Abstract
Rev Bras Ter Intensiva. 2021;33(3):428-433
DOI 10.5935/0103-507X.20210068
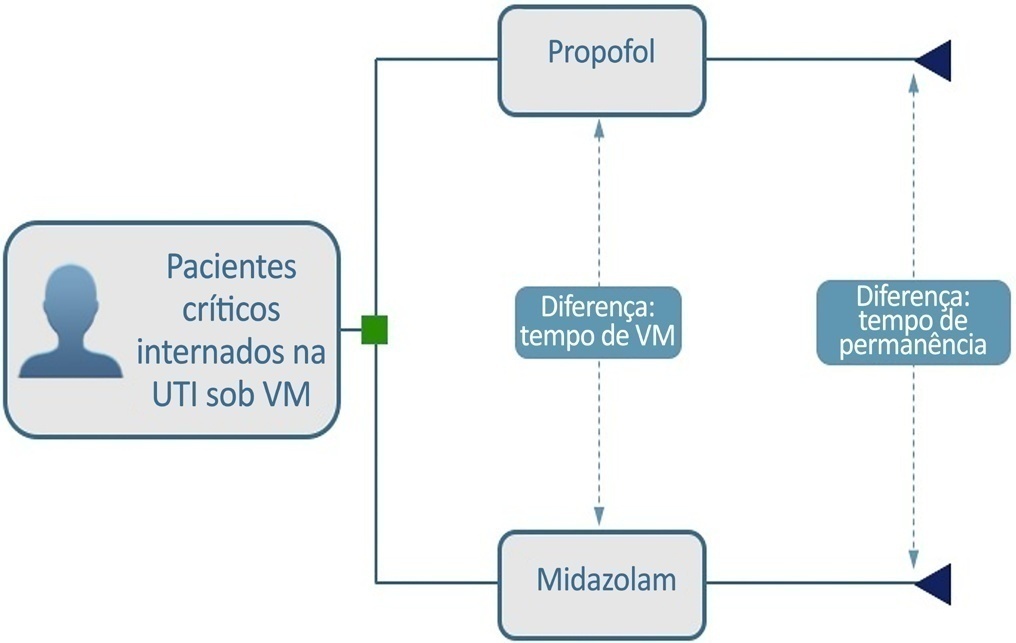
To build a cost-effectiveness model to compare the use of propofol versus midazolam in critically ill adult patients under mechanical ventilation.
We built a decision tree model for critically ill patients submitted to mechanical ventilation and analyzed it from the Brazilian private health care system perspective. The time horizon was that of intensive care unit hospitalization. The outcomes were cost-effectiveness per hour of intensive care unit stay avoided and cost-effectiveness per hour of mechanical ventilation avoided. We retrieved data for the model from a previous meta-analysis. We assumed that the cost of medication was embedded in the intensive care unit cost. We conducted univariate and probabilistic sensitivity analyses.
Mechanically ventilated patients using propofol had their intensive care unit stay and the duration of mechanical ventilation decreased by 47.97 hours and 21.65 hours, respectively. There was an average cost reduction of US$ 2,998.971 for propofol when compared to midazolam. The cost-effectiveness per hour of intensive care unit stay and mechanical ventilation avoided were dominant 94.40% and 80.8% of the time, respectively.
There was a significant reduction in costs associated with propofol use related to intensive care unit stay and duration of mechanical ventilation for critically ill adult patients.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):196-205
DOI 10.5935/0103-507X.20210027
To identify more severe COVID-19 presentations.
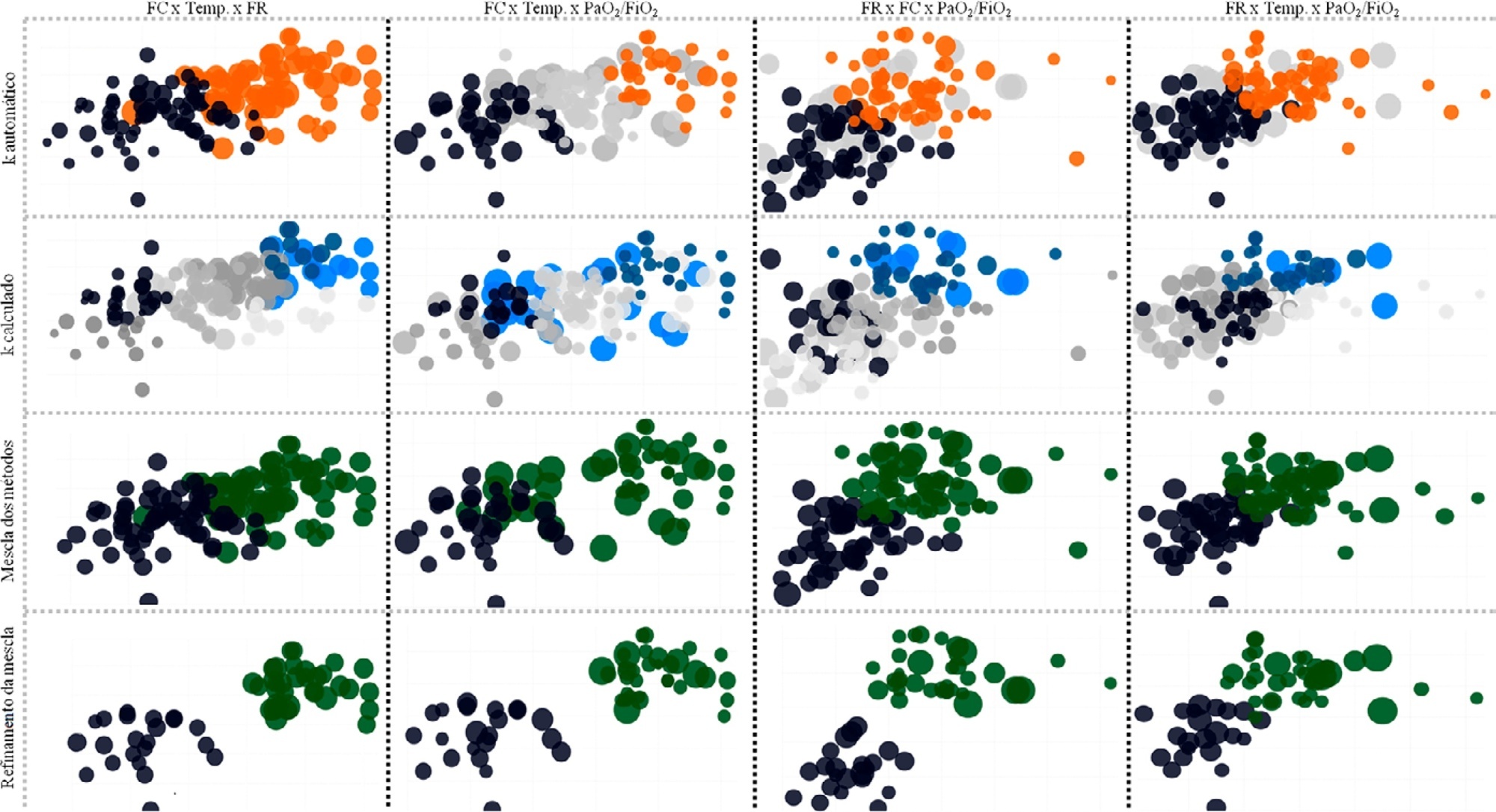
Consecutive intensive care unit-admitted patients were subjected to a stepwise clustering method.
Data from 147 patients who were on average 56 ± 16 years old with a Simplified Acute Physiological Score 3 of 72 ± 18, of which 103 (70%) needed mechanical ventilation and 46 (31%) died in the intensive care unit, were analyzed. From the clustering algorithm, two well-defined groups were found based on maximal heart rate [Cluster A: 104 (95%CI 99 - 109) beats per minute versus Cluster B: 159 (95%CI 155 - 163) beats per minute], maximal respiratory rate [Cluster A: 33 (95%CI 31 - 35) breaths per minute versus Cluster B: 50 (95%CI 47 - 53) breaths per minute], and maximal body temperature [Cluster A: 37.4 (95%CI 37.1 - 37.7)°C versus Cluster B: 39.3 (95%CI 39.1 - 39.5)°C] during the intensive care unit stay, as well as the oxygen partial pressure in the blood over the oxygen inspiratory fraction at intensive care unit admission [Cluster A: 116 (95%CI 99 - 133) mmHg versus Cluster B: 78 (95%CI 63 - 93) mmHg]. Subphenotypes were distinct in inflammation profiles, organ dysfunction, organ support, intensive care unit length of stay, and intensive care unit mortality (with a ratio of 4.2 between the groups).
Our findings, based on common clinical data, revealed two distinct subphenotypes with different disease courses. These results could help health professionals allocate resources and select patients for testing novel therapies.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):219-230
DOI 10.5935/0103-507X.20210029
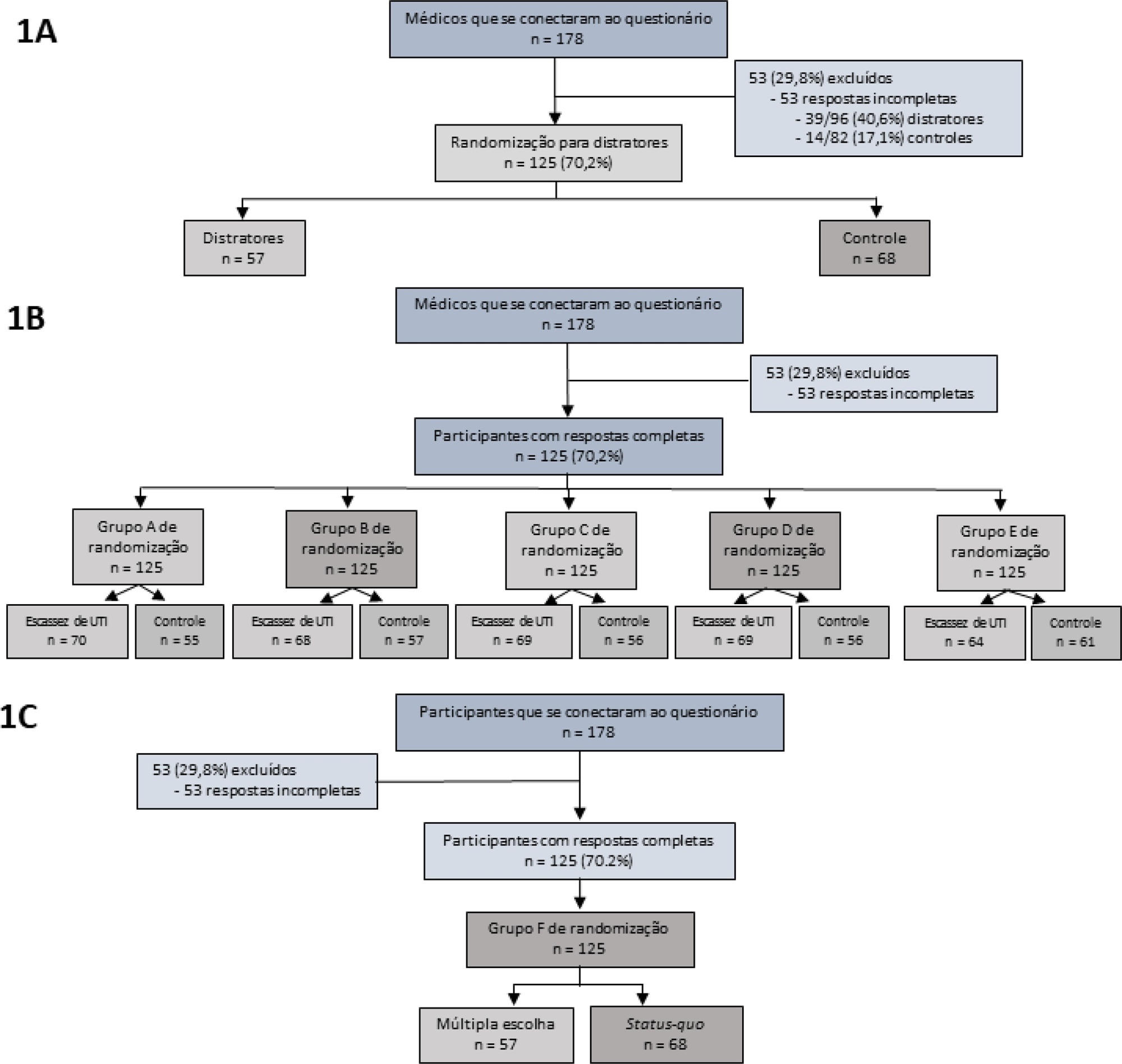
To assess the impact of intensive care unit bed availability, distractors and choice framing on intensive care unit admission decisions.
This study was a randomized factorial trial using patient-based vignettes. The vignettes were deemed archetypical for intensive care unit admission or refusal, as judged by a group of experts. Intensive care unit physicians were randomized to 1) an increased distraction (intervention) or a control group, 2) an intensive care unit bed scarcity or nonscarcity (availability) setting, and 3) a multiple-choice or omission (status quo) vignette scenario. The primary outcome was the proportion of appropriate intensive care unit allocations, defined as concordance with the allocation decision made by the group of experts.
We analyzed 125 physicians. Overall, distractors had no impact on the outcome; however, there was a differential drop-out rate, with fewer physicians in the intervention arm completing the questionnaire. Intensive care unit bed availability was associated with an inappropriate allocation of vignettes deemed inappropriate for intensive care unit admission (OR = 2.47; 95%CI 1.19 - 5.11) but not of vignettes appropriate for intensive care unit admission. There was a significant interaction with the presence of distractors (p = 0.007), with intensive care unit bed availability being associated with increased intensive care unit admission of vignettes inappropriate for intensive care unit admission in the distractor (intervention) arm (OR = 9.82; 95%CI 2.68 - 25.93) but not in the control group (OR = 1.02; 95%CI 0.38 - 2.72). Multiple choices were associated with increased inappropriate allocation in comparison to the omission group (OR = 5.18; 95%CI 1.37 - 19.61).
Intensive care unit bed availability and cognitive biases were associated with inappropriate intensive care unit allocation decisions. These findings may have implications for intensive care unit admission policies.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):231-242
DOI 10.5935/0103-507X.20210030
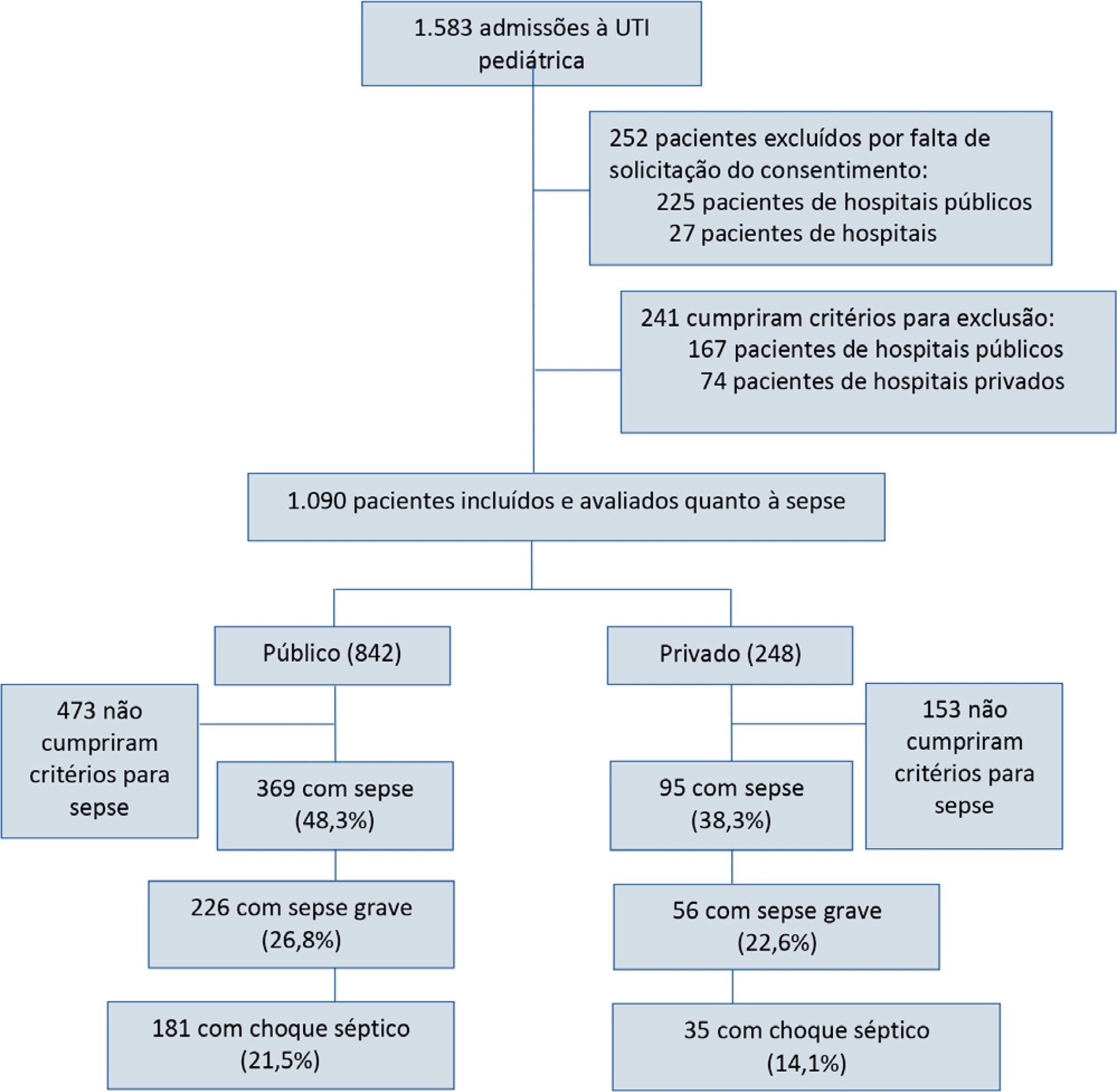
To report the prevalence and outcomes of sepsis in children admitted to public and private hospitals.
Post hoc analysis of the Latin American Pediatric Sepsis Study (LAPSES) data, a cohort study that analyzed the prevalence and outcomes of sepsis in critically ill children with sepsis on admission at 21 pediatric intensive care units in five Latin American countries.
Of the 464 sepsis patients, 369 (79.5%) were admitted to public hospitals and 95 (20.5%) to private hospitals. Compared to those admitted to private hospitals, sepsis patients admitted to public hospitals did not differ in age, sex, immunization status, hospital length of stay or type of admission but had higher rates of septic shock, higher Pediatric Risk of Mortality (PRISM), Pediatric Index of Mortality 2 (PIM 2), and Pediatric Logistic Organ Dysfunction (PELOD) scores, and higher rates of underlying diseases and maternal illiteracy. The proportion of patients admitted from pediatric wards and sepsis-related mortality were higher in public hospitals. Multivariate analysis did not show any correlation between mortality and the type of hospital, but mortality was associated with greater severity on pediatric intensive care unit admission in patients from public hospitals.
In this sample of critically ill children from five countries in Latin America, the prevalence of septic shock within the first 24 hours at admission and sepsis-related mortality were higher in public hospitals than in private hospitals. Higher sepsis-related mortality in children admitted to public pediatric intensive care units was associated with greater severity on pediatric intensive care unit admission but not with the type of hospital. New studies will be necessary to elucidate the causes of the higher prevalence and mortality of pediatric sepsis in public hospitals.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):243-250
DOI 10.5935/0103-507X.20210031
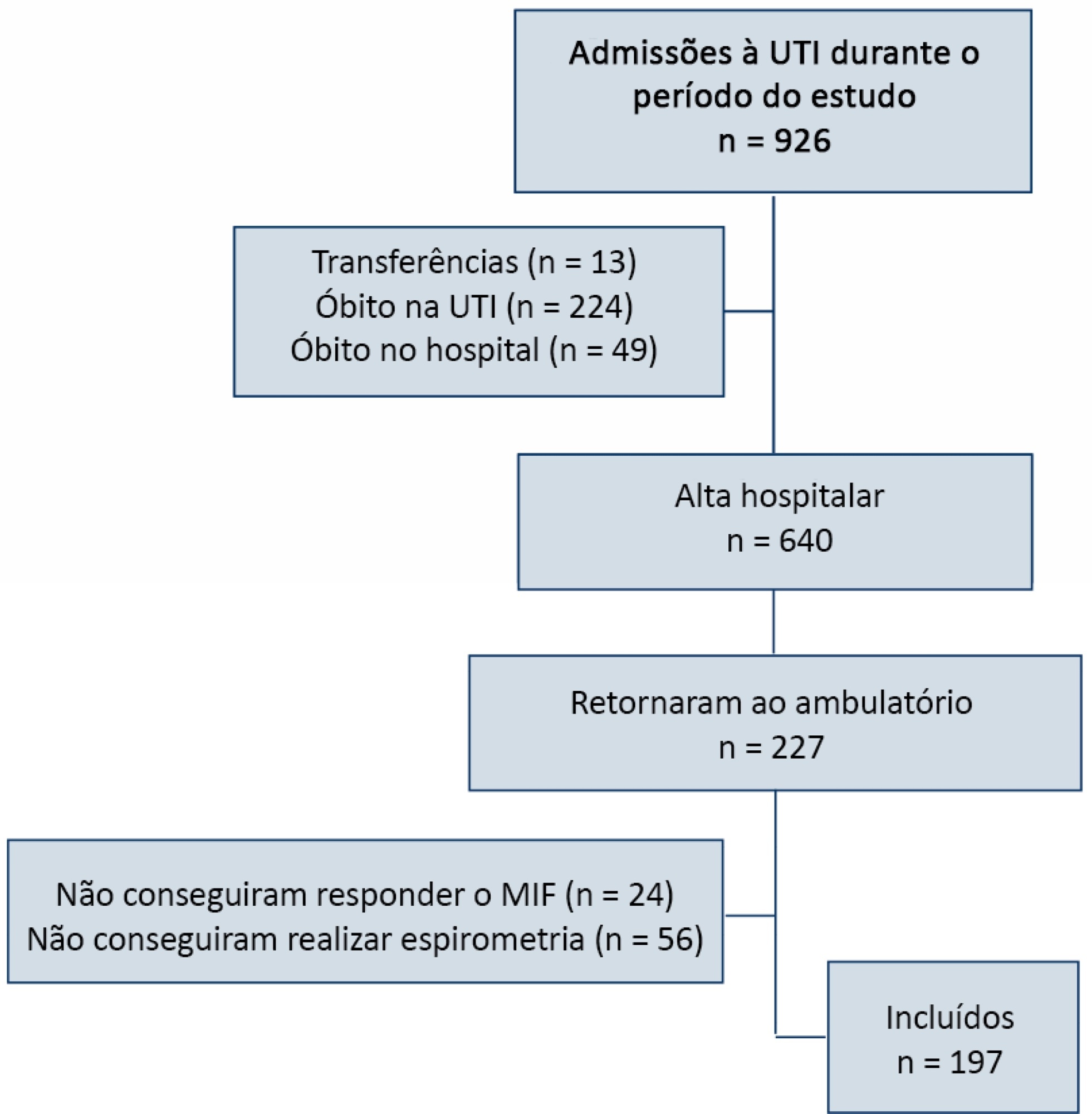
To relate functional independence to the degree of pulmonary impairment in adult patients 3 months after discharge from the intensive care unit.
This was a retrospective cohort study conducted in one adult intensive care unit and a multi-professional post-intensive care unit outpatient clinic of a single center. Patients admitted to the intensive care unit from January 2012 to December 2013 who underwent (3 months later) spirometry and answered the Functional Independence Measure Questionnaire were included.
Patients were divided into groups according to the classification of functional independence and spirometry. The study included 197 patients who were divided into greater dependence (n = 4), lower dependence (n = 12) and independent (n = 181) groups. Comparing the three groups, regarding the classification of the Functional Independence Measure, patients with greater dependence had higher Acute Physiology and Chronic Health Evaluation II and Sequential Organ Failure Assessment values at intensive care unit admission with more advanced age, more days on mechanical ventilation, and longer stay in the intensive care unit and hospital. The majority of patients presented with pulmonary impairment, which was the obstructive pattern observed most frequently. When comparing functional independence with pulmonary function, it was observed that the lower the functional status, the worse the pulmonary function, with a significant difference being observed in peak expiratory flow (p = 0.030).
The majority of patients who returned to the outpatient clinic 3 months after discharge had good functional status but did present with pulmonary impairment, which is related to the degree of functional dependence.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):261-265
DOI 10.5935/0103-507X.20210033
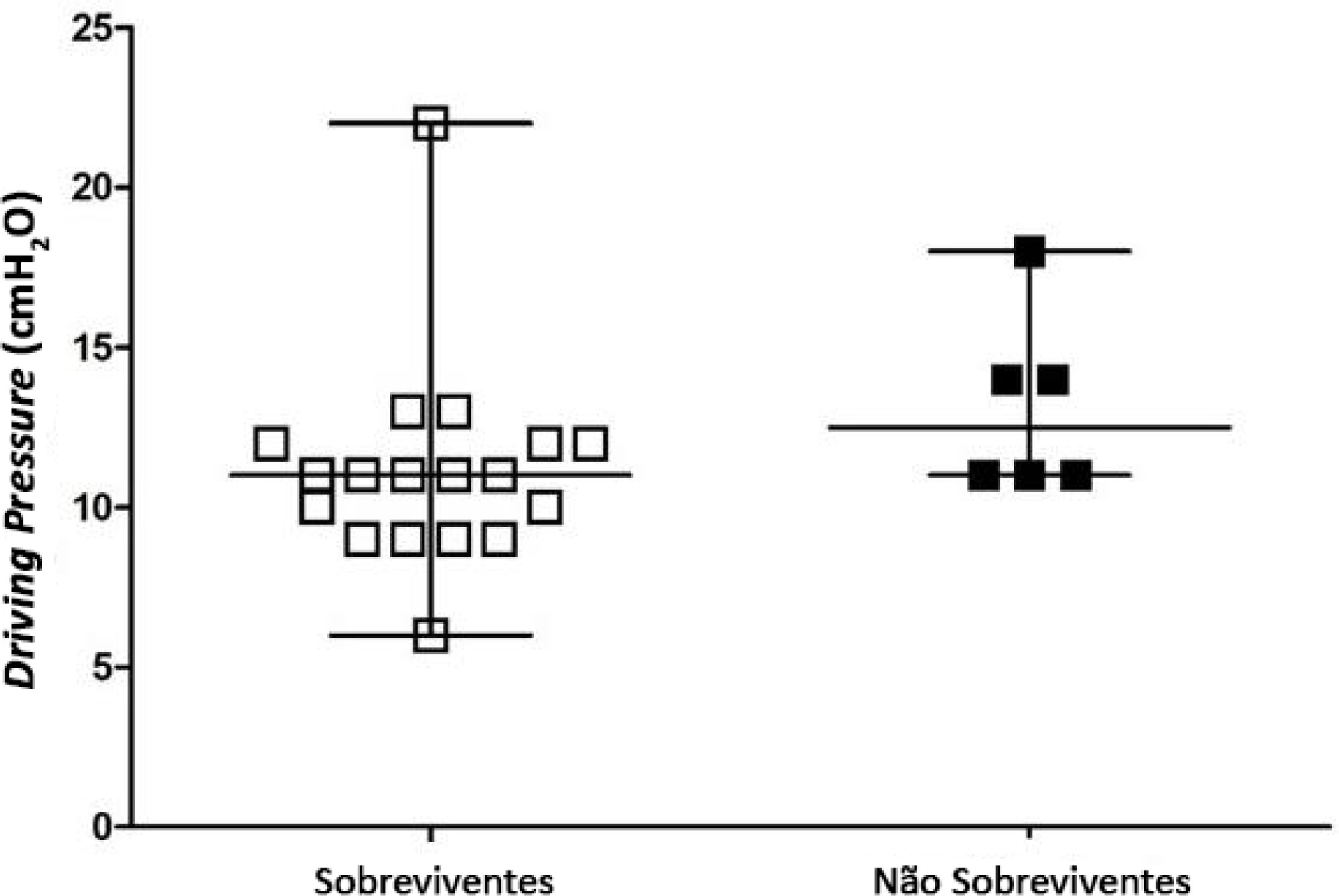
To identify the possible association between driving pressure and mechanical power values and oxygenation index on the first day of mechanical ventilation with the mortality of trauma patients without a diagnosis of acute respiratory distress syndrome.
Patients under pressure-controlled or volume-controlled ventilation were included, with data collection 24 hours after orotracheal intubation. Patient follow-up was performed for 30 days to obtain the clinical outcome. The patients were admitted to two intensive care units of the Hospital de Pronto Socorro de Porto Alegre from June to September 2019.
A total of 24 patients were evaluated. Driving pressure, mechanical power and oxygenation index were similar among patients who survived and those who died, with no statistically significant difference between groups.
Driving pressure, mechanical power and oxygenation index values obtained on the first day of mechanical ventilation were not associated with mortality of trauma patients without acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):312-319
DOI 10.5935/0103-507X.20210040
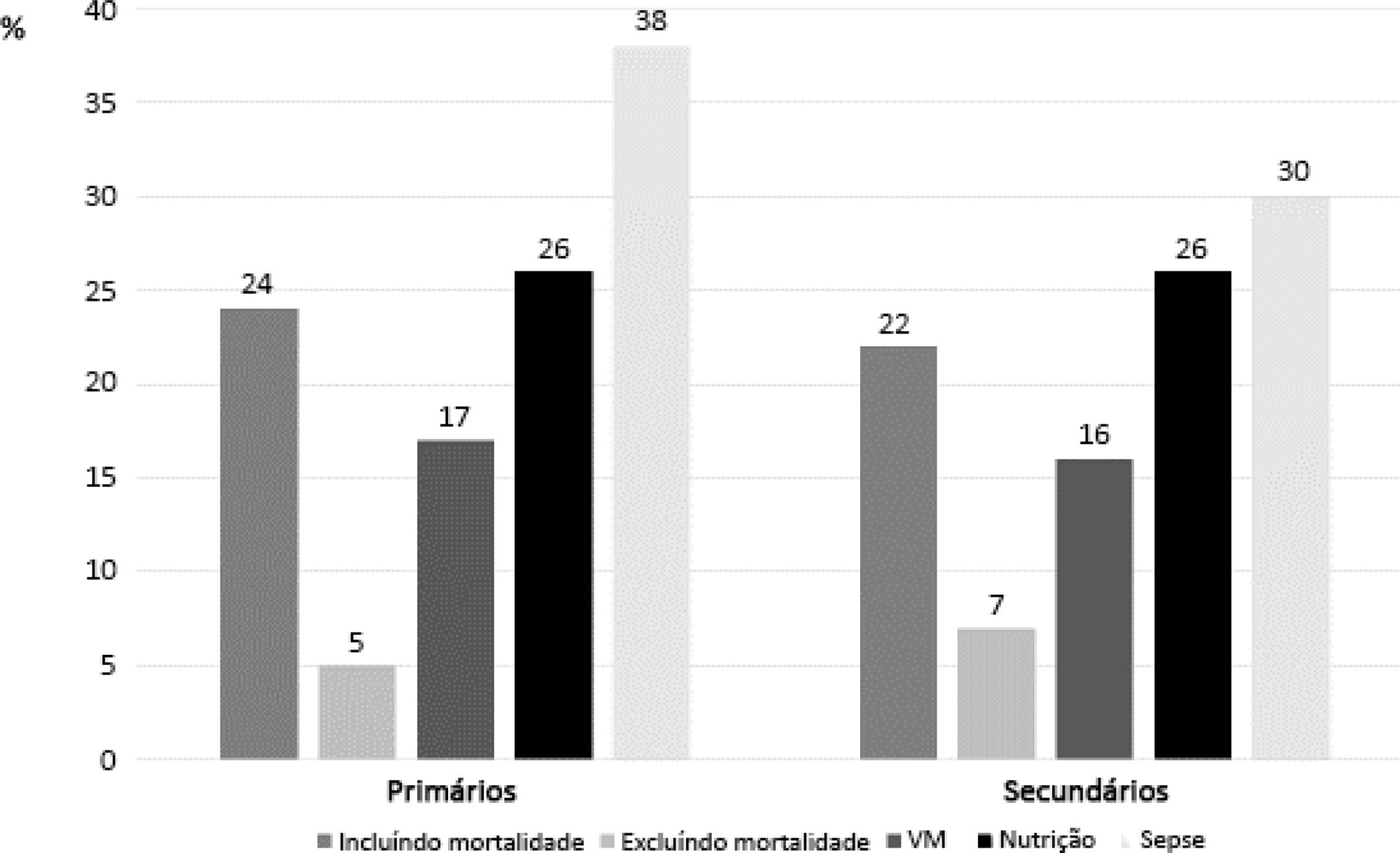
Randomized clinical trials in intensive care prioritize disease-focused outcomes rather than patient-centered outcomes. A paradigm shift considering the evaluation of measures after hospital discharge and measures focused on quality of life and common symptoms, such as pain and dyspnea, could better reflect the wishes of patients and their families. However, barriers related to the systematization of the interpretation of these outcomes, the heterogeneity of measurement instruments and the greater difficulty in performing the studies, to date, seem to hinder this change. In addition, the joint participation of patients, families, researchers, and clinicians in the definition of study outcomes is not yet a reality.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):38-47
DOI 10.5935/0103-507X.20210004
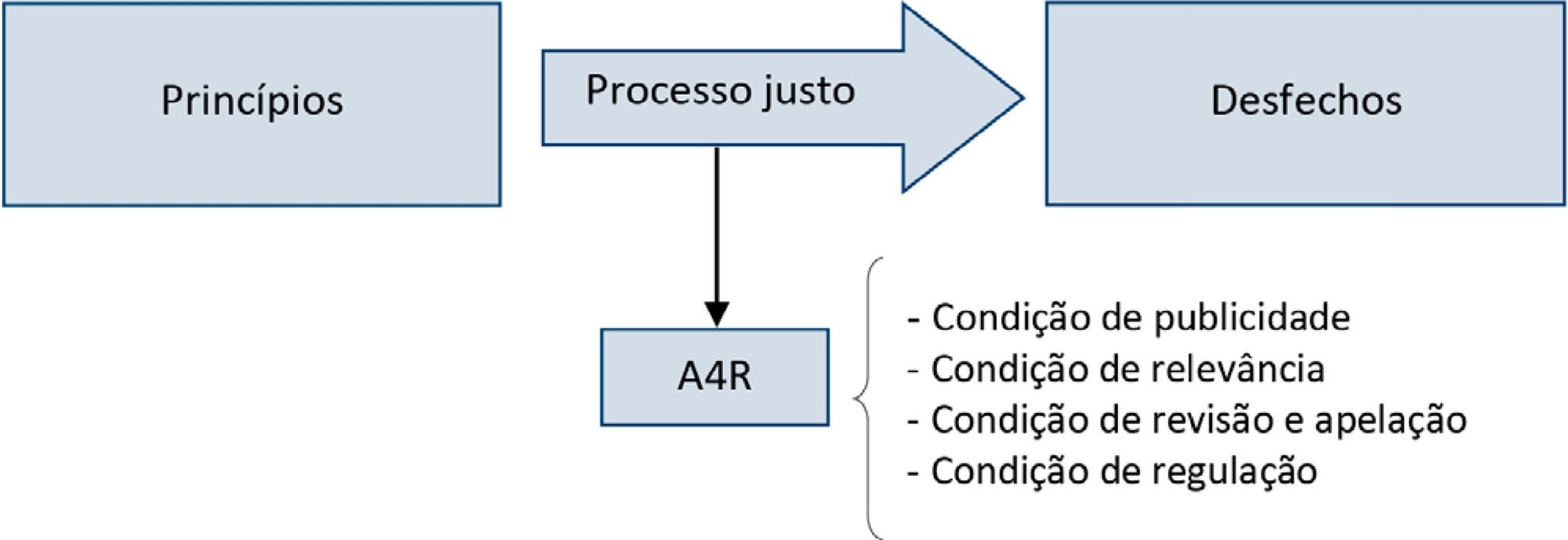
Triage for intensive care unit admission is a frequent event and is associated to worse clinical outcomes. The process of triage is variable and may be influenced by biases and prejudices, which could lead to potentially unfair decisions. The Brazilian Federal Council of Medicine (Conselho Federal de Medicina) has recently released a guideline for intensive care unit admission and discharge. The aim of this paper is to evaluate the ethical dilemmas related to the implementation of this guideline, through the accountability for reasonabless approach, known as A4R, as elaborated by Norman Daniels. We conclude that the guideline contemplates A4R conditions, but we observe that there is a need for indication of A4R-concordant criteria to operationalize the guidelines.