Abstract
Rev Bras Ter Intensiva. 2019;31(1):27-33
DOI 10.5935/0103-507X.20190006
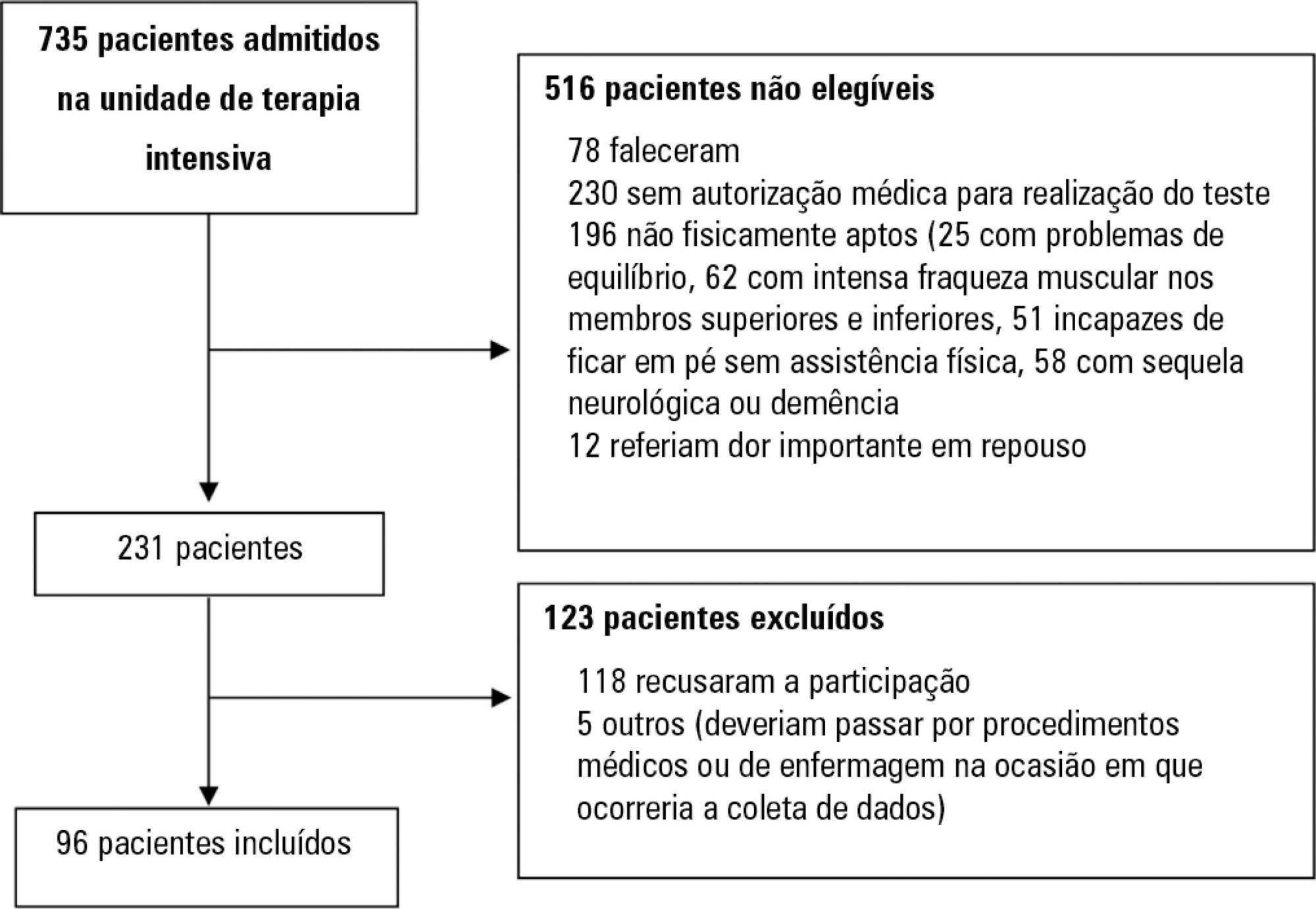
Assess the Five Times Sit-to-Stand Test safety and clinimetric properties in older patients hospitalized in an intensive care unit.
Test safety was assessed according to the incidence of adverse events and through hemodynamic and respiratory data. Additionally, reliability properties were investigated using the intraclass correlation coefficients, standard error of measurement, standard error percentage change, Altman-Bland plot and a survival agreement plot.
The overall suitability of the Five Times Sit-to-Stand Test was found to be low, with 29.8% meeting the inclusion criteria. Only 44% of the hospitalized patients who met the inclusion criteria performed the test, with no need for discontinuation in any patient. Heart rate (79.7 ± 10.2bpm/86.6 ± 9.7bpm; p = 0.001) and systolic blood pressure (118 ± 21.4mmHg/129 ± 21.5mmHg; p = 0.031) were the only variables that presented a significant statistical increase, with no evidence of exacerbated response to the test. Additionally, no adverse events were reported from participating and both test-retest and interrater reliability were high (intraclass correlation coefficient ≥ 0.99).
The Five Times Sit-to-Stand Test was proven to be safe and to have excellent reliability. Its clinical use, however, may be restricted to high-functioning older adults in hospital settings.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):39-46
DOI 10.5935/0103-507X.20190005
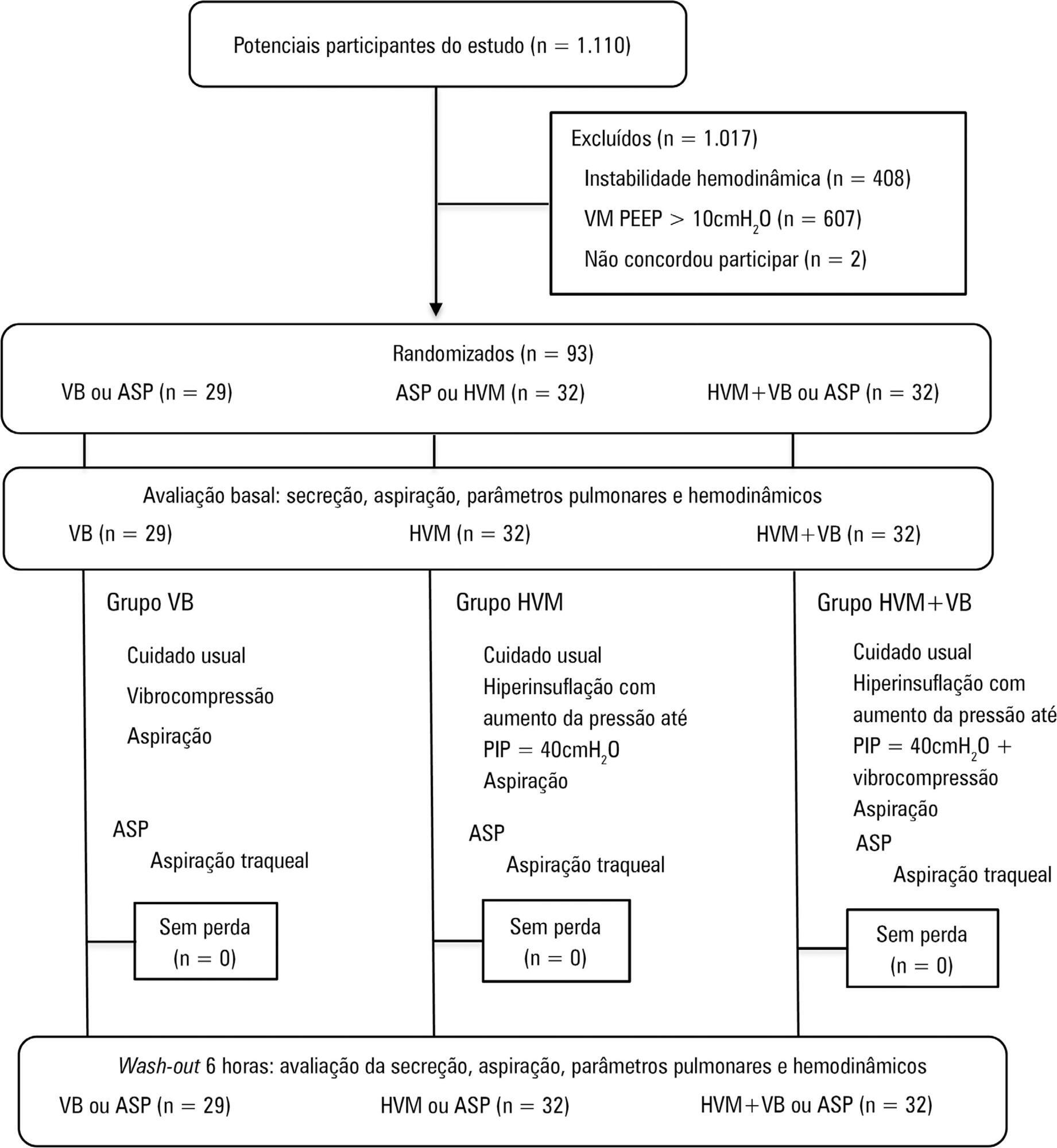
To compare the effects of vibrocompression and hyperinflation with mechanical ventilator techniques alone and in combination (hyperinflation with mechanical ventilator + vibrocompression) on the amount of aspirated secretion and the change in hemodynamic and pulmonary parameters.
A randomized clinical trial with critically ill patients on mechanical ventilation conducted in the intensive care unit of a university hospital. The patients were randomly allocated to receive one of the bronchial hygiene techniques for 10 minutes (vibrocompression or hyperinflation with mechanical ventilator or hyperinflation with mechanical ventilator + vibrocompression). Afterwards, the patients were again randomly allocated to receive either the previous randomly allocated technique or only tracheal aspiration. The weight of aspirated secretions (in grams), ventilatory mechanics and cardiopulmonary data before and after the application of the techniques were analyzed. The tracheal reintubation frequency and time and mortality on mechanical ventilation were also evaluated.
A total of 93 patients (29 vibrocompression, 32 hyperinflation with mechanical ventilator and 32 hyperinflation with mechanical ventilator + vibrocompression) on mechanical ventilation for more than 24 hours were included. The hyperinflation with mechanical ventilator + vibrocompression group was the only one that presented a significant increase in aspirated secretions compared to tracheal aspiration alone [0.7g (0.1 - 2.5g) versus 0.2g (0.0 - 0.6g), p value = 0.006].
Compared to tracheal aspiration alone, the combination of hyperinflation with mechanical ventilator + vibrocompression techniques was most efficient for increasing the amount of aspirated secretions.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):187-194
DOI 10.5935/0103-507X.20180037
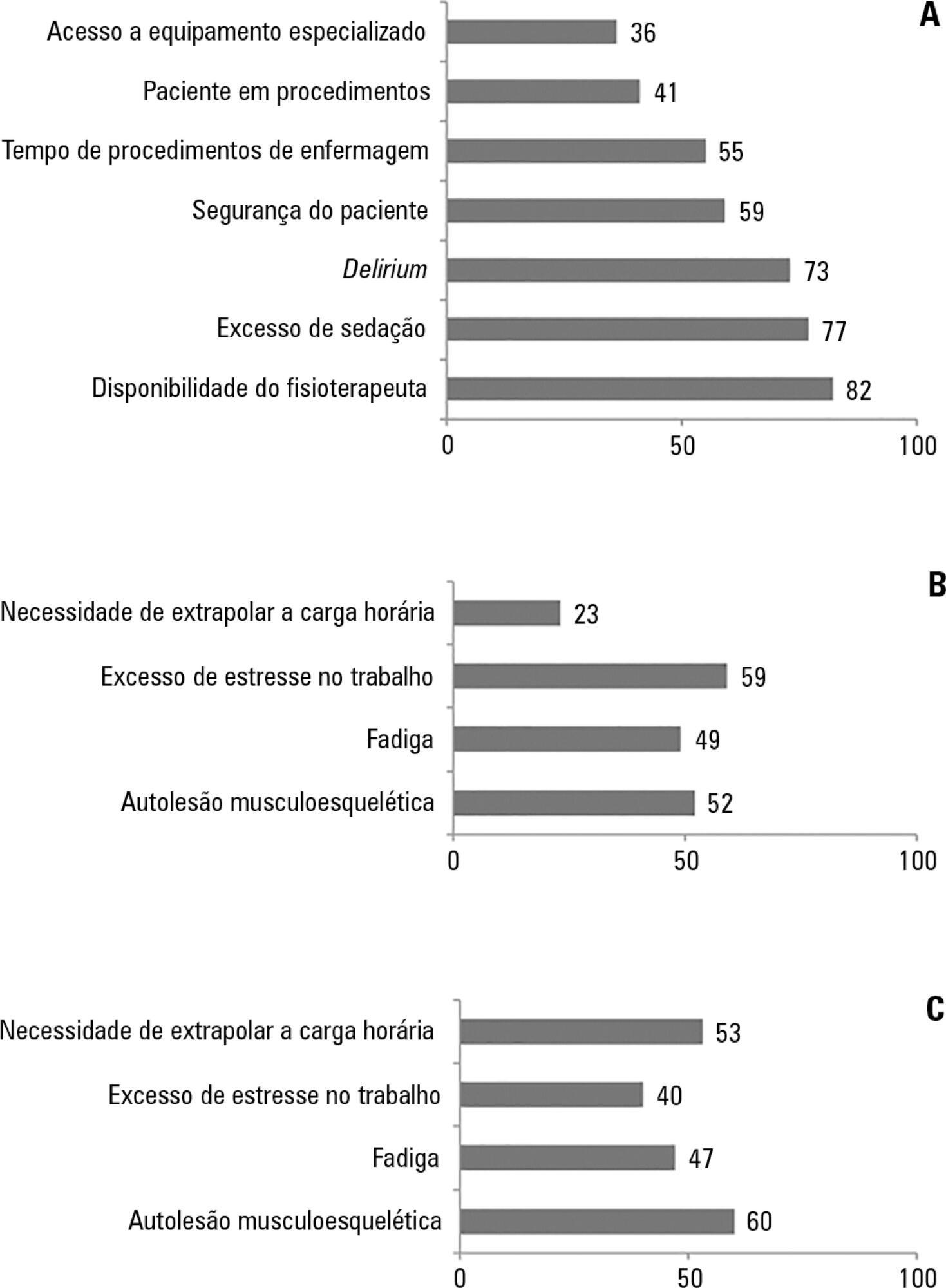
To investigate the knowledge of multi-professional staff members about the early mobilization of critically ill adult patients and identify attitudes and perceived barriers to its application.
A cross-sectional study was conducted during the second semester of 2016 with physicians, nursing professionals and physical therapists from six intensive care units at two teaching hospitals. Questions were answered on a 5-point Likert scale and analyzed as proportions of professionals who agreed or disagreed with statements. The chi-square and Fisher's exact tests were used to investigate differences in the responses according to educational/training level, previous experience with early mobilization and years of experience in intensive care units.
The questionnaire was answered by 98 out of 514 professionals (response rate: 19%). The acknowledged benefits of early mobilization were maintenance of muscle strength (53%) and shortened length of mechanical ventilation (83%). Favorable attitudes toward early mobilization included recognition that its benefits for patients under mechanical ventilation exceed the risks for both patients and staff, that early mobilization should be routinely performed via nursing and physical therapy protocols, and readiness to change the parameters of mechanical ventilation and reduce sedation to facilitate the early mobilization of patients. The main barriers mentioned were the unavailability of professionals and time to mobilize patients, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
The participants were aware of the benefits of early mobilization and manifested attitudes favorable to its application. However, the actual performance of early mobilization was perceived as a challenge, mainly due to the lack of professionals and time, excessive sedation, delirium, risk of musculoskeletal self-injury and excessive stress at work.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):96-104
DOI 10.5935/0103-507X.20170014
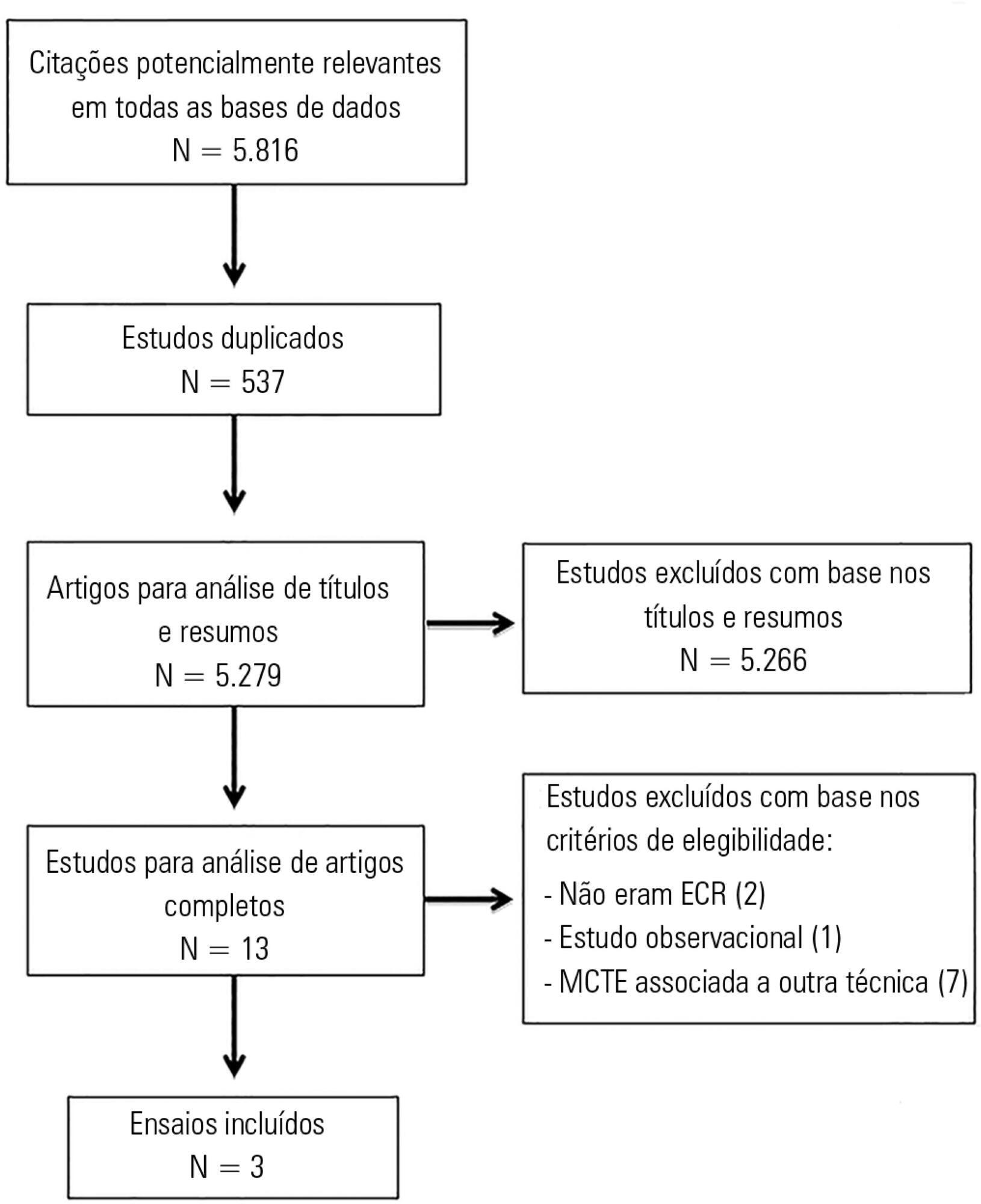
To review the literature on the effects of expiratory rib cage compression on ventilatory mechanics, airway clearance, and oxygen and hemodynamic indices in mechanically ventilated adults.
Systematic review with meta-analysis of randomized clinical trials in the databases MEDLINE (via PubMed), EMBASE, Cochrane CENTRAL, PEDro, and LILACS. Studies on adult patients hospitalized in intensive care units and under mechanical ventilation that analyzed the effects of expiratory rib cage compression with respect to a control group (without expiratory rib cage compression) and evaluated the outcomes static and dynamic compliance, sputum volume, systolic blood pressure, diastolic blood pressure, mean arterial pressure, heart rate, peripheral oxygen saturation, and ratio of arterial oxygen partial pressure to fraction of inspired oxygen were included. Experimental studies with animals and those with incomplete data were excluded.
The search strategy produced 5,816 studies, of which only three randomized crossover trials were included, totaling 93 patients. With respect to the outcome of heart rate, values were reduced in the expiratory rib cage compression group compared with the control group [-2.81 bpm (95% confidence interval [95%CI]: -4.73 to 0.89; I2: 0%)]. Regarding dynamic compliance, there was no significant difference between groups [-0.58mL/cmH2O (95%CI: -2.98 to 1.82; I2: 1%)]. Regarding the variables systolic blood pressure and diastolic blood pressure, significant differences were found after descriptive evaluation. However, there was no difference between groups regarding the variables secretion volume, static compliance, ratio of arterial oxygen partial pressure to fraction of inspired oxygen, and peripheral oxygen saturation.
There is a lack of evidence to support the use of expiratory rib cage compression in routine care, given that the literature on this topic offers low methodological quality and is inconclusive.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):7-13
DOI 10.5935/0103-507X.20140002
To evaluate the role of quality indicators and adverse events registering in the quality assessment of intensive care physiotherapy and to evaluate the impact of implementing protocolized care and professional training in the quality improvement process.
A prospective before-after study was designed to assess 15 indicators of the quality of care. Baseline compliance and adverse events were collected before and after the implementation of treatment protocols and staff training.
Eighty-nine patients admitted, being 48 in the pre-intervention period and 41 in the post-intervention period with a total of 1246 and 1191 observations respectively. Among the indicators related to the global population, there was a significant improvement in chest x-ray control, multidisciplinary rounds and shift changes as well as in compliance with these decisions. Indicators related to the population under mechanical ventilation, obtained by direct observation at bedside, showed a significant improvement in the compliance with the tidal volume of 6-8mL/Kg, plateau pressure <30cmH2O, adequate mechanical ventilation alarm setting, mechanical ventilation humidification control, adequate humidification line exchange and orotracheal tube position. Among the mechanical ventilation indicators collected through the physiotherapy records, there was significantly improved compliance with the predicted tidal volume registry and cuff pressure registry. There was a significant reduction in the number of adverse events. There was no impact on intensive care unit mortality, length of stay, duration of mechanical ventilation and ventilator-free days.
It is possible to measure the quality of physiotherapy care using indicators of quality control. The implementation of care protocols and training of the professionals can improve team performance.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):163-168
DOI 10.5935/0103-507X.20140024
To compare the effectiveness of the alveolar recruitment maneuver and the breath stacking technique with respect to lung mechanics and gas exchange in patients with acute lung injury.
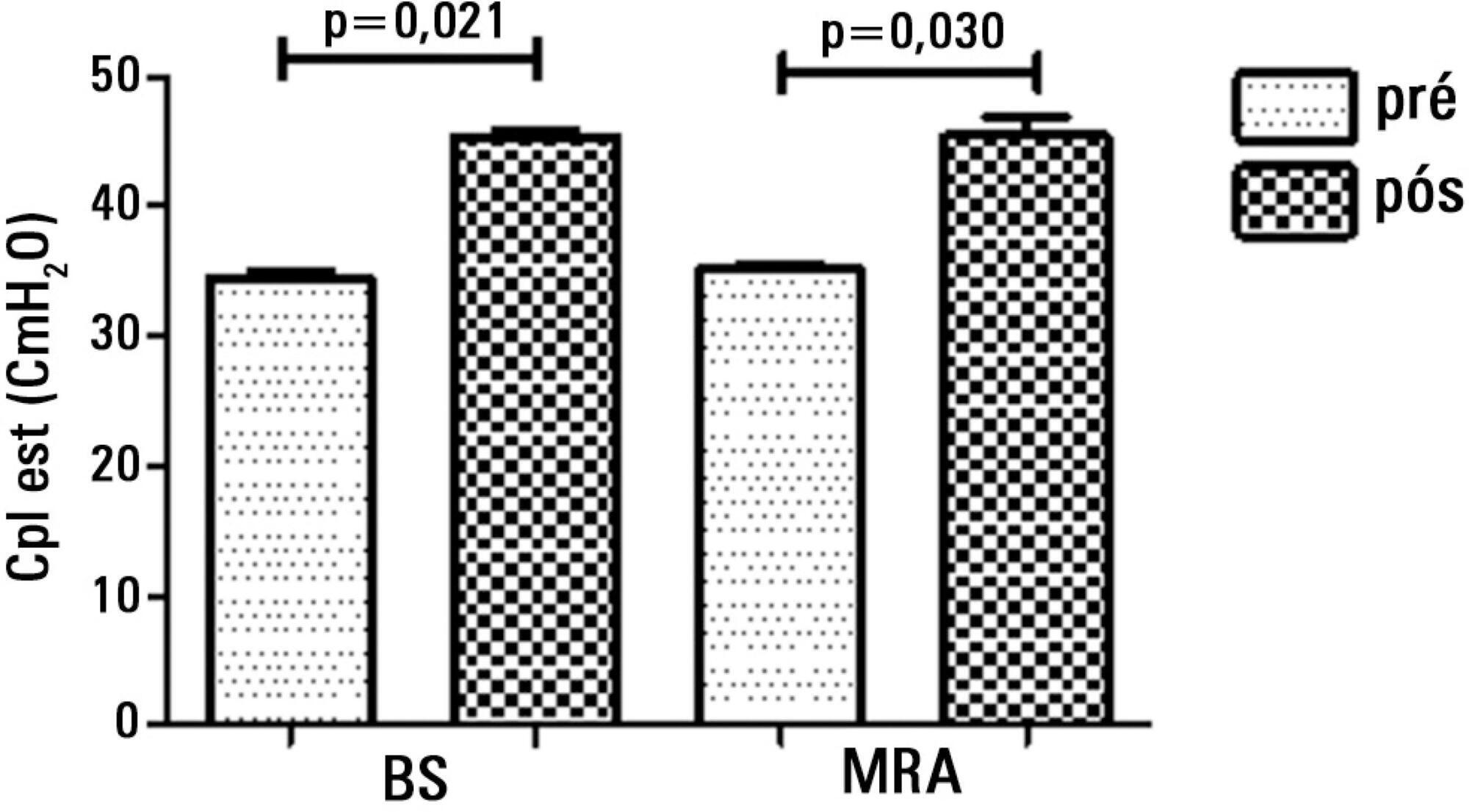
Thirty patients were distributed into two groups: Group 1 - breath stacking; and Group 2 - alveolar recruitment maneuver. After undergoing conventional physical therapy, all patients received both treatments with an interval of 1 day between them. In the first group, the breath stacking technique was used initially, and subsequently, the alveolar recruitment maneuver was applied. Group 2 patients were initially subjected to alveolar recruitment, followed by the breath stacking technique. Measurements of lung compliance and airway resistance were evaluated before and after the use of both techniques. Gas analyses were collected before and after the techniques were used to evaluate oxygenation and gas exchange.
Both groups had a significant increase in static compliance after breath stacking (p=0.021) and alveolar recruitment (p=0.03), but with no significant differences between the groups (p=0.95). The dynamic compliance did not increase for the breath stacking (p=0.22) and alveolar recruitment (p=0.074) groups, with no significant difference between the groups (p=0.11). The airway resistance did not decrease for either groups, i.e., breath stacking (p=0.91) and alveolar recruitment (p=0.82), with no significant difference between the groups (p=0.39). The partial pressure of oxygen increased significantly after breath stacking (p=0.013) and alveolar recruitment (p=0.04), but there was no significant difference between the groups (p=0.073). The alveolar-arterial O2 difference decreased for both groups after the breath stacking (p=0.025) and alveolar recruitment (p=0.03) interventions, and there was no significant difference between the groups (p=0.81).
Our data suggest that the breath stacking and alveolar recruitment techniques are effective in improving the lung mechanics and gas exchange in patients with acute lung injury.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):57-64
DOI 10.5935/0103-507X.20140009
To describe the characteristics of physical therapy assistance to newborns and to provide a profile of physical therapists working in intensive care units in the city of São Paulo, Brazil.
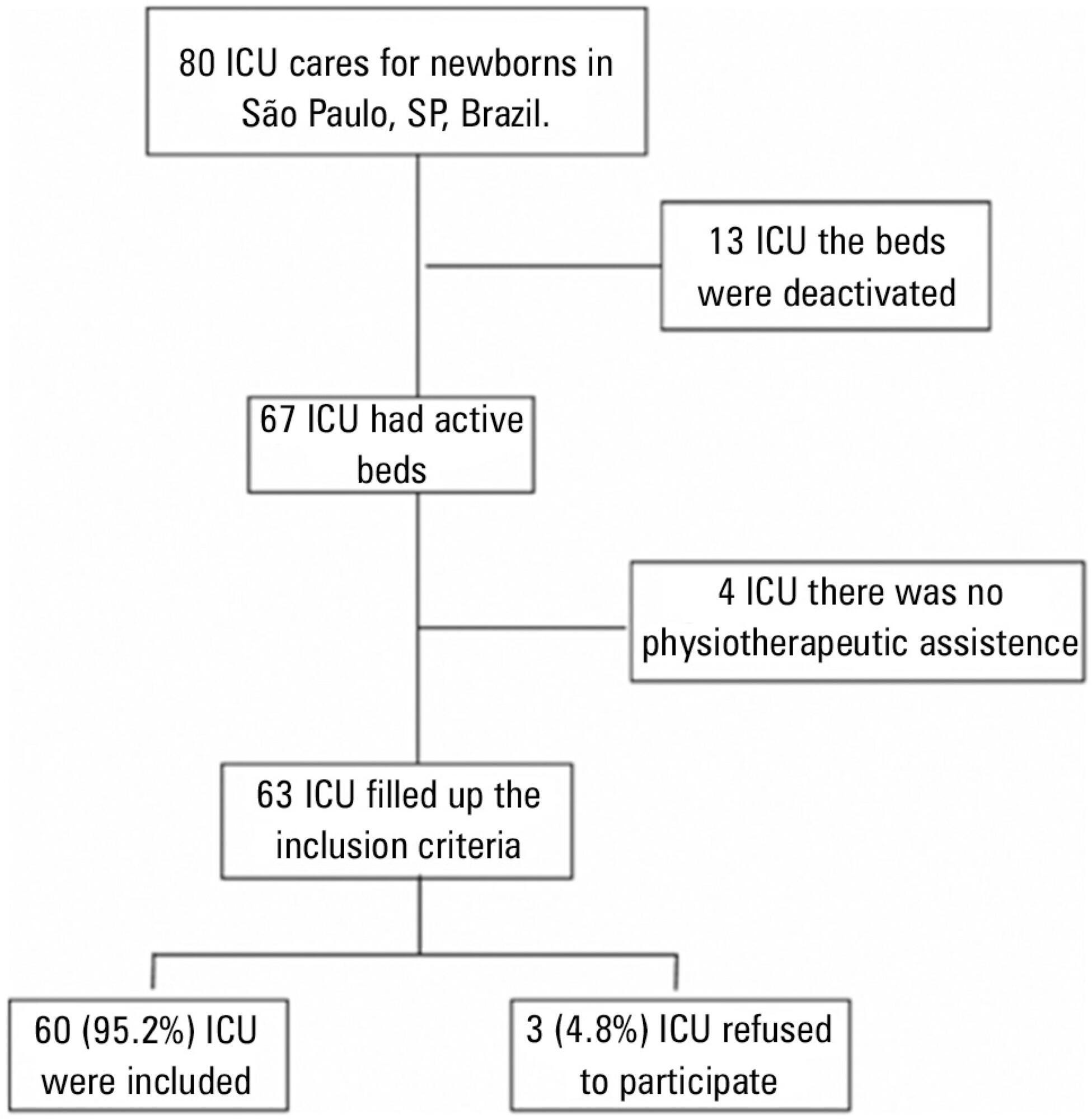
This cross-sectional study was conducted in every hospital in São Paulo city that had at least one intensive care unit bed for newborns registered at the National Registry of Health Establishments in 2010. In each unit, three types of physical therapists were included: an executive who was responsible for the physical therapy service in that hospital (chief-physical therapists), a physical therapist who was responsible for the physical therapy assistance in the neonatal unit (reference-physical therapists), and a randomly selected physical therapist who was directly involved in the neonatal care (care-physical therapists).
Among the 67 hospitals eligible for the study, 63 (94.0%) had a physical therapy service. Of those hospitals, three (4.8%) refused to participate. Thus, 60 chief-PTs, 52 reference-physical therapists, and 44 care-physical therapists were interviewed. During day shifts, night shifts, and weekends/holidays, there were no physical therapists in 1.7%, 45.0%, and 13.3% of the intensive care units, respectively. Physical therapy assistance was available for 17.8±7.2 hours/day, and each physical therapist cared for 9.4±2.6 newborns during six working hours. Most professionals had completed at least one specialization course.
Most neonatal intensive care units in the city of São Paulo had physical therapists working on the day shift. However, other shifts had incomplete staff with less than 18 hours of available physical therapy assistance per day.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):258-262
DOI 10.5935/0103-507X.20130043
To perform an assessment of the available literature on manual hyperinflation as a respiratory physical therapy technique used in pediatric patients, with the main outcome of achieving airway clearance.
We reviewed articles included in the Lilacs (Latin American and Caribbean Literature on Health Sciences/Literatura Latino Americana e do Caribe em Ciências da Saúde), Cochrane Library, Medline (via Virtual Health Library and PubMed), SciELO (Scientific Electronic Library), and PEDro (Physiotherapy Evidence Database) databases from 2002 to 2013 using the following search terms: "physiotherapy (techniques)", "respiratory therapy", "intensive care", and "airway clearance". The selected studies were classified according to the level of evidence and grades of recommendation (method of the Oxford Centre for Evidence-Based Medicine) by two examiners, while a third examiner repeated the search and analysis and checked the classification of the articles.
Three articles were included for analysis, comprising 250 children (aged 0 to 16 years). The main diagnoses were acute respiratory failure, recovery following heart congenital disease and upper abdominal surgery, bone marrow transplantation, asthma, tracheal reconstruction, brain injury, airway injury, and heterogeneous lung diseases. The studies were classified as having a level of evidence 2C and grade of recommendation C.
Manual hyperinflation appeared useful for airway clearance in the investigated population, although the evidence available in the literature remains insufficient. Therefore, controlled randomized studies are needed to establish the safety and efficacy of manual hyperinflation in pediatric patients. However, manual hyperinflation must be performed by trained physical therapists only.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)