Abstract
Rev Bras Ter Intensiva. 2022;34(1):131-140
DOI 10.5935/0103-507X.20220007-en
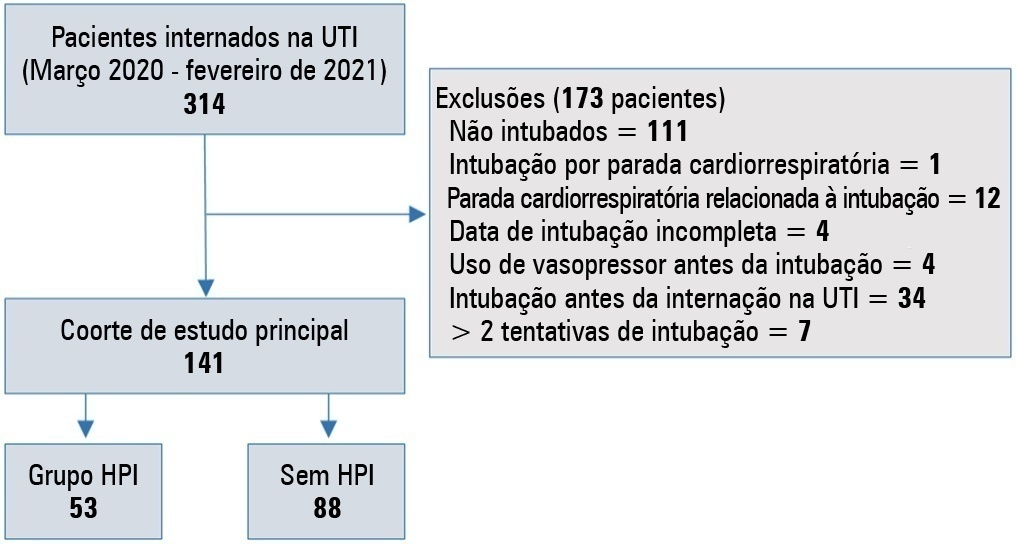
To evaluate the incidence of risk factors for postintubation hypotension in critically ill patients with COVID-19.
We conducted a retrospective study of 141 patients with COVID-19 who were intubated in the intensive care unit. Postintubation hypotension was defined as the need for any vasopressor dose at any time within the 60 minutes following intubation. Patients with intubation-related cardiac arrest and hypotension before intubation were excluded from the study.
Of the 141 included patients, 53 patients (37.5%) had postintubation hypotension, and 43.6% of the patients (n = 17) were female. The median age of the postintubation hypotension group was 75.0 (interquartile range: 67.0 - 84.0). In the multivariate analysis, shock index ≥ 0.90 (OR = 7.76; 95%CI 3.14 - 19.21; p < 0.001), albumin levels < 2.92g/dL (OR = 3.65; 95%CI 1.49 - 8.96; p = 0.005), and procalcitonin levels (OR = 1.07, 95%CI 1.01 - 1.15; p = 0.045) were independent risk factors for postintubation hypotension. Hospital mortality was similar in patients with postintubation hypotension and patients without postintubation hypotension (92.5% versus 85.2%; p = 0.29).
The incidence of postintubation hypotension was 37.5% in critically ill COVID-19 patients. A shock index ≥ 0.90 and albumin levels < 2.92g/dL were independently associated with postintubation hypotension. Furthermore, a shock index ≥ 0.90 may be a practical tool to predict the increased risk of postintubation hypotension in bedside scenarios before endotracheal intubation. In this study, postintubation hypotension was not associated with increased hospital mortality in COVID-19 patients.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):565-571
DOI 10.5935/0103-507X.20210073
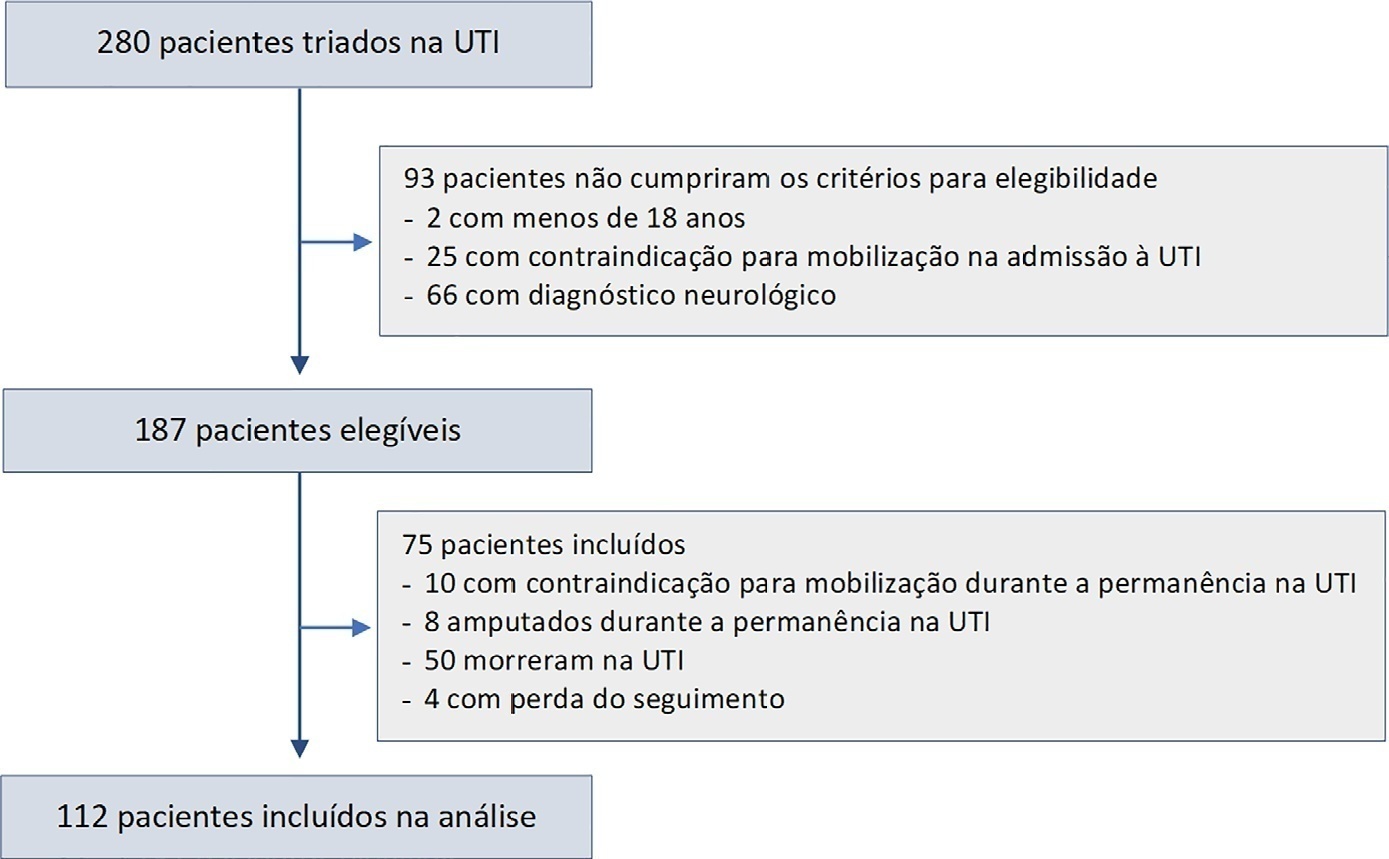
To identify the factors associated with functional status decline in intensive care unit patients.
In this prospective study, patients in an intensive care unit aged 18 years or older without neurological disease or contraindications to mobilization were included. The exclusion criteria were patients who spent fewer than 4 days in the intensive care unit or died during the study period. Accelerometry was used to assess the physical activity level of patients. We recorded age, SAPS 3, days on mechanical ventilation, drugs used, comorbidities, and functional status after intensive care unit discharge. After intensive care unit discharge, the patients were assigned to a dependent group or an independent group according to their Barthel index. Logistic regression and the odds ratio were used in the analyses.
Sixty-three out of 112 included patients were assigned to the dependent group. The median Charlson comorbidity index was 3 (2 - 4). The mean SAPS 3 score was 53 ± 11. The patients spent 94 ± 4% of the time spent in inactivity and 4.8 ± 3.7% in light activities. The odds ratio showed that age (OR = 1.08; 95%CI 1.04 - 1.13) and time spent in inactivity (OR = 1.38; 95%CI 1.14 - 1.67) were factors associated with functional status decline. Time spent in light activity was associated with a better functional status (OR = 0.73; 95%CI 0.60 - 0.89).
Age and time spent in inactivity during intensive care unit stay are associated with functional status decline. On the other hand, performing light activities seems to preserve the functional status of patients.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):592-599
DOI 10.5935/0103-507X.20210086
To translate and culturally adapt the Pediatric Intensive Care Unit-Quality of Dying and Death questionnaire into Brazilian Portuguese.
This was a cross-cultural adaptation process including conceptual, cultural, and semantic equivalence steps comprising three stages. Stage 1 involved authorization to perform the translation and cultural adaptation. Stage 2 entailed independent translation from English into Brazilian Portuguese, a synthesis of the translation, back-translation, and an expert panel. Stage 3 involved a pretest conducted with family caregivers and a multidisciplinary team.
The evaluation by the expert panel resulted in an average agreement of 0.8 in relation to semantic, cultural, and conceptual equivalence. The pretests of both versions of the questionnaire showed that the participants had adequate comprehension regarding the ease of understanding the items and response options.
After going through the process of translation and cultural adaptation, the Pediatric Intensive Care Unit-Quality of Dying and Death caregiver and multidisciplinary team versions were considered culturally adapted, with both groups having a good understanding of the items. The questionnaires include relevant items to evaluate the process of death and dying in the intensive care setting, and suggest changes in care centered on patients and especially family caregivers, given the finitude of their children.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
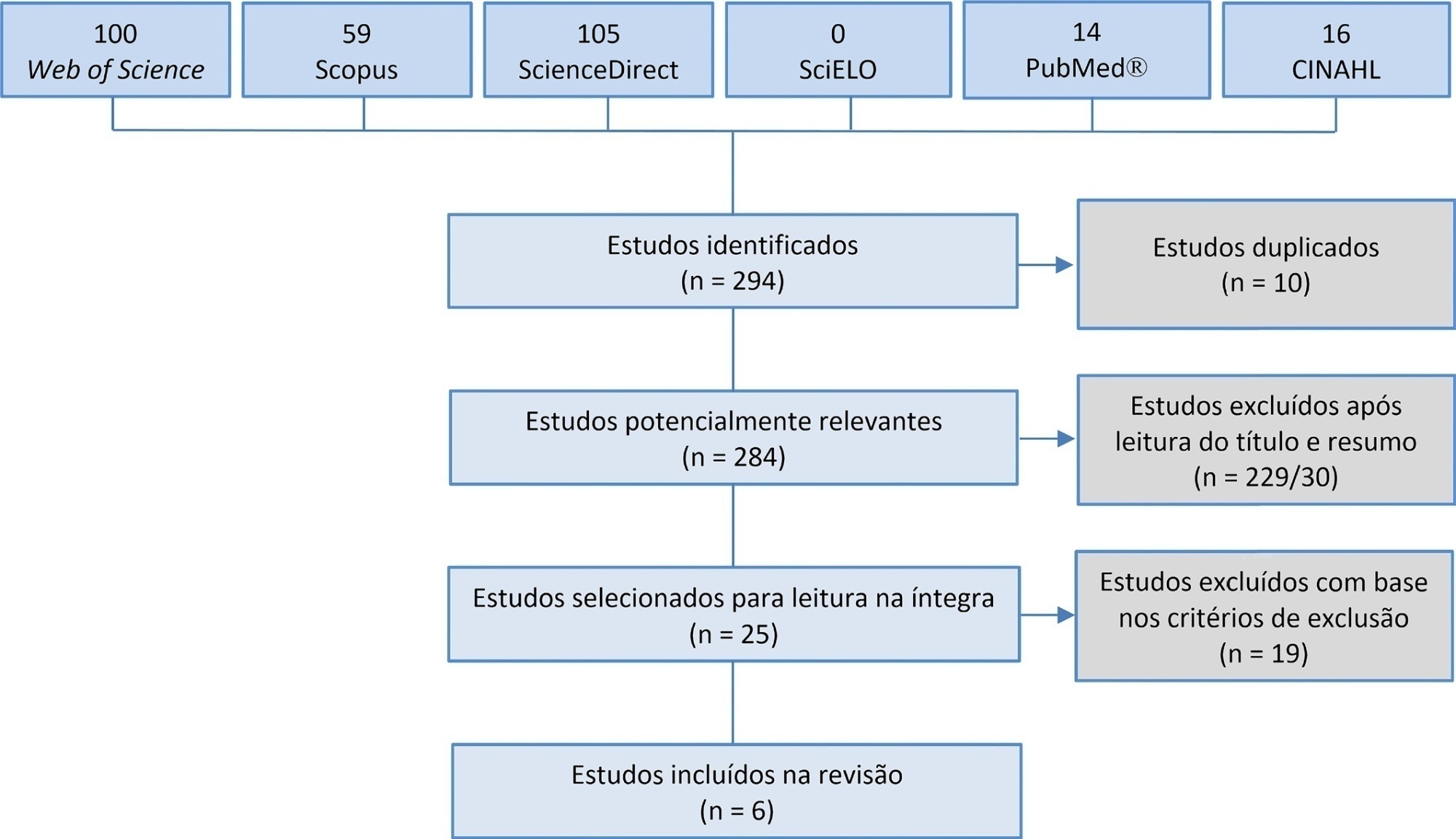
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):624-634
DOI 10.5935/0103-507X.20210088
To identify the clinical and epidemiological profile of adult intensive care units in Brazil.
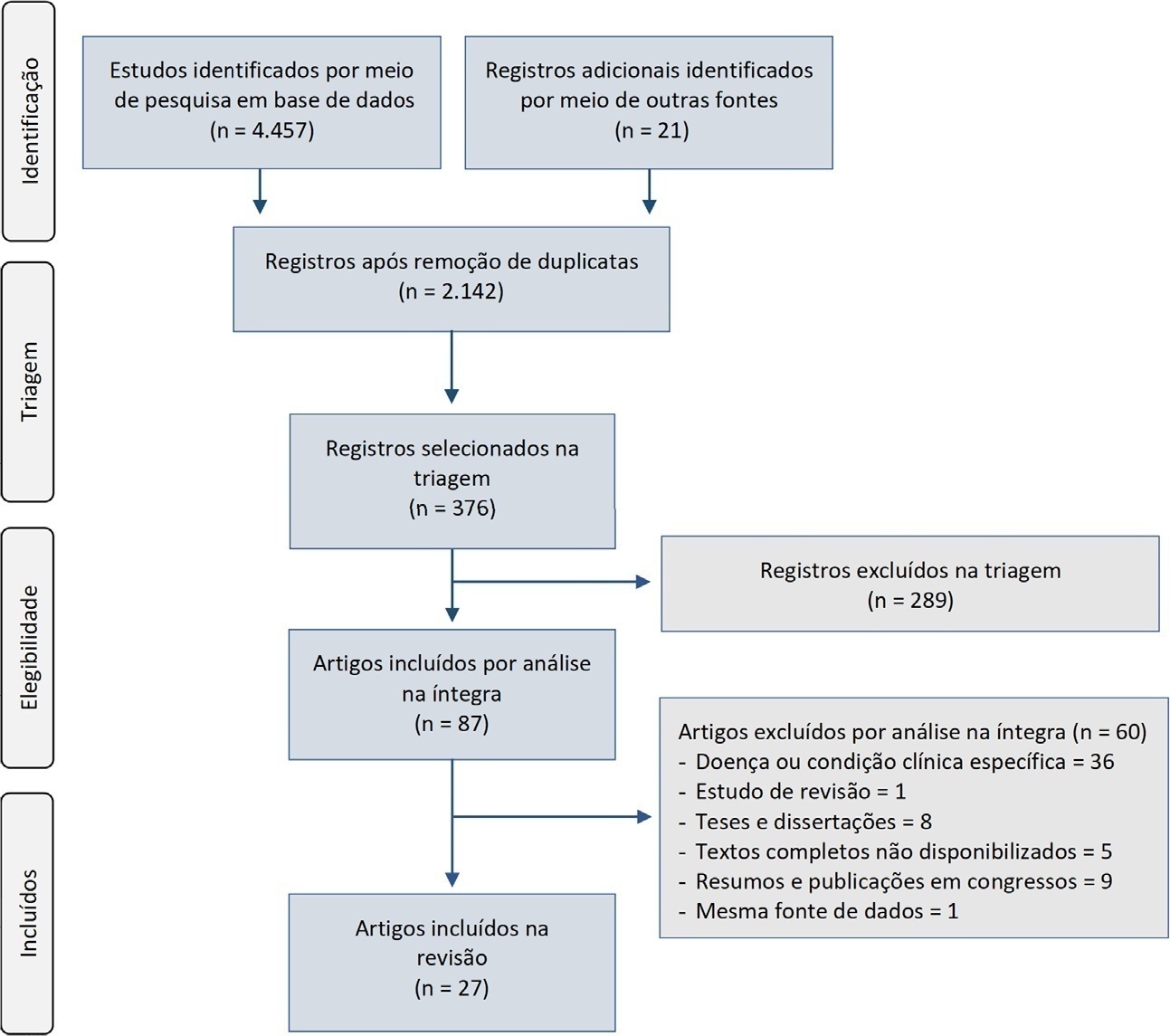
A systematic review was performed using a comprehensive strategy to search PubMed®, Embase, SciELO, and the Biblioteca Virtual em Saúde. The eligibility criteria for this review were observational studies that described the epidemiological and/or clinical profile of critically ill patients admitted to Brazilian intensive care units and were published between 2007 and 2020.
From the 4,457 identified studies, 27 were eligible for this review, constituting an analysis of 113 intensive care units and a final sample of 75,280 individuals. There was a predominance of male and elderly patients. Cardiovascular diseases were the main cause of admission to the intensive care unit. The Acute Physiology and Chronic Health Evaluation II score was the most widely used disease severity assessment system. The length of stay and mortality in the intensive care unit varied widely between institutions.
These results can help guide the planning and organization of intensive care units, providing support for decision-making and the implementation of interventions that ensure better quality patient care.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):635-639
DOI 10.5935/0103-507X.20210089
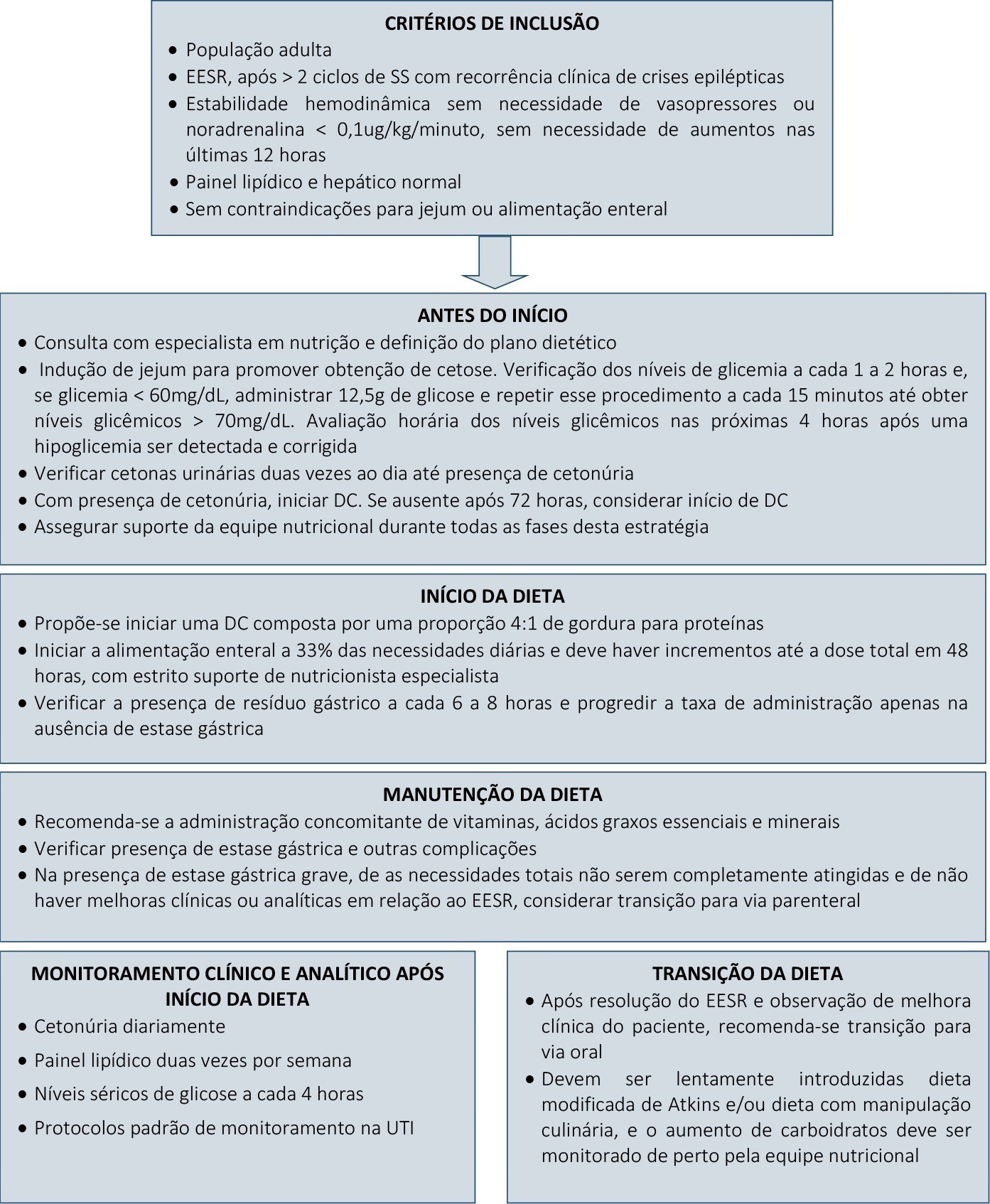
Super-refractory status epilepticus is defined as seizures that persist or reemerge in the setting of an intravenous anesthetic infusion for more than 24 hours. In recent years, attention has been driven to the potential benefits of a ketogenic diet in the management of these patients. However, the specific role of this strategy in the adult population, as well as its underlying mechanism of action and optimal time for the initiation and management of complications, remain widely debatable. We report a case series of three patients admitted to an intensive care unit due to super-refractory status epilepticus who were managed with a ketogenic diet and propose a clinical approach to its initiation, transition, and management of clinical intercurrences.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):346-352
DOI 10.5935/0103-507X.20210053
To assess pulmonary embolism incidence, its relationship with D-dimer levels and other possible associated factors in addition to anticoagulation and contrast medium adverse effects.
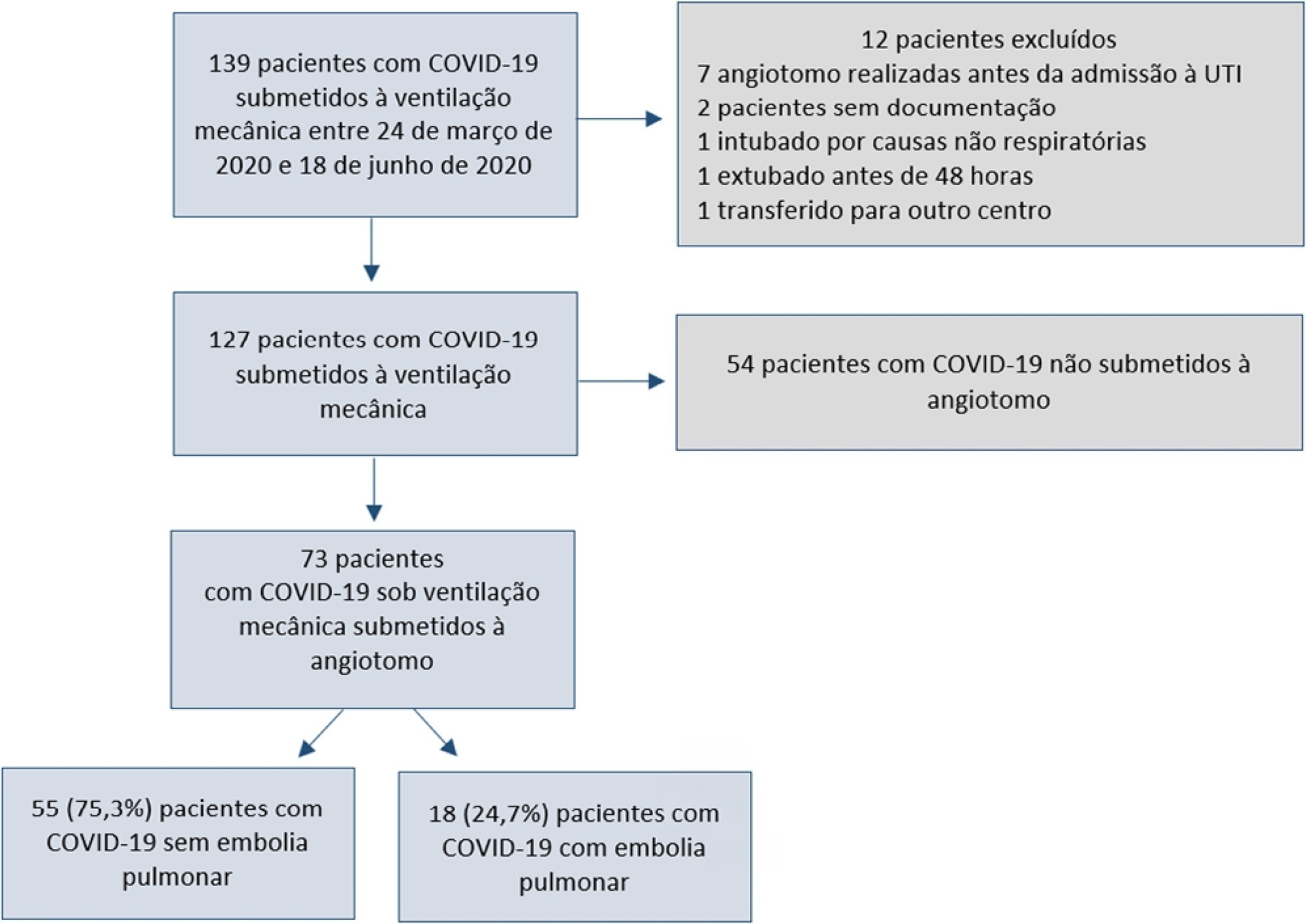
A retrospective observational cohort study at a Chilean public hospital was performed. Intensive care unit mechanically ventilated COVID-19 patients older than 18 years old between March and June 2020 were included. All patients received heparin thromboprophylaxis, which was increased to the anticoagulation dose with D-dimer greater than 3µg/mL.
A total of 127 patients were followed up, of whom 73 underwent pulmonary computed tomography angiography (mean age, 54 ± 12 years; 49 men). Sixty-two of the 73 patients (84.9%) received full anticoagulation before computed tomography angiography. In addition, 18 of the 73 patients had pulmonary embolism (24.7%). When comparing patients with and without pulmonary embolism, no significant differences were observed in age, sex, obesity, smoking, Wells and revised Geneva scores, D-dimer or mortality. Anticoagulant use was similar in both groups. Days from the start of anticoagulation until computed tomography angiography were significantly lower in the pulmonary embolism group (p = 0.002). Three patients presented post contrast-acute kidney injury (4.1%), and one patient had major bleeding.
Despite anticoagulation, one in four COVID-19 patients connected to mechanical ventilation and evaluated with pulmonary computed tomography angiography had pulmonary embolism. With a longer the delay in performing computed tomography angiography once empirical anticoagulation was started, significantly less pulmonary embolism was identified.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):353-361
DOI 10.5935/0103-507X.20210051
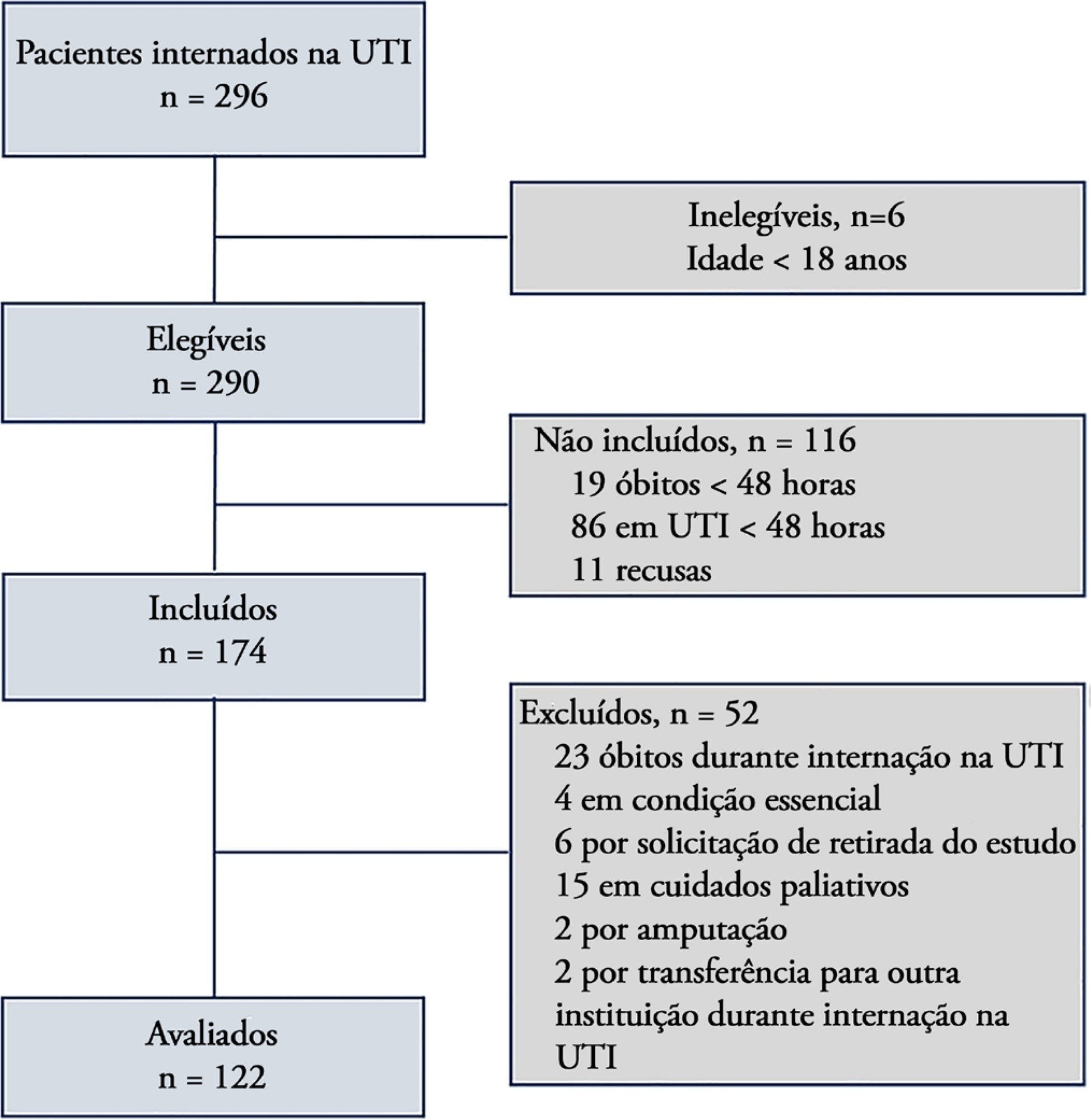
To translate and cross-culturally adapt the Early Rehabilitation Index to Brazilian Portuguese and validate the Early Rehabilitation Barthel Index for use in the intensive care unit to assess functional status.
The following steps were performed: preparation, translation, reconciliation, back-translation, revision, harmonization, pretesting, and psychometric evaluation. After this initial process, the Portuguese version was applied by two evaluators to patients hospitalized in the intensive care unit for at least 48 hours. The reliability of the scale was assessed by internal consistency, interrater reliability, and floor and ceiling effects. To measure construct validity, the Early Rehabilitation Barthel Index was correlated with instruments typically used to assess functional status in the intensive care unit.
A total of 122 patients with a median age of 56 (46.8 - 66) years participated in the study. The Early Rehabilitation Barthel Index had adequate reliability, with a Cronbach’s alpha coefficient of 0.65. The interrater reliability was excellent, with an intraclass correlation coefficient of 0.94 (95%CI 0.92 - 0.96), and agreement was moderate to excellent, with a kappa agreement index of 0.54 to 1.0. The floor and ceiling effects were minimal. The validity of the Early Rehabilitation Barthel Index was observed through its correlations with the total Perme score (rho = 0.72), the Functional Status Score for the ICU (rho = 0.77), the Physical Function in the Intensive Care Test score (rho = 0.69), and the Medical Research Council sum score (rho = 0.58), in addition to handgrip strength (rho = 0.58) and knee extensor strength measured by hand-held dynamometry (rho = 0.55), all with p < 0.001.
The adapted versions of the Early Rehabilitation Index for Brazilian Portuguese and, in its entirety, the Early Rehabilitation Barthel Index are reliable and valid for assessing the functional status of patients at discharge from the intensive care unit.