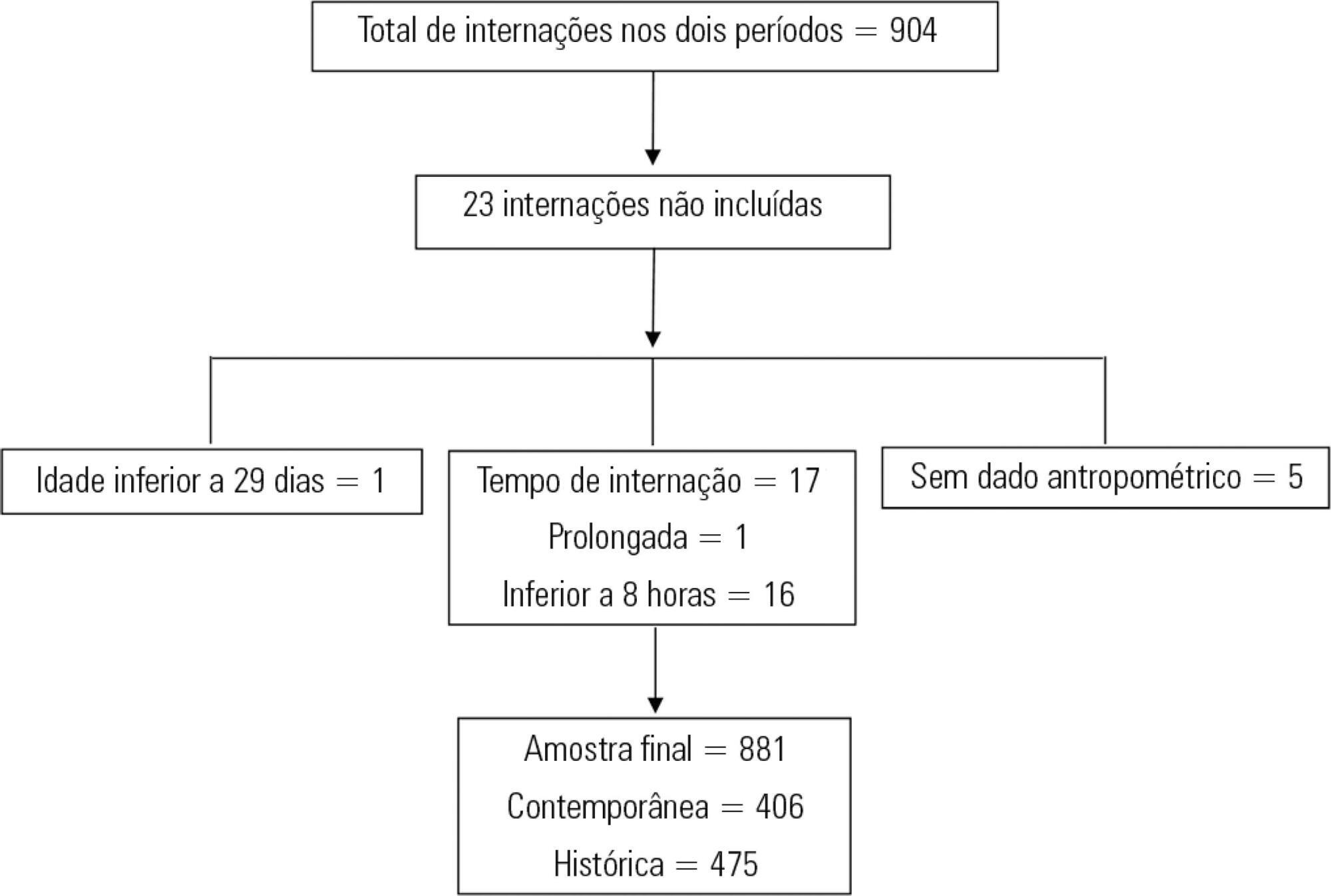
This was a retrospective cross-sectional study of patients admitted to the pediatric intensive care unit of a university hospital during two one-year periods with an interval of four years between them. Nutritional evaluation was conducted based on weight and height measured at admission. The body mass index-for-age was the parameter chosen to evaluate nutritional status, as classified according to the World Health Organization, according to age group.
The total sample size was 881 (406 in the contemporary sample and 475 in the historical sample). There was a significant reduction in malnutrition in the contemporary sample (p = 0.03). Malnourishment in patients in the historical sample was significantly associated with mortality and length of stay, while malnourishment in patients in the contemporary sample was not associated with worse outcomes.
There was a significant reduction in malnutrition among patients in the same pediatric intensive care unit when comparing the two time periods. Our findings of a change in nutritional profile in critically ill patients corroborate the nutritional status data of children and adolescents worldwide.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):181-186
DOI 10.5935/0103-507X.20180032
To evaluate the calibration and discrimination of APACHE IV in the postoperative period after kidney transplantation.
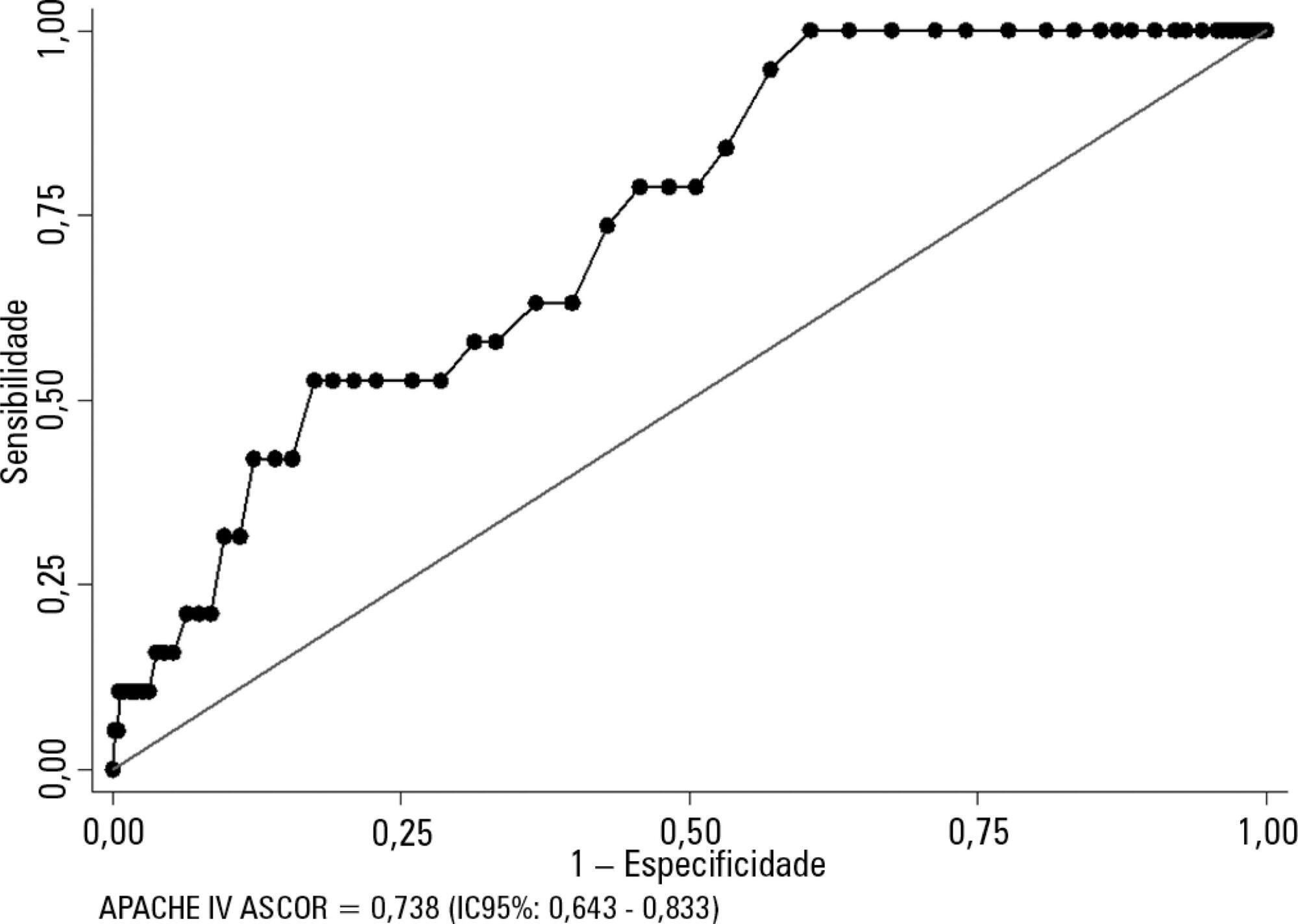
This clinical cohort study included 986 hospitalized adult patients in the immediate postoperative period after kidney transplantation, in a single center in southern Brazil.
Kidney transplant patients who died in hospital had significantly higher APACHE IV values and higher predicted mortality. The APACHE IV score showed adequate calibration (H-L 11.24 p = 0.188) and a good discrimination ROC curve of 0.738 (95%CI 0.643 - 0.833, p < 0.001), although SMR overestimated mortality (SMR = 0.73; 95%CI: 0.24 - 1.42, p = 0.664).
The APACHE IV score showed adequate performance for predicting hospital outcomes in the postoperative period for kidney transplant recipients.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):317-324
DOI 10.5935/0103-507X.20170047
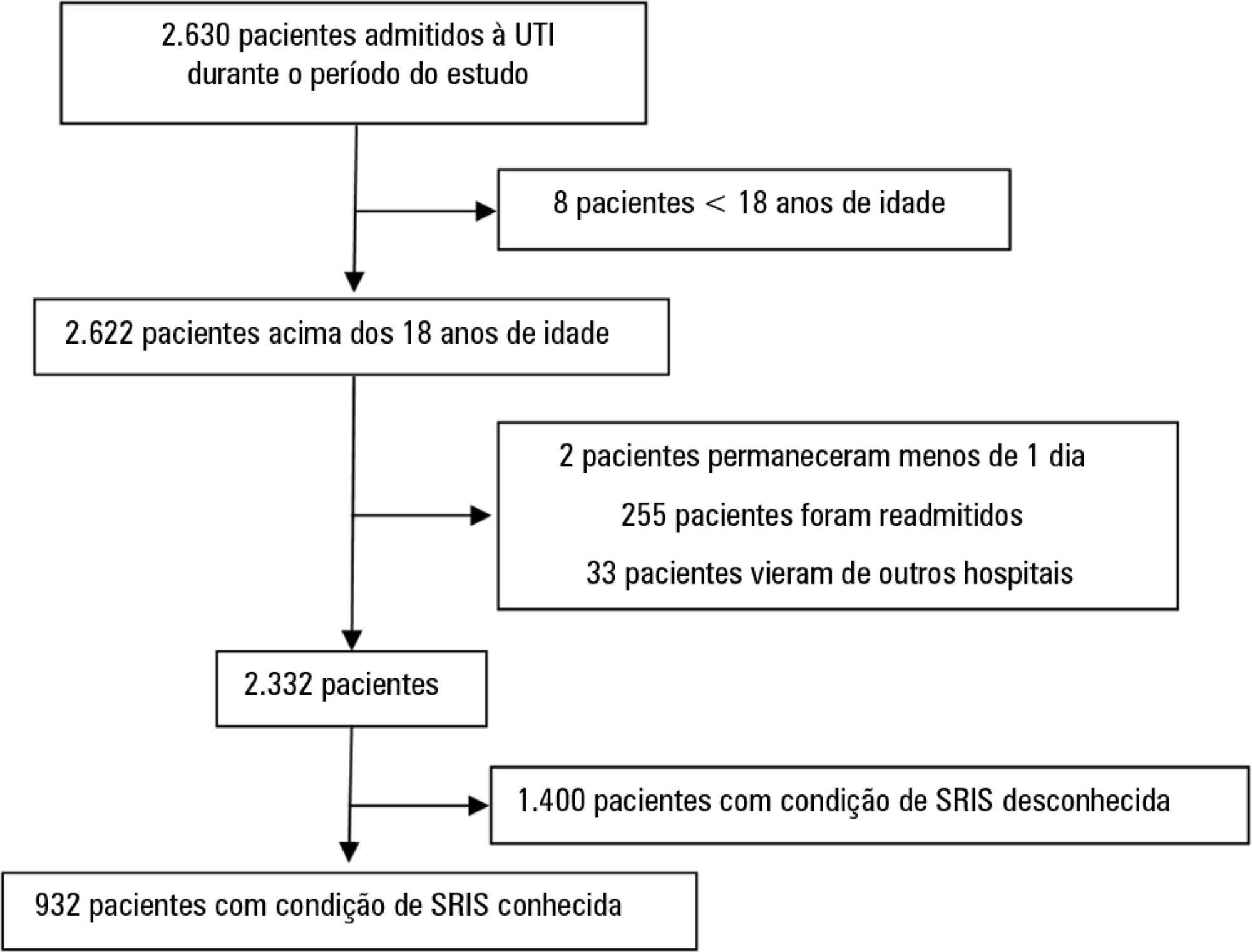
This study intended to determine whether the systemic inflammatory response syndrome criteria can predict hospital mortality in a Brazilian cohort of critically ill patients.
We performed a retrospective cohort study at a private tertiary hospital in São Paulo (SP), Brazil. We extracted information from the adult intensive care unit database (Sistema EpimedTM). We compared the SAPS 3 and the systemic inflammatory response syndrome model as dichotomous (≥ 2 criteria: systemic inflammatory response syndrome -positive versus 0 - 1 criterion: systemic inflammatory response syndrome -negative) and ordinal variables from 0 to 4 (according to the number of systemic inflammatory response syndrome criteria met) in the prediction of hospital mortality at intensive care unit admission. Model discrimination was compared using the area under the receiver operating characteristics (AUROC) curve.
From January to December 2012, we studied 932 patients (60.4% were systemic inflammatory response syndrome -positive). systemic inflammatory response syndrome -positive patients were more critically ill than systemic inflammatory response syndrome -negative patients and had higher hospital mortality (16.9% versus 8.1%, p < 0.001). In the adjusted analysis, being systemic inflammatory response syndrome -positive independently increased the risk of death by 82% (odds ratio 1.82; 95% confidence interval [CI] 1.12 - 2.96, p = 0.016). However, the AUROC curve for the SAPS 3 model was higher (0.81, 95%CI 0.78 - 0.85) compared to the systemic inflammatory response syndrome model with the systemic inflammatory response syndrome criteria as a dichotomous variable (0.60, 95%CI 0.55 - 0.65) and as an ordinal variable (0.62, 95%CI 0.57 - 0.68; p < 0.001) for hospital mortality.
Although systemic inflammatory response syndrome is associated with hospital mortality, the systemic inflammatory response syndrome criteria show low accuracy in the prediction of mortality compared with the SAPS 3.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):303-309
DOI 10.5935/0103-507X.20170041
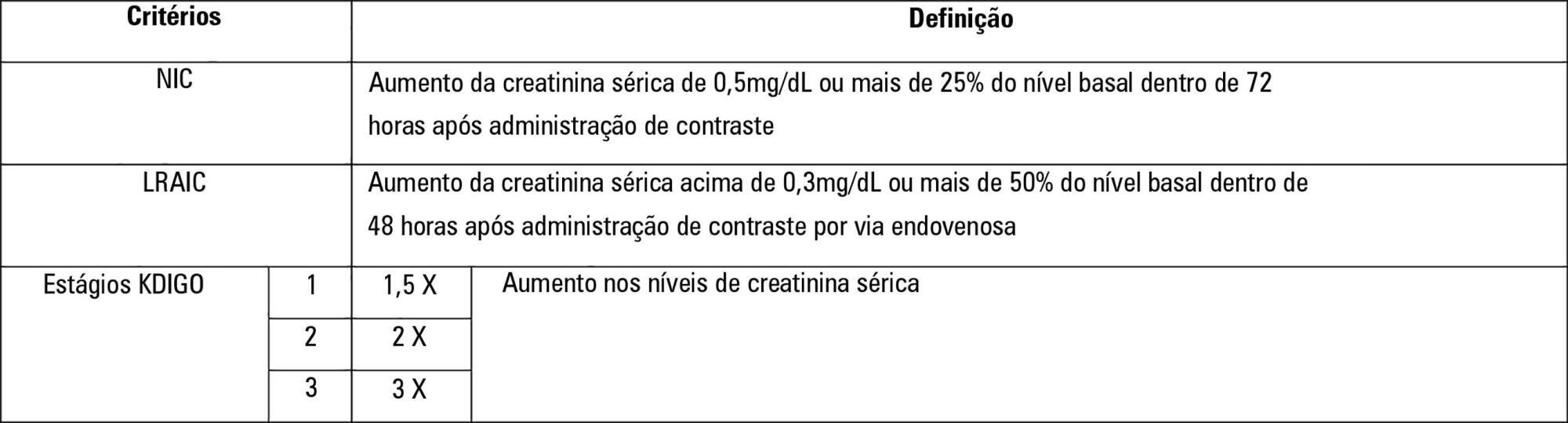
To establish whether there is superiority between contrast-induced acute kidney injury and contrast-induced nephropathy criteria as predictors of unfavorable clinical outcomes.
Retrospective study carried out in a tertiary hospital with 157 patients undergoing radiocontrast infusion for propaedeutic purposes.
One hundred forty patients fulfilled the inclusion criteria: patients who met the criteria for contrast-induced acute kidney injury (59) also met the criteria for contrast-induced nephropathy (76), 44.3% met the criteria for KDIGO staging, 6.4% of the patients required renal replacement therapy, and 10.7% died.
The diagnosis of contrast-induced nephropathy was the most sensitive criterion for renal replacement therapy and death, whereas KDIGO showed the highest specificity; there was no correlation between contrast volume and progression to contrast-induced acute kidney injury, contrast-induced nephropathy, support dialysis or death in the assessed population.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):63-69
DOI 10.5935/0103-507X.20170010
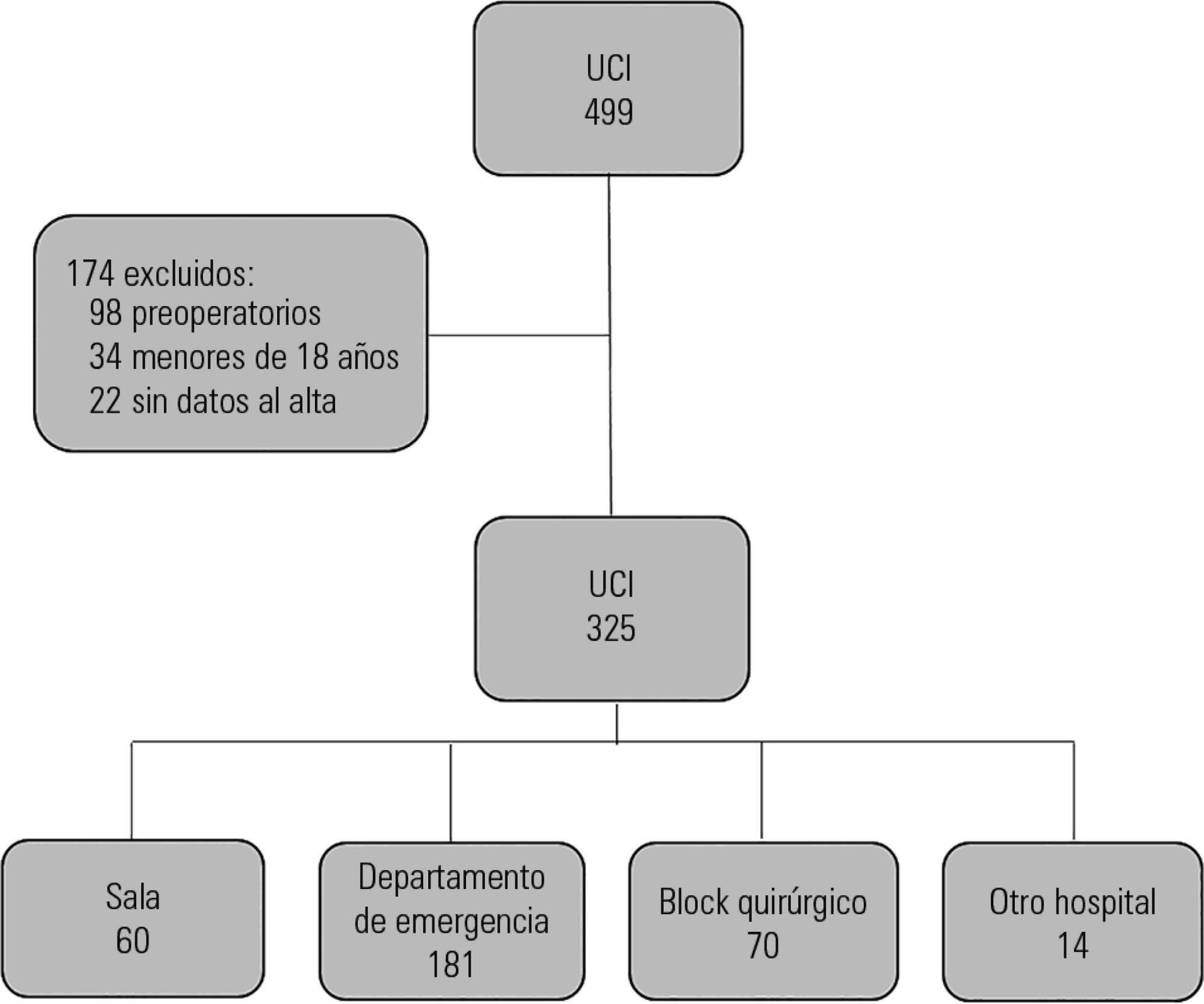
To determine the impact of the day and time of admission and discharge from the intensive care unit on mortality.
Prospective observational study that included patients admitted to the intensive care unit of the Hospital Maciel in Montevideo between April and November 2014.
We analyzed 325 patients with an average age of 55 (36 - 71) years and a SAPS II value of 43 (29 - 58) points. No differences were found in the mortality of patients in the intensive care unit when time of admission (35% on the weekend versus 31% on weekdays, p = ns) or the hour of entry (35% at night versus 31% in the daytime, p = ns) were compared. The time of discharge was associated with higher hospital mortality rates (57% for weekend discharges versus 14% for weekday discharges, p = 0.000). The factors independently associated with hospital mortality after discharge from the intensive care unit were age > 50 years (OR 2.4, 95%CI, 1.1 - 5.4) and weekend discharge (OR 7.7, 95%CI, 3.8-15.6).
This study identified the time of discharge from the intensive care unit as a factor that was independently associated with hospital mortality.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)