Abstract
Rev Bras Ter Intensiva. 2016;28(2):190-194
DOI 10.5935/0103-507X.20160032
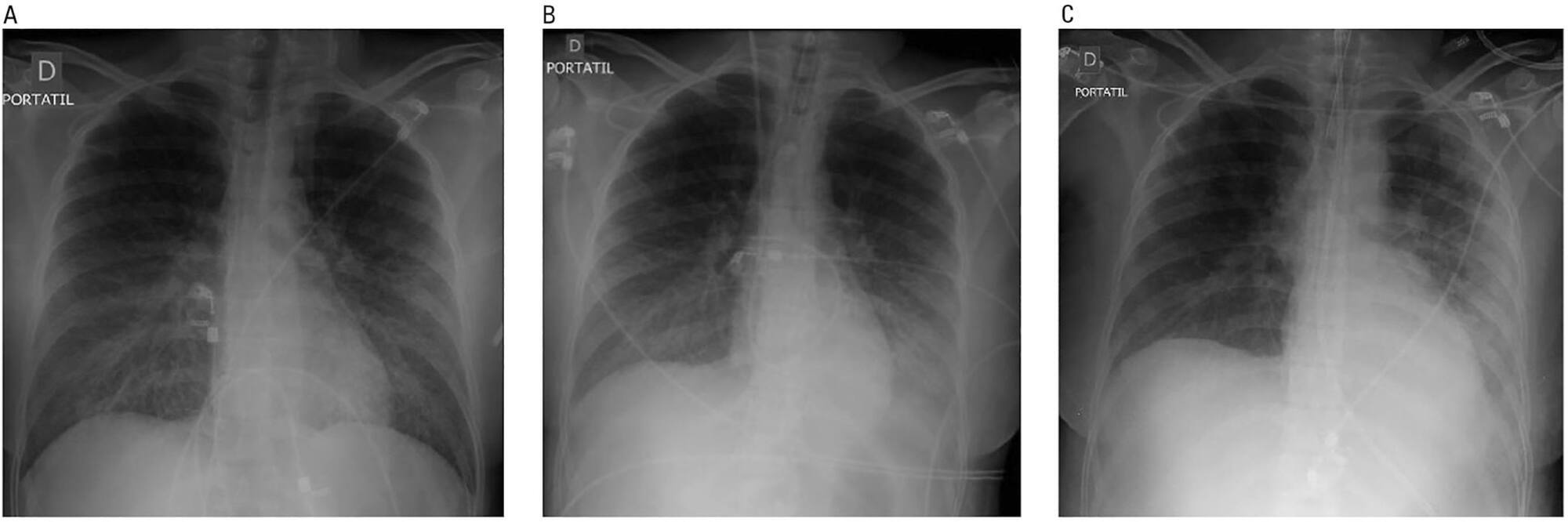
Hantavirus cardiopulmonary syndrome has a high mortality rate, and early connection to extracorporeal membrane oxygenation has been suggested to improve outcomes. We report the case of a patient with demonstrated Hantavirus cardiopulmonary syndrome and refractory shock who fulfilled the criteria for extracorporeal membrane oxygenation and responded successfully to high volume continuous hemofiltration. The implementation of high volume continuous hemofiltration along with protective ventilation reversed the shock within a few hours and may have prompted recovery. In patients with Hantavirus cardiopulmonary syndrome, a short course of high volume continuous hemofiltration may help differentiate patients who can be treated with conventional intensive care unit management from those who will require more complex therapies, such as extracorporeal membrane oxygenation.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):436-443
DOI 10.5935/0103-507X.20160077
To evaluate the clinical course and respiratory parameters of mechanically ventilated children with cancer suffering from sepsis-related acute respiratory distress syndrome.
This 2-year prospective, longitudinal, observational cohort study enrolled 29 children and adolescents. Clinical data, measurements of blood gases and ventilation parameters were collected at four different time points. Fluctuations between measurements as well as differences in estimated means were analyzed by linear mixed models in which death within 28 days from the onset of acute respiratory distress syndrome was the primary endpoint.
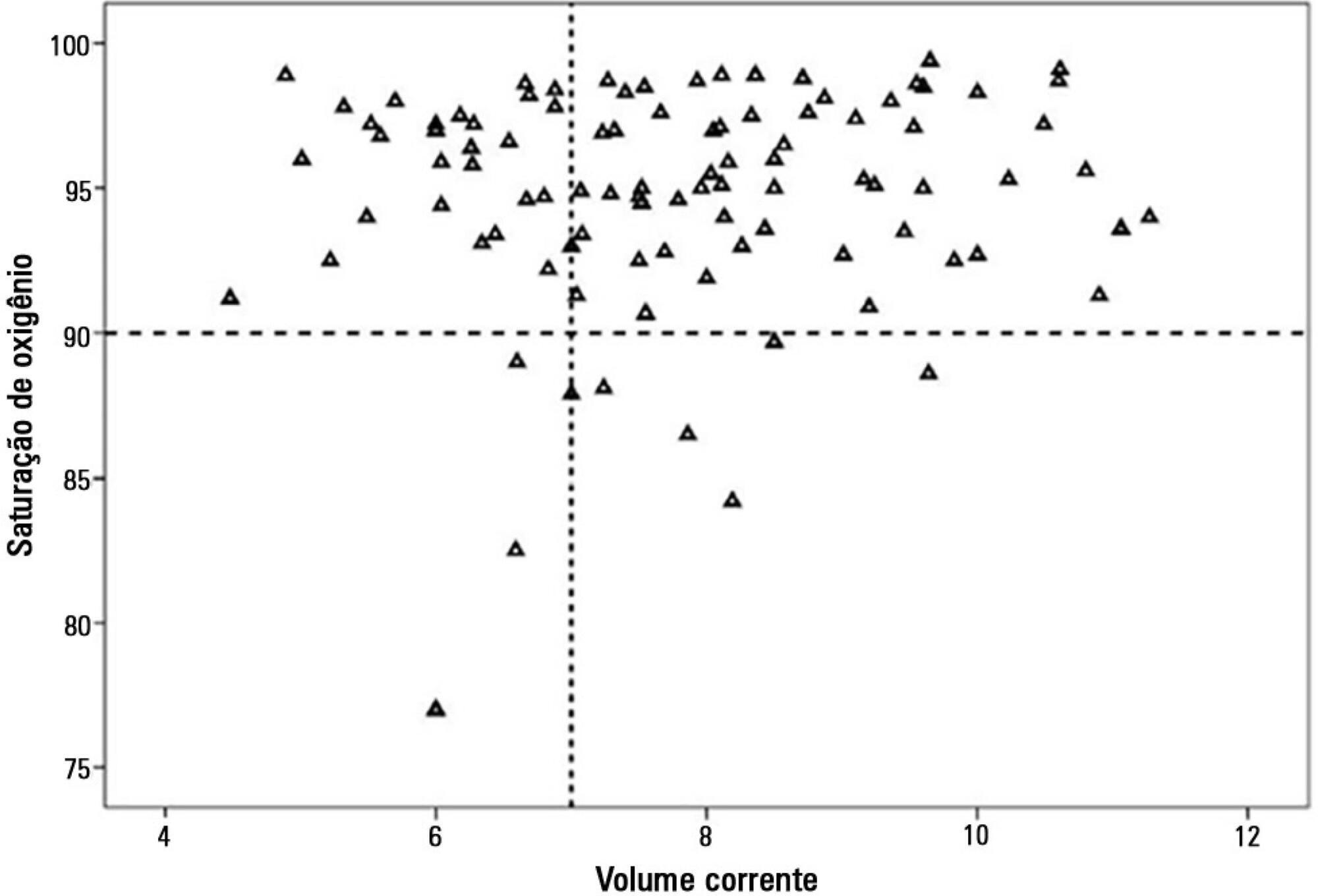
There were 17 deaths within 28 days of acute respiratory distress syndrome onset and another 7 between 29 - 60 days. Only 5 patients survived for more than 60 days. Nine (31%) patients died as a direct consequence of refractory hypoxemia, and the others died of multiple organ failure and catecholamine-refractory shock. In 66% of the measurements, the tidal volume required to obtain oxygen saturation equal to or above 90% was greater than 7mL/kg. The estimated means of dynamic compliance were low and were similar for survivors and non-survivors but with a negative slope between the first and final measurements, accompanied by a negative slope of the tidal volume for non-survivors. Non-survivors were significantly more hypoxemic, with PaO2/FiO2 ratios showing lower estimated means and a negative slope along the four measurements. Peak, expiratory and mean airway pressures showed positive slopes in the non-survivors, who also had more metabolic acidosis.
In most of our children with cancer, sepsis and acute respiratory distress syndrome progressed with deteriorating ventilation indexes and escalating organic dysfunction, making this triad nearly fatal in children.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):260-265
DOI 10.5935/0103-507X.20150047
>To evaluate the agreement between a new epidemiological surveillance method of the Center for Disease Control and Prevention and the clinical pulmonary infection score for mechanical ventilator-associated pneumonia detection.
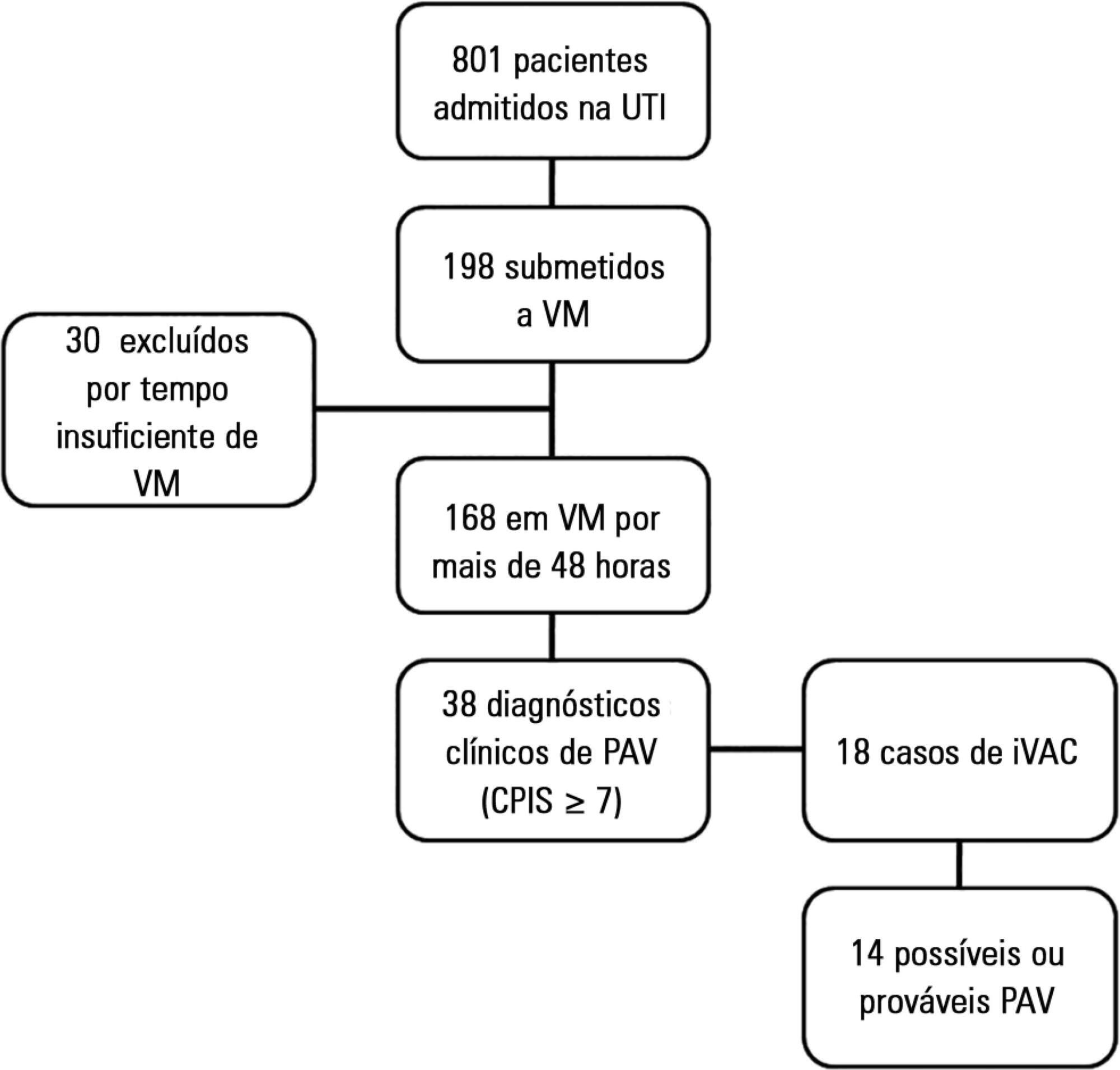
This was a prospective cohort study that evaluated patients in the intensive care units of two hospitals who were intubated for more than 48 hours between August 2013 and June 2014. Patients were evaluated daily by physical therapist using the clinical pulmonary infection score. A nurse independently applied the new surveillance method proposed by the Center for Disease Control and Prevention. The diagnostic agreement between the methods was evaluated. A clinical pulmonary infection score of ≥ 7 indicated a clinical diagnosis of mechanical ventilator-associated pneumonia, and the association of a clinical pulmonary infection score ≥ 7 with an isolated semiquantitative culture consisting of ≥ 104 colony-forming units indicated a definitive diagnosis.
Of the 801 patients admitted to the intensive care units, 198 required mechanical ventilation. Of these, 168 were intubated for more than 48 hours. A total of 18 (10.7%) cases of mechanical ventilation-associated infectious conditions were identified, 14 (8.3%) of which exhibited possible or probable mechanical ventilatorassociated pneumonia, which represented 35% (14/38) of mechanical ventilator-associated pneumonia cases. The Center for Disease Control and Prevention method identified cases of mechanical ventilator-associated pneumonia with a sensitivity of 0.37, specificity of 1.0, positive predictive value of 1.0, and negative predictive value of 0.84. The differences resulted in discrepancies in the mechanical ventilator-associated pneumonia incidence density (CDC, 5.2/1000 days of mechanical ventilation; clinical pulmonary infection score ≥ 7, 13.1/1000 days of mechanical ventilation).
The Center for Disease Control and Prevention method failed to detect mechanical ventilatorassociated pneumonia cases and may not be satisfactory as a surveillance method.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):51-56
DOI 10.5935/0103-507X.20150009
To assess the causes and factors associated with the death of patients between intensive care unit discharge and hospital discharge.
The present is a pilot, retrospective, observational cohort study. The records of all patients admitted to two units of a public/private university hospital from February 1, 2013 to April 30, 2013 were assessed. Demographic and clinical data, risk scores and outcomes were obtained from the Epimed monitoring system and confirmed in the electronic record system of the hospital. The relative risk and respective confidence intervals were calculated.
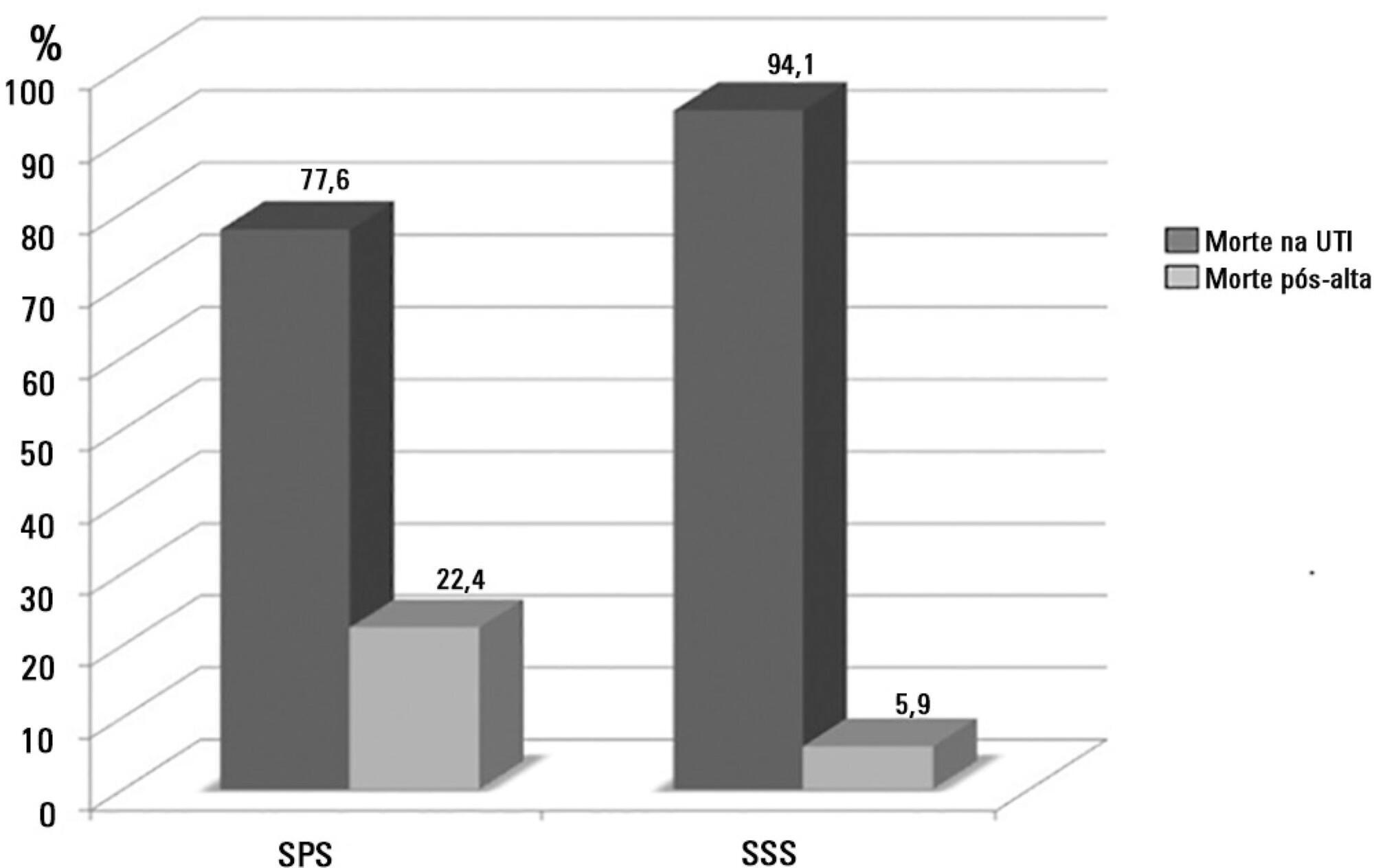
A total of 581 patients were evaluated. The mortality rate in the intensive care unit was 20.8% and in the hospital was 24.9%. Septic shock was the cause of death in 58.3% of patients who died after being discharged from the intensive care unit. Of the patients from the public health system, 73 (77.6%) died in the intensive care unit and 21 (22.4%) died in the hospital after being discharged from the unit. Of the patients from the Supplementary Health System, 48 (94.1%) died in the intensive care unit and 3 (5.9%) died in the hospital after being discharged from the unit (relative risk, 3.87%; 95% confidence interval, 1.21 - 12.36; p < 0.05). The post-discharge mortality rate was significantly higher in patients with intensive care unit hospitalization time longer than 6 days.
The main cause of death of patients who were discharged from the intensive care unit and died in the ward before hospital discharge was septic shock. Coverage by the public healthcare system and longer hospitalization time in the intensive care unit were factors associated with death after discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):57-63
DOI 10.5935/0103-507X.20150010
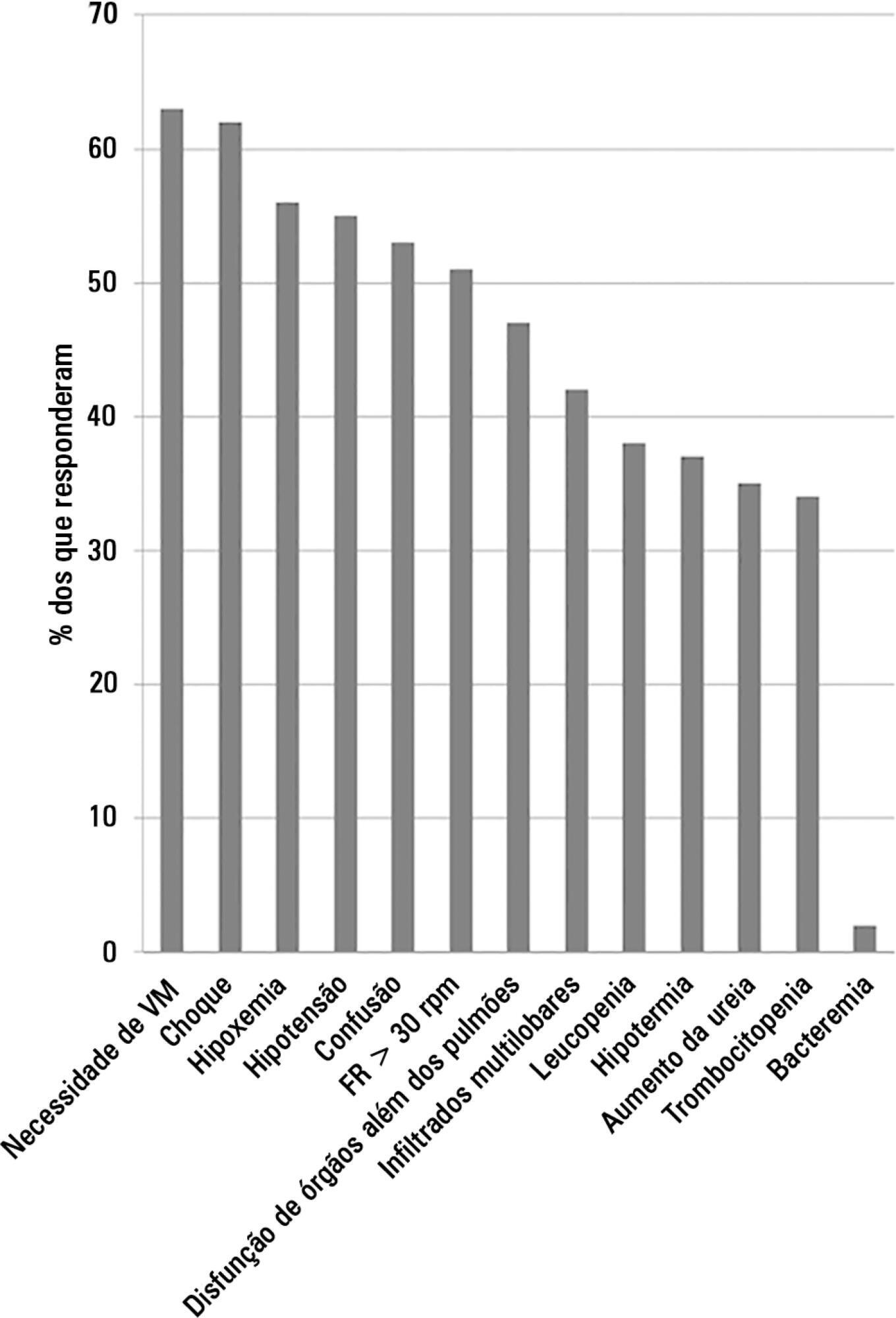
This study aimed to evaluate Brazilian physicians’ perceptions regarding the diagnosis, severity assessment, treatment and risk stratification of severe community-acquired pneumonia patients and to compare those perceptions to current guidelines.
We conducted a cross-sectional international anonymous survey among a convenience sample of critical care, pulmonary, emergency and internal medicine physicians from Brazil between October and December 2008. The electronic survey evaluated physicians’ attitudes towards the diagnosis, risk assessment and therapeutic interventions for patients with severe community-acquired pneumonia.
A total of 253 physicians responded to the survey, with 66% from Southeast Brazil. The majority (60%) of the responding physicians had > 10 years of medical experience. The risk assessment of severe community-acquired pneumonia was very heterogeneous, with clinical evaluation as the most frequent approach. Although blood cultures were recognized as exhibiting a poor diagnostic performance, these cultures were performed by 75% of respondents. In contrast, the presence of urinary pneumococcal and Legionella antigens was evaluated by less than 1/3 of physicians. The vast majority of physicians (95%) prescribe antibiotics according to a guideline, with the combination of a 3rd/4th generation cephalosporin plus a macrolide as the most frequent choice.
This Brazilian survey identified an important gap between guidelines and clinical practice and recommends the institution of educational programs that implement evidence-based strategies for the management of severe community-acquired pneumonia.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):10-17
DOI 10.5935/0103-507X.20150004
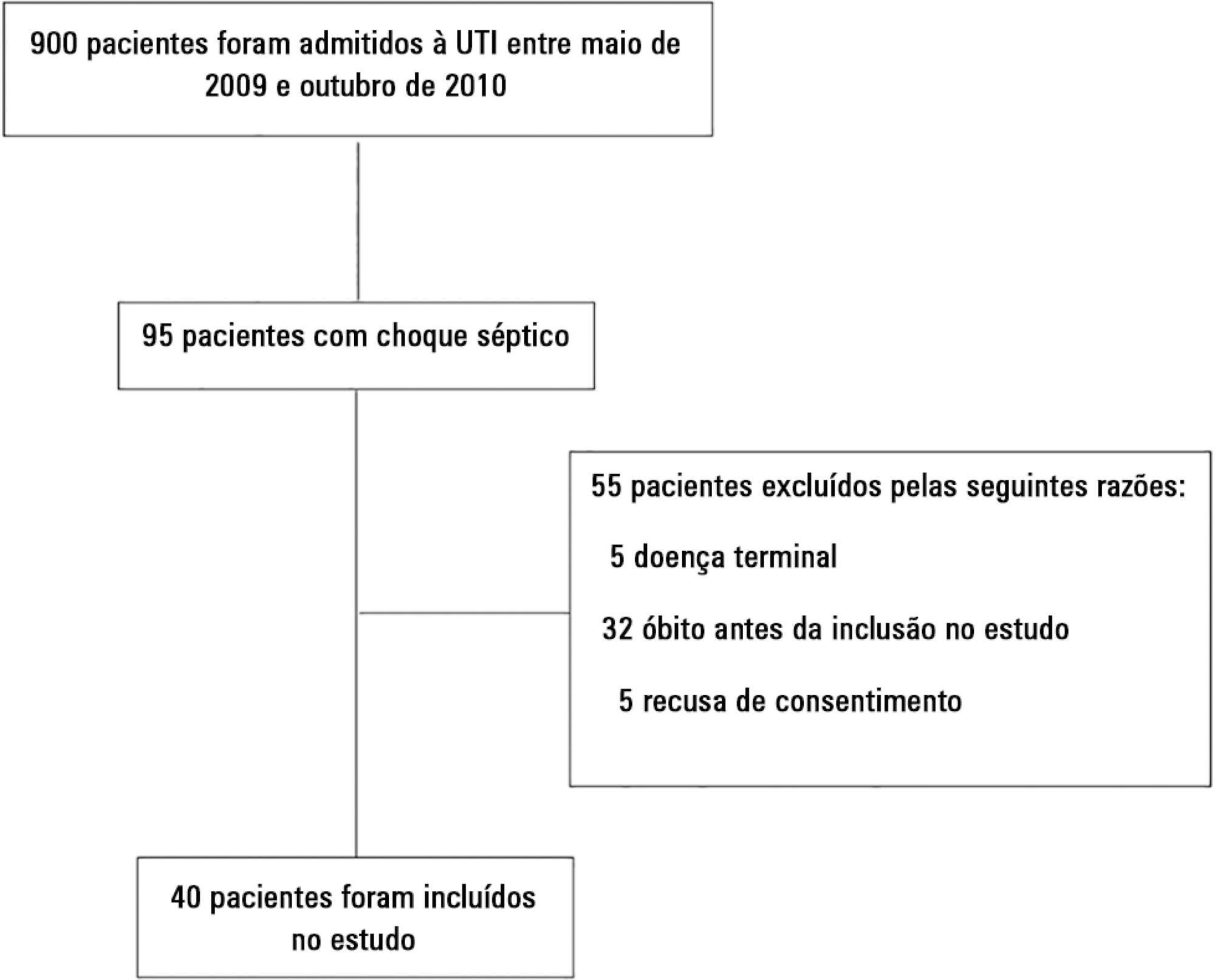
We aimed to evaluate the cumulative fluid balance during the period of shock and determine what happens to fluid balance in the 7 days following recovery from shock.
A prospective and observational study in septic shock patients. Patients with a mean arterial pressure ≥ 65mmHg and lactate < 2.0mEq/L were included < 12 hours after weaning from vasopressor, and this day was considered day 1. The daily fluid balance was registered during and for seven days after recovery from shock. Patients were divided into two groups according to the full cohort’s median cumulative fluid balance during the period of shock: Group 1 ≤ 4.4L (n = 20) and Group 2 > 4.4L (n = 20).
We enrolled 40 patients in the study. On study day 1, the cumulative fluid balance was 1.1 [0.6 - 3.4] L in Group 1 and 9.0 [6.7 - 13.8] L in Group 2. On study day 7, the cumulative fluid balance was 8.0 [4.5 - 12.4] L in Group 1 and 14.7 [12.7 - 20.6] L in Group 2 (p < 0.001 for both). Afterwards, recovery of shock fluid balance continued to increase in both groups. Group 2 had a more prolonged length of stay in the intensive care unit and hospital compared to Group 1.
In conclusion, positive fluid balances are frequently seen in patients with septic shock and may be related to worse outcomes. During the shock period, even though the fluid balance was previously positive, it becomes more positive. After recovery from shock, the fluid balance continues to increase. The group with a more positive fluid balance group spent more time in the intensive care unit and hospital.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):36-43
DOI 10.5935/0103-507X.20150007
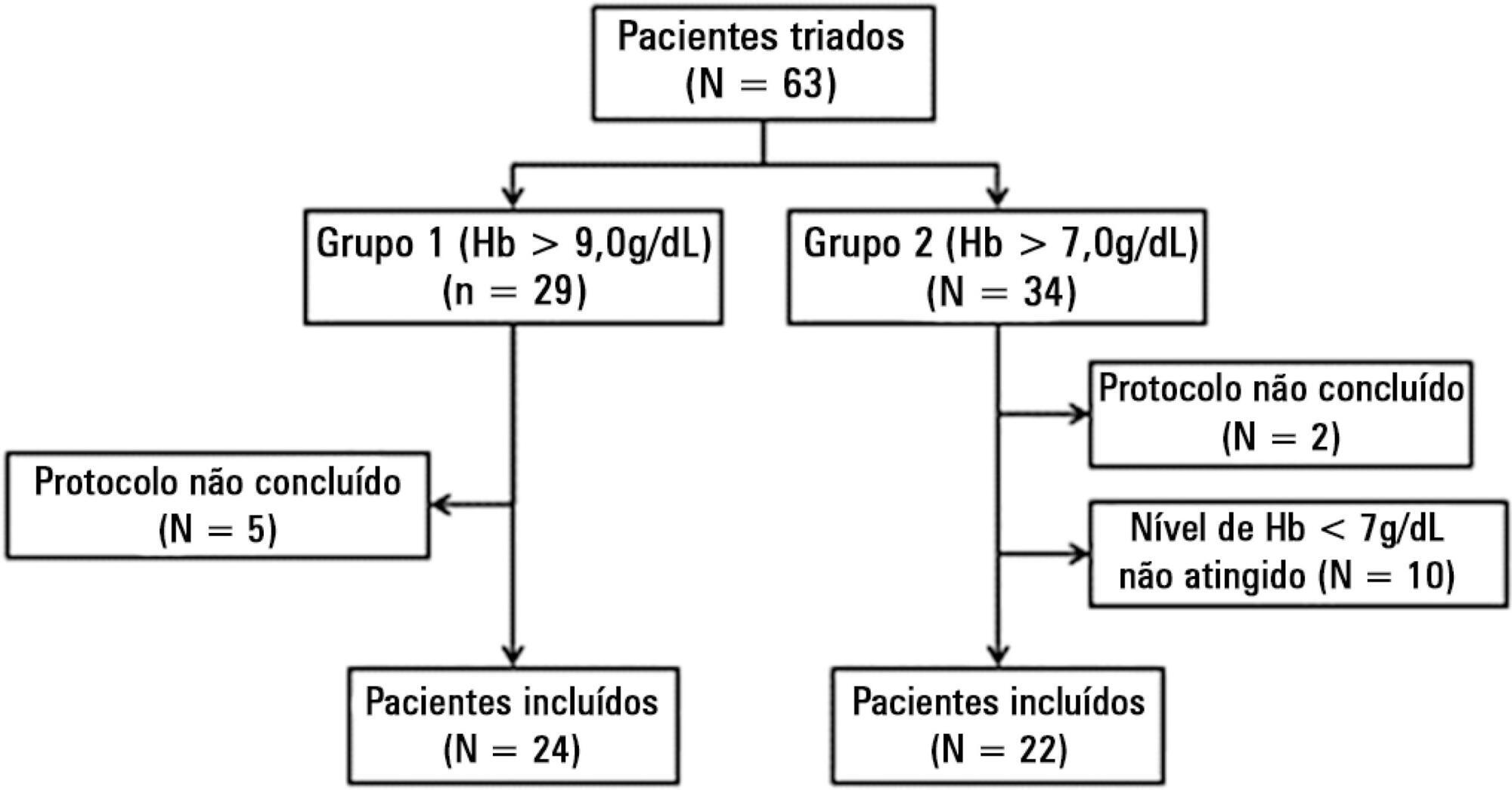
To evaluate the immediate effects of red blood cell transfusion on central venous oxygen saturation and lactate levels in septic shock patients with different transfusion triggers.
We included patients with a diagnosis of septic shock within the last 48 hours and hemoglobin levels below 9.0g/dL Patients were randomized for immediate transfusion with hemoglobin concentrations maintained above 9.0g/dL (Group Hb9) or to withhold transfusion unless hemoglobin felt bellow 7.0g/dL (Group Hb7). Hemoglobin, lactate, central venous oxygen saturation levels were determined before and one hour after each transfusion.
We included 46 patients and 74 transfusions. Patients in Group Hb7 had a significant reduction in median lactate from 2.44 (2.00 - 3.22) mMol/L to 2.21 (1.80 - 2.79) mMol/L, p = 0.005, which was not observed in Group Hb9 [1.90 (1.80 - 2.65) mMol/L to 2.00 (1.70 - 2.41) mMol/L, p = 0.23]. Central venous oxygen saturation levels increased in Group Hb7 [68.0 (64.0 - 72.0)% to 72.0 (69.0 - 75.0)%, p < 0.0001] but not in Group Hb9 [72.0 (69.0 - 74.0)% to 72.0 (71.0 - 73.0)%, p = 0.98]. Patients with elevated lactate or central venous oxygen saturation < 70% at baseline had a significant increase in these variables, regardless of baseline hemoglobin levels. Patients with normal values did not show a decrease in either group.
Red blood cell transfusion increased central venous oxygen saturation and decreased lactate levels in patients with hypoperfusion regardless of their baseline hemoglobin levels. Transfusion did not appear to impair these variables in patients without hypoperfusion.
Abstract
Rev Bras Ter Intensiva. 2015;27(4):333-339
DOI 10.5935/0103-507X.20150057
To evaluate the prevalence of myocardial dysfunction and its prognostic value in patients with severe sepsis and septic shock.
Adult septic patients admitted to an intensive care unit were prospectively studied using transthoracic echocardiography within the first 48 hours after admission and thereafter on the 7th-10th days. Echocardiographic variables of biventricular function, including the E/e' ratio, were compared between survivors and non-survivors.
A total of 99 echocardiograms (53 at admission and 46 between days 7 - 10) were performed on 53 patients with a mean age of 74 (SD 13) years. Systolic and diastolic dysfunction was present in 14 (26%) and 42 (83%) patients, respectively, and both types of dysfunction were present in 12 (23%) patients. The E/e' ratio, an index of diastolic dysfunction, was the best predictor of hospital mortality according to the area under the ROC curve (0.71) and was an independent predictor of outcome, as determined by multivariate analysis (OR = 1.36 [1.05 - 1.76], p = 0.02).
In septic patients admitted to an intensive care unit, echocardiographic systolic dysfunction is not associated with increased mortality. In contrast, diastolic dysfunction is an independent predictor of outcome.