To identify more severe COVID-19 presentations.
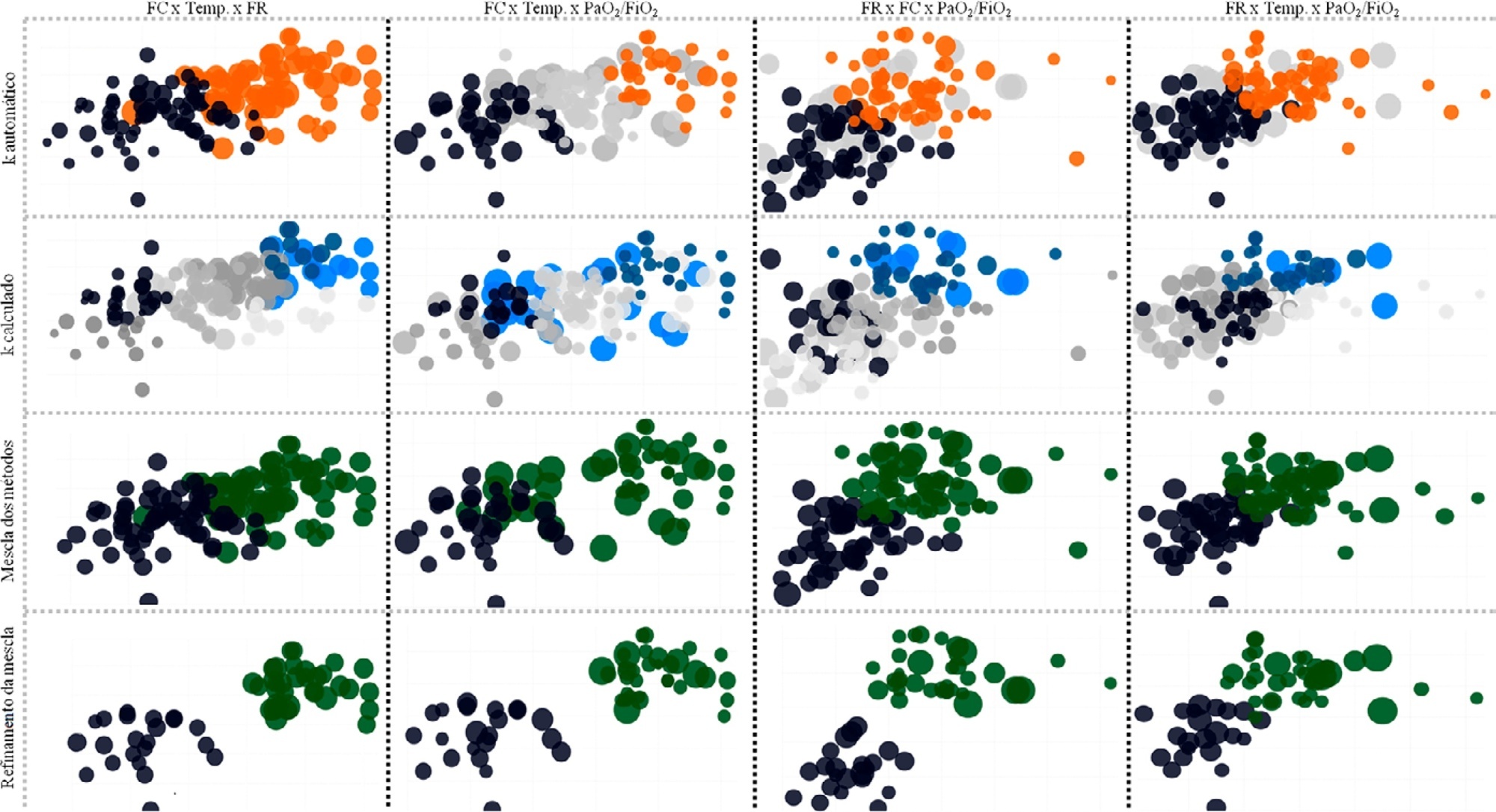
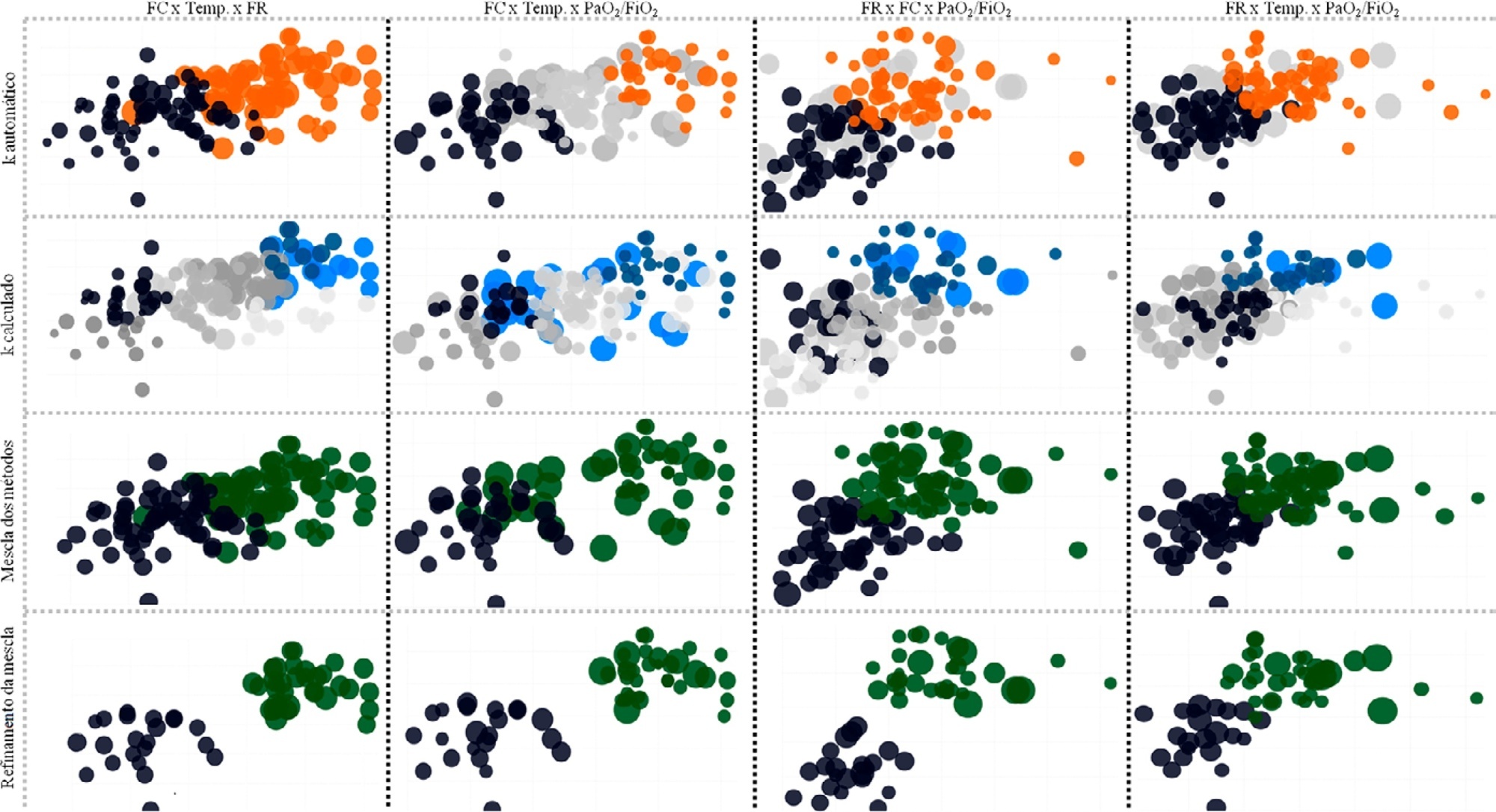
Consecutive intensive care unit-admitted patients were subjected to a stepwise clustering method.
Data from 147 patients who were on average 56 ± 16 years old with a Simplified Acute Physiological Score 3 of 72 ± 18, of which 103 (70%) needed mechanical ventilation and 46 (31%) died in the intensive care unit, were analyzed. From the clustering algorithm, two well-defined groups were found based on maximal heart rate [Cluster A: 104 (95%CI 99 – 109) beats per minute versus Cluster B: 159 (95%CI 155 – 163) beats per minute], maximal respiratory rate [Cluster A: 33 (95%CI 31 – 35) breaths per minute versus Cluster B: 50 (95%CI 47 – 53) breaths per minute], and maximal body temperature [Cluster A: 37.4 (95%CI 37.1 – 37.7)°C versus Cluster B: 39.3 (95%CI 39.1 – 39.5)°C] during the intensive care unit stay, as well as the oxygen partial pressure in the blood over the oxygen inspiratory fraction at intensive care unit admission [Cluster A: 116 (95%CI 99 – 133) mmHg versus Cluster B: 78 (95%CI 63 – 93) mmHg]. Subphenotypes were distinct in inflammation profiles, organ dysfunction, organ support, intensive care unit length of stay, and intensive care unit mortality (with a ratio of 4.2 between the groups).
Our findings, based on common clinical data, revealed two distinct subphenotypes with different disease courses. These results could help health professionals allocate resources and select patients for testing novel therapies.
Search
Search in:

Comments