Abstract
Rev Bras Ter Intensiva. 2013;25(4):327-333
DOI 10.5935/0103-507X.20130055
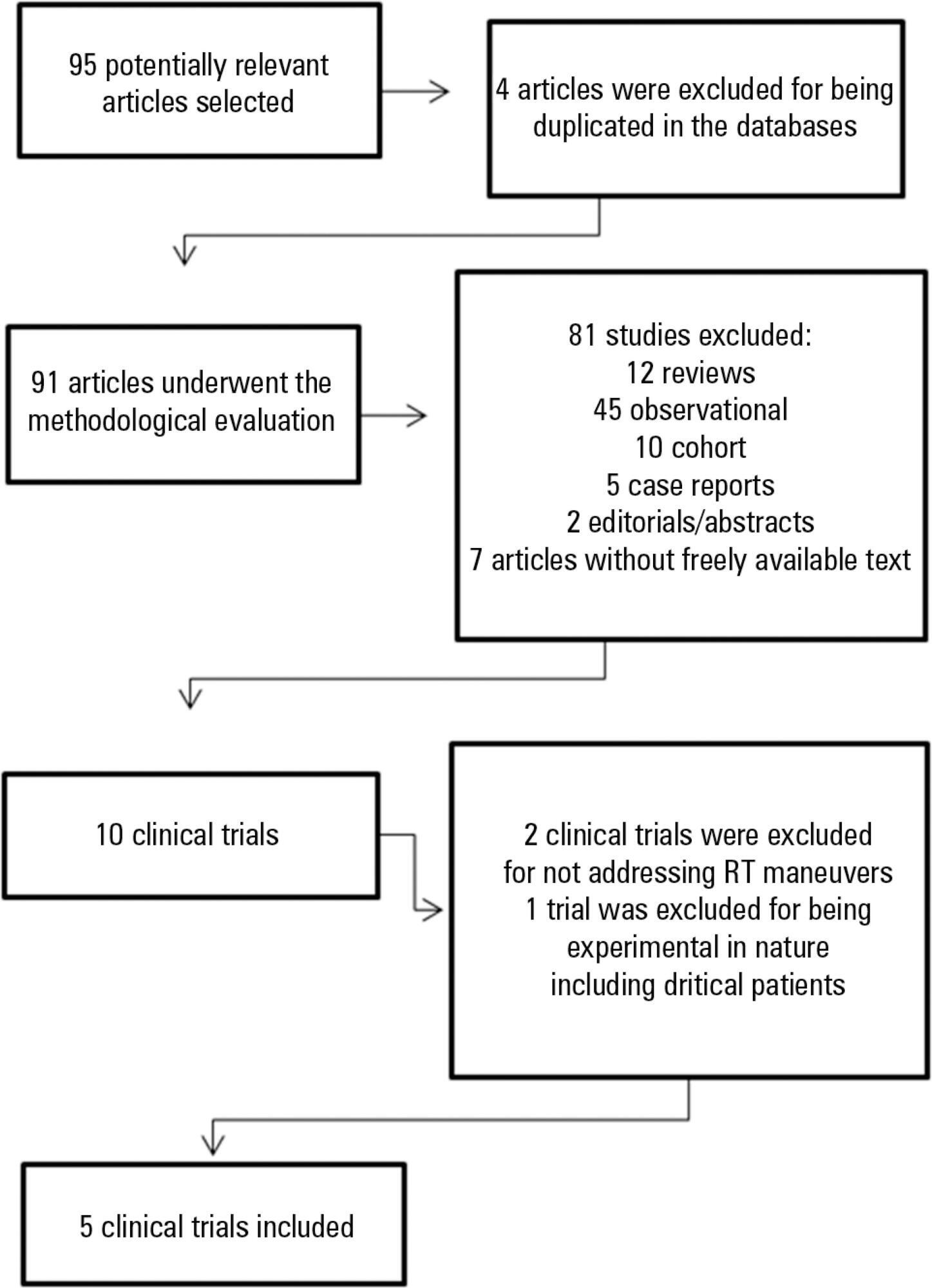
To analyze the outcomes of increased or decreased intracranial pressure and/or the decrease in cerebral perfusion pressure resulting from respiratory physiotherapy on critically ill patients admitted to the intensive care unit.
Through a systematic review of the literature, clinical trials published between 2002 and 2012 were selected. The search involved the LILACS, SciELO, MedLine and PEDro databases using the keywords "physical therapy", "physiotherapy", "respiratory therapy" and "randomized controlled trials" combined with the keyword "intracranial pressure".
In total, five studies, including a total of 164 patients between 25 and 65 years of age, reporting that respiratory physiotherapy maneuvers significantly increased intracranial pressure without changing the cerebral perfusion pressure were included. The articles addressed several techniques including vibration, vibrocompression, tapping, postural drainage, and the endotracheal aspiration maneuver. All patients required invasive mechanical ventilation.
Respiratory physiotherapy leads to increased intracranial pressure. Studies suggest that there are no short-term hemodynamic or respiratory repercussions or changes in the cerebral perfusion pressure. However, none of the studies evaluated the clinical outcomes or ensured the safety of the maneuvers.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):230-235
DOI 10.1590/S0103-507X2012000300005
OBJECTIVE: This study established the incidence and primary causes of unplanned extubation in newborns in the neonatal intensive care units of the Hospital Sofia Feldman, Belo Horizonte (Minas Gerais). METHODS: This retrospective study was conducted between July 1, 2009 and April 30, 2010. Unplanned extubations and their primary causes were assessed using an adverse events form. The following variables were assessed: gender, corrected age, present weight, duration of mechanical ventilation time, and motives/causes of the event on the day of the unplanned extubation event. RESULTS: Fifty-four unplanned extubations occurred, which corresponded to an incidence of 1.0 event/100 days of mechanical ventilation. This rate was higher among newborns with a corrected age of 30 to 36 weeks and weight < 1,000 g. The primary causes of unplanned extubations included patient agitation, inappropriate handling of patients during the performance of procedures, and inappropriate fixation and positioning of the endotracheal tube. CONCLUSION: The incidence of unplanned extubation in the investigated neonatal intensive care units was low during the study period compared to previously reported data. Nevertheless, the assessment of the quality of procedures, the continuous follow-up of newborns, and the monitoring of the causes of extubation are required to further reduce this incidence.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):119-129
DOI 10.1590/S0103-507X2012000200005
Developing guidelines for the role of the physiotherapist in neonatal and pediatric intensive care units is essential because these professionals are responsible for the rehabilitation of critically ill patients. Rehabilitation includes the evaluation and prevention of functional kinetic alterations, application of treatment interventions (respiratory and/or motor physiotherapy), control and application of medical gases, care of mechanical ventilation, weaning and extubation, tracheal gas insufflation, inflation/deflation of the endotracheal cuff protocol, and surfactant application, aiming to allow patients to have a full recovery and return to their functional activities. In this article, we present guidelines that are intended to guide the physiotherapist in some of the prevention/treatment interventions in respiratory therapy (airway clearance, lung expansion, position in bed, airway suction, drug inhalation, and cough assist), which help in the rehabilitation process of newborns and children in intensive care units during mechanical ventilation and up to 12 hours following extubation.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):190-198
DOI 10.1590/S0103-507X2011000200012
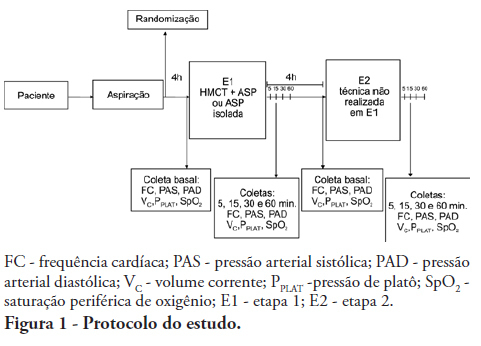
OBJECTIVES: To evaluate the effects of the manual hyperinflation with thoracic compression (MHTC) maneuver on the clearance of secretions, pulmonary mechanics, hemodynamics and oxygenation in mechanically ventilated patients. METHODS: This was a controlled, crossover study that included twenty patients who were under invasive ventilation for more than 48 hours. Four hours after the last airway suctioning procedure, the patients underwent the study interventions, Suction alone or MHTC plus Suction, in sequence at four hour intervals. The sequence order for the procedures was established by randomization. Data were collected before, during and 5, 15, 30 and 60 minutes after each intervention. The suctioned secretions were collected and weighed. RESULTS: No significant differences between the procedures were found regarding tidal volume, plateau pressure and pulmonary compliance (p>0.05). The hemodynamic variables showed increased pressures and heart rate during the procedures and returned to baseline values five minutes after the end of the procedure (p≤0.001). No significant hemodynamic differences were seen between the interventions (p>0.05). For the duration of the study, oxygen saturation was 99% with only two exceptions during the MHTC + Suction procedure, where saturation was 98% (p<0.05). No significant differences were observed between the techniques regarding the weight of the suctioned secretion. CONCLUSION: The results suggest that MHTC, as performed in this study, adds no benefit with respect to oxygenation optimization, pulmonary mechanics and clearance of secretions. However, the MHTC maneuver did not result in hemodynamic changes when compared to the suctioning procedure alone.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):186-191
DOI 10.1590/S0103-507X2010000200013
OBJECTIVES: To evaluate the applicability of the bag squeezing and zeep maneuvers in mechanically ventilated patients. METHODS: Twenty stable mechanically ventilated patients were studied. All patients were randomly allocated to either bag squeezing techinique followed by zeep maneuver, or the reversed sequence. Each group crossed to the other sequence four hours later. Heart rate, respiratory rate, peripheral oxygen saturation and blood pressure were measured before, during and after each technique use. The suctioned secretions were collected and measured. The data were analyzed by pairwise statistical analysis for inter-group comparisons, and ANOVA for each group results analysis. RESULTS: The heart rate was significantly increased, from 92.6 ± 18.3 bpm to 99.8 ± 18.5 bpm and the peripheral oxygen saturation significantly decreased from 96.9 ± 3.0% to 94.5 ± 4.3% during the bag squeezing maneuver, although the values remained within the normal range. No significant changes were seen for the zeep maneuver. Peripheral oxygen saturation during the maneuvers was found to change when the techniques were compared. No differences were found for the suctionedsecretions amounts. CONCLUSION: The results suggest that both techniques are feasible as they cause few hemodynamic changes, and both are effective for bronchial secretions removal.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):85-91
DOI 10.1590/S0103-507X2010000100014
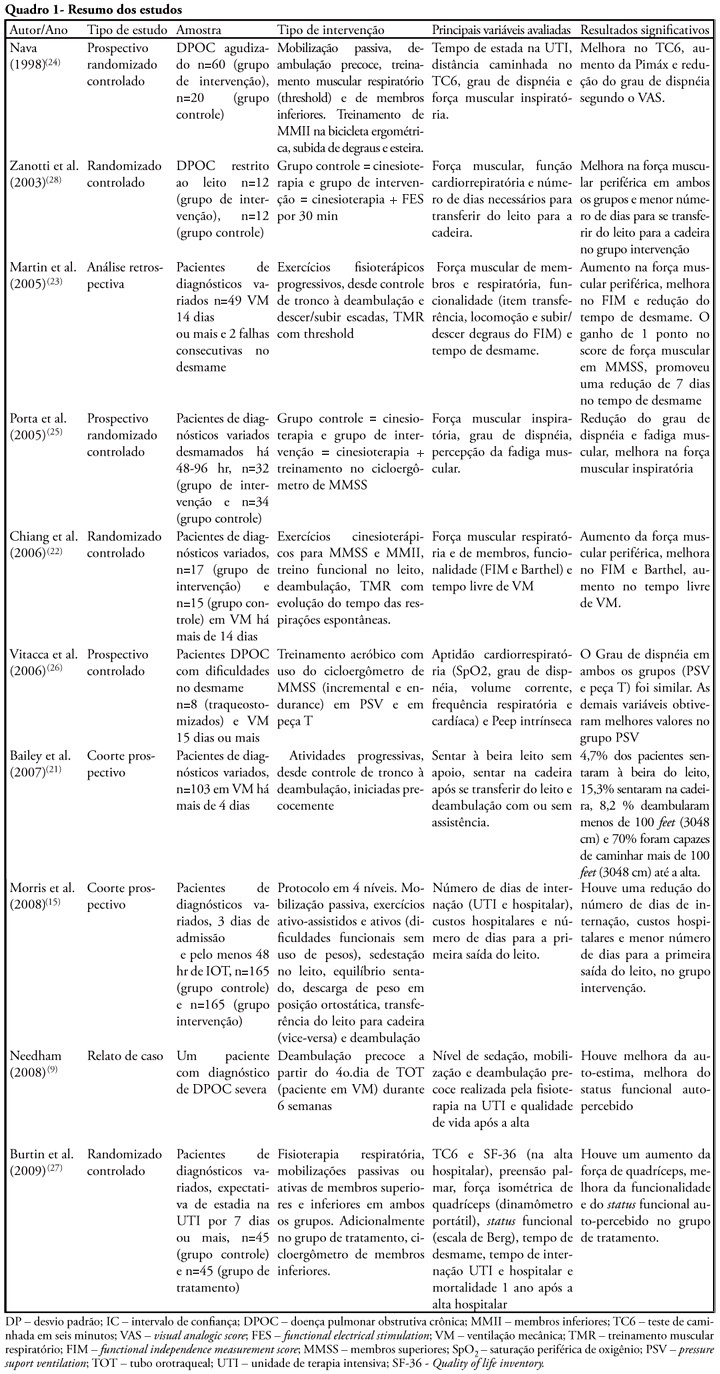
The development of critical patient-related generalized weakness is a common complication in patients admitted to an intensive care unit. The reduced muscle strength increases the time for weaning, hospitalization, the risk of infections and consequent mortality. Physiotherapy is used in these patients as a resource for the prevention of muscle weakness, atrophy and functional capacity recovery. The aim of this study was to review the literature regarding the use of exercise alone in intensive care units staying patients. Literature searches were performed using the electronic databases Medline, LILACS, CINAHL, Cochrane, High Wire Press and SciELO, from January 1998 to July 2009 and book chapters, using keywords including "critical illness", "cinesiotherapy", "physical therapy", "physiotherapy", "exercises", "training", "force", "active mobilization", "mobilization", "ICU", "rehabilitation", "mobility", "muscle strength" and "weakness". Despite the lack of studies and methodological diversity of studies found, confirming the use of exercise alone as a therapeutic resource, its use, including early seems an alternative to prevent and reverse muscle weakness intensive care unit ICU-acquired.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):27-32
DOI 10.1590/S0103-507X2010000100006
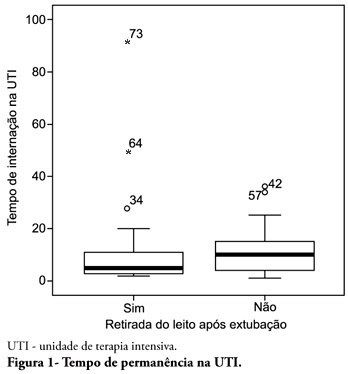
OBJECTIVE: To describe the withdrawal of the bed frequency in mechanic ventilation patients and its impact on mortality and length of stay in the intensive care unit. METHODS: This was a retrospective cohort study in mechanical ventilation patients. Clinical and epidemiological variables, withdrawal of bed related motor therapy, intensive care unit length of stay and mortality were evaluated. RESULTS: We studied 91 patients, mean age of 62.5± 18.8 years, predominantly female (52%) and mean intensive care unit length of stay of 07 days (95% CI, 8-13 days). Considering the withdrawal of the bed or not, no difference was observed between groups regarding length of stay in intensive care unit. Patients who were withdrawn of bed had a lower clinical severity. Their mortality rate was 29.7%. The not withdrawn of bed group had higher both actual and expected mortality. CONCLUSIONS: Patients withdrawn of bed following mechanical ventilation discontinuation showed lower mortality. It is suggested that early intensive care unit mobilization and withdrawal of bed should be stimulated.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):40-46
DOI 10.1590/S0103-507X2010000100008
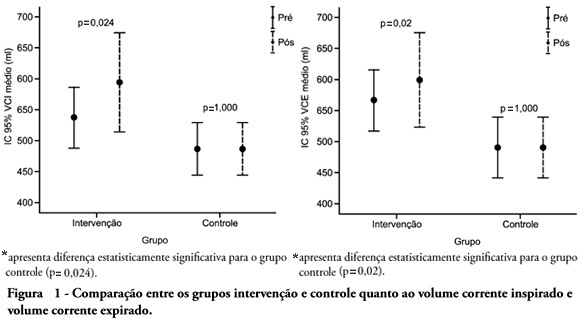
OBJECTIVE: To verify the effects of manual hyperinflation maneuver associated with positive end expiratory pressure in coronary artery bypass grafting patients. METHODS: This was a randomized trial, conducted from August 2007 to July 2008 in the intensive care unit of the Hospital Luterano (ULBRA). The patients were divided in the groups intervention - with manual hyperinflation plus positive end expiratory pressure - and controlThe ventilatory variables were measured before and after the manual hyperinflation. The t Student's test was used for independent and paired samples as well as Fisher's exact test and McNemar's Chi-square test with 0.05 significance level. RESULTS: Eighteen patients were included. The mean age was 64± 11 years and 55.6% were female. The inspired tidal volume was 594± 112ml in the intervention group and 487± 51ml in the control group (p=0.024) and the expired tidal volume was 598± 105ml in the intervention group and 490± 58ml in the control group (p=0.02). The mean pre-maneuver static pulmonary compliance in the intervention group was 41.6± 12.1 ml/cmH2O and post maneuver it was 47.4± 16.6 ml/cmH2O (p=0.03). There was no significant between groups difference in the following variables: oxygen peripheral saturation, oxygen arterial pressure, extubation time and radiological changes. CONCLUSION: The results show that the manual hyperinflation associated with positive end expiratory pressure maneuver trends to promote increased lung volumes and static compliance, however these findings require further confirmation.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)