You searched for:"Rogério Zigaib"
We found (6) results for your search.-
Original Article
Exploring the association of two oxygenators in parallel or in series during respiratory support using extracorporeal membrane oxygenation
Rev Bras Ter Intensiva. 2022;34(4):402-409
Abstract
Original ArticleExploring the association of two oxygenators in parallel or in series during respiratory support using extracorporeal membrane oxygenation
Rev Bras Ter Intensiva. 2022;34(4):402-409
DOI 10.5935/0103-507X.20220299-en
Views3ABSTRACT
Objective:
To characterize the pressures, resistances, oxygenation, and decarboxylation efficacy of two oxygenators associated in series or in parallel during venous-venous extracorporeal membrane oxygenation support.
Methods:
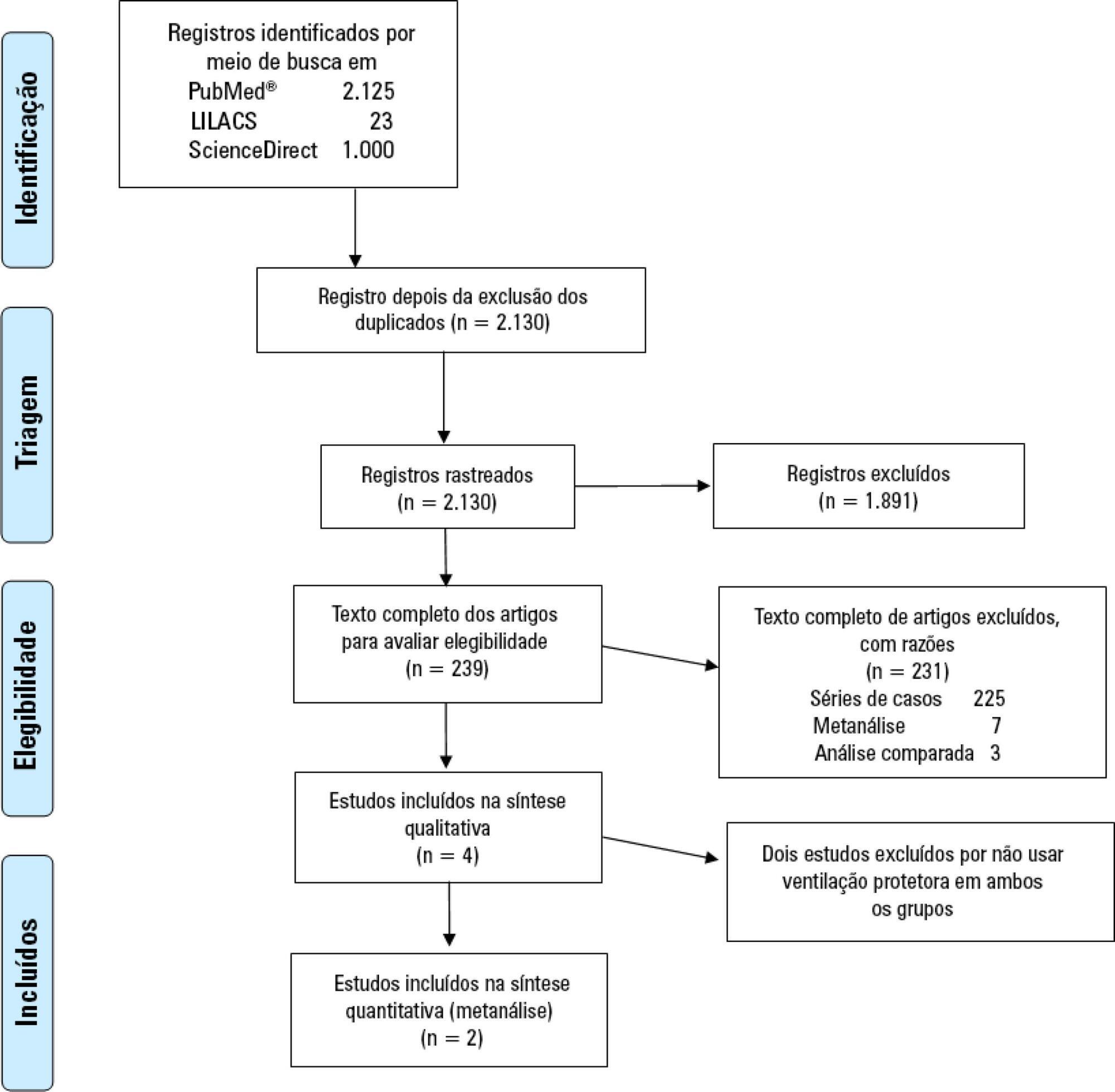
Using the results of a swine severe respiratory failure associated with multiple organ dysfunction venous-venous extracorporeal membrane oxygenation support model and mathematical modeling, we explored the effects on oxygenation, decarboxylation and circuit pressures of in-parallel and in-series associations of oxygenators.
Results:
Five animals with a median weight of 80kg were tested. Both configurations increased the oxygen partial pressure after the oxygenators. The return cannula oxygen content was also slightly higher, but the impact on systemic oxygenation was minimal using oxygenators with a high rated flow (~ 7L/minute). Both configurations significantly reduced the systemic carbon dioxide partial pressure. As the extracorporeal membrane oxygenation blood flow increased, the oxygenator resistance decreased initially with a further increase with higher blood flows but with a small clinical impact.
Conclusion:
Association of oxygenators in parallel or in series during venous-venous extracorporeal membrane oxygenation support provides a modest increase in carbon dioxide partial pressure removal with a slight improvement in oxygenation. The effect of oxygenator associations on extracorporeal circuit pressures is minimal.
Keywords:acute respiratory distress syndromeDecarboxylationExtracorporeal membrane oxygenationHypercapniaHypoxiaOxygenatorsSwineSee more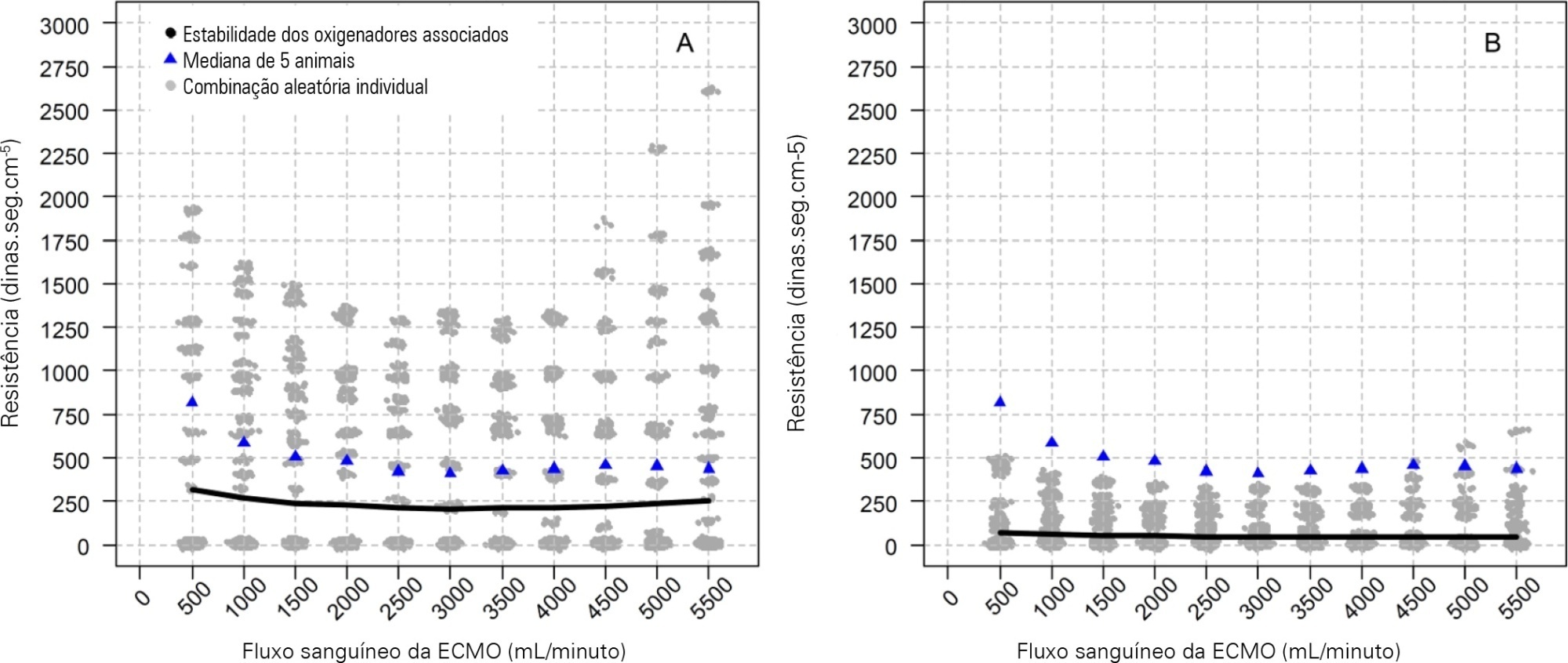
-
Original Article
Bedside clinical data subphenotypes of critically ill COVID-19 patients: a cohort study
Rev Bras Ter Intensiva. 2021;33(2):196-205
Abstract
Original ArticleBedside clinical data subphenotypes of critically ill COVID-19 patients: a cohort study
Rev Bras Ter Intensiva. 2021;33(2):196-205
DOI 10.5935/0103-507X.20210027
Views0See moreAbstract
Objective:
To identify more severe COVID-19 presentations.
Methods:
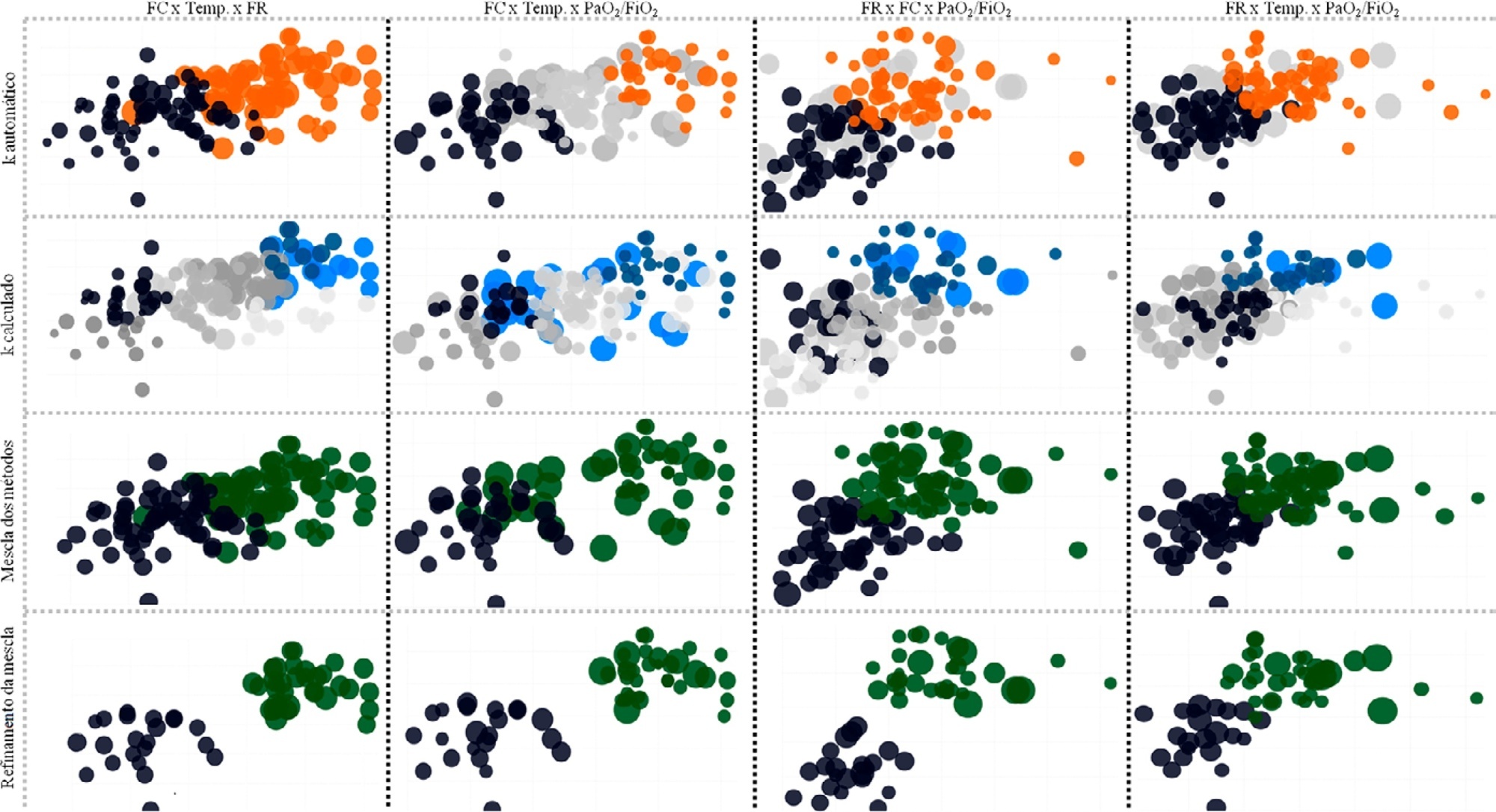
Consecutive intensive care unit-admitted patients were subjected to a stepwise clustering method.
Results:
Data from 147 patients who were on average 56 ± 16 years old with a Simplified Acute Physiological Score 3 of 72 ± 18, of which 103 (70%) needed mechanical ventilation and 46 (31%) died in the intensive care unit, were analyzed. From the clustering algorithm, two well-defined groups were found based on maximal heart rate [Cluster A: 104 (95%CI 99 – 109) beats per minute versus Cluster B: 159 (95%CI 155 – 163) beats per minute], maximal respiratory rate [Cluster A: 33 (95%CI 31 – 35) breaths per minute versus Cluster B: 50 (95%CI 47 – 53) breaths per minute], and maximal body temperature [Cluster A: 37.4 (95%CI 37.1 – 37.7)°C versus Cluster B: 39.3 (95%CI 39.1 – 39.5)°C] during the intensive care unit stay, as well as the oxygen partial pressure in the blood over the oxygen inspiratory fraction at intensive care unit admission [Cluster A: 116 (95%CI 99 – 133) mmHg versus Cluster B: 78 (95%CI 63 – 93) mmHg]. Subphenotypes were distinct in inflammation profiles, organ dysfunction, organ support, intensive care unit length of stay, and intensive care unit mortality (with a ratio of 4.2 between the groups).
Conclusion:
Our findings, based on common clinical data, revealed two distinct subphenotypes with different disease courses. These results could help health professionals allocate resources and select patients for testing novel therapies.
-
Original Article
Oxygen delivery, carbon dioxide removal, energy transfer to lungs and pulmonary hypertension behavior during venous-venous extracorporeal membrane oxygenation support: a mathematical modeling approach
Rev Bras Ter Intensiva. 2019;31(2):113-121
Abstract
Original ArticleOxygen delivery, carbon dioxide removal, energy transfer to lungs and pulmonary hypertension behavior during venous-venous extracorporeal membrane oxygenation support: a mathematical modeling approach
Rev Bras Ter Intensiva. 2019;31(2):113-121
DOI 10.5935/0103-507X.20190018
Views0ABSTRACT
Objective:
To describe (1) the energy transfer from the ventilator to the lungs, (2) the match between venous-venous extracorporeal membrane oxygenation (ECMO) oxygen transfer and patient oxygen consumption (VO2), (3) carbon dioxide removal with ECMO, and (4) the potential effect of systemic venous oxygenation on pulmonary artery pressure.
Methods:
Mathematical modeling approach with hypothetical scenarios using computer simulation.
Results:
The transition from protective ventilation to ultraprotective ventilation in a patient with severe acute respiratory distress syndrome and a static respiratory compliance of 20mL/cm H2O reduced the energy transfer from the ventilator to the lungs from 35.3 to 2.6 joules/minute. A hypothetical patient, hyperdynamic and slightly anemic with VO2 = 200mL/minute, can reach an arterial oxygen saturation of 80%, while maintaining the match between the oxygen transfer by ECMO and the VO2 of the patient. Carbon dioxide is easily removed, and normal PaCO2 is easily reached. Venous blood oxygenation through the ECMO circuit may drive the PO2 stimulus of pulmonary hypoxic vasoconstriction to normal values.
Conclusion:
Ultraprotective ventilation largely reduces the energy transfer from the ventilator to the lungs. Severe hypoxemia on venous-venous-ECMO support may occur despite the matching between the oxygen transfer by ECMO and the VO2 of the patient. The normal range of PaCO2 is easy to reach. Venous-venous-ECMO support potentially relieves hypoxic pulmonary vasoconstriction.
Keywords:acute respiratory distress syndromeExtracorporeal membrane oxygenationIntensive Care UnitMathematical modelmechanical ventilationrespiratory failureSee more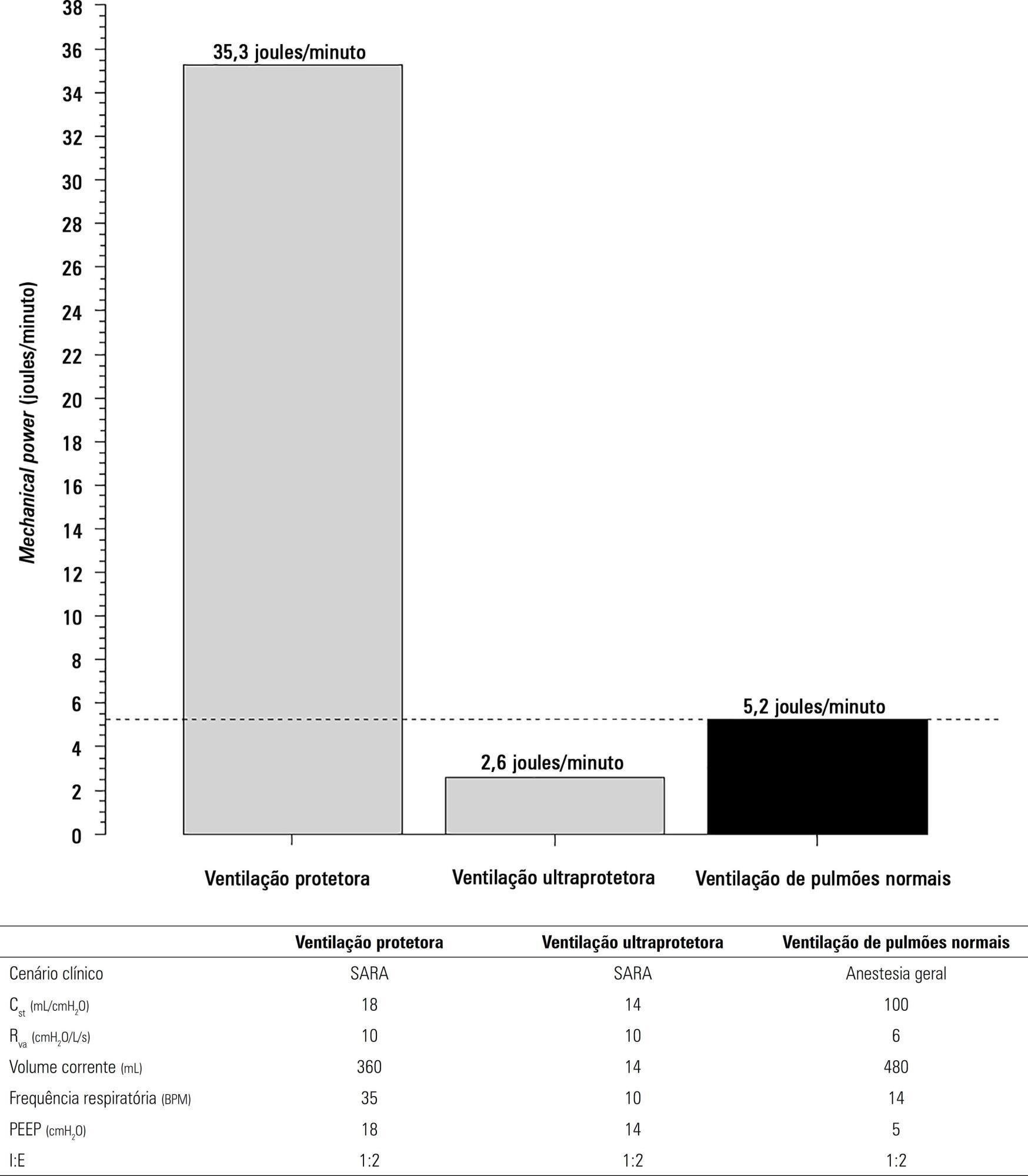
-
Original Articles
Evaluation of cost-effectiveness from the funding body’s point of view of ultrasound-guided central venous catheter insertion compared with the conventional technique
Rev Bras Ter Intensiva. 2016;28(1):62-69
Abstract
Original ArticlesEvaluation of cost-effectiveness from the funding body’s point of view of ultrasound-guided central venous catheter insertion compared with the conventional technique
Rev Bras Ter Intensiva. 2016;28(1):62-69
DOI 10.5935/0103-507X.20160014
Views0ABSTRACT
Objective:
To evaluate the cost-effectiveness, from the funding body’s point of view, of real-time ultrasound-guided central venous catheter insertion compared to the traditional method, which is based on the external anatomical landmark technique.
Methods:
A theoretical simulation based on international literature data was applied to the Brazilian context, i.e., the Unified Health System (Sistema Único de Saúde – SUS). A decision tree was constructed that showed the two central venous catheter insertion techniques: real-time ultrasonography versus external anatomical landmarks. The probabilities of failure and complications were extracted from a search on the PubMed and Embase databases, and values associated with the procedure and with complications were taken from market research and the Department of Information Technology of the Unified Health System (DATASUS). Each central venous catheter insertion alternative had a cost that could be calculated by following each of the possible paths on the decision tree. The incremental cost-effectiveness ratio was calculated by dividing the mean incremental cost of real-time ultrasound compared to the external anatomical landmark technique by the mean incremental benefit, in terms of avoided complications.
Results:
When considering the incorporation of real-time ultrasound and the concomitant lower cost due to the reduced number of complications, the decision tree revealed a final mean cost for the external anatomical landmark technique of 262.27 Brazilian reals (R$) and for real-time ultrasound of R$187.94. The final incremental cost of the real-time ultrasound-guided technique was -R$74.33 per central venous catheter. The incremental cost-effectiveness ratio was -R$2,494.34 due to the pneumothorax avoided.
Conclusion:
Real-time ultrasound-guided central venous catheter insertion was associated with decreased failure and complication rates and hypothetically reduced costs from the view of the funding body, which in this case was the SUS.
Keywords:Central venous cateteres/ economicsCosts and cost analysisDiagnostic techniques and proceduresHelath care costsUltrasonography/economicsUnified Health System/economicsSee more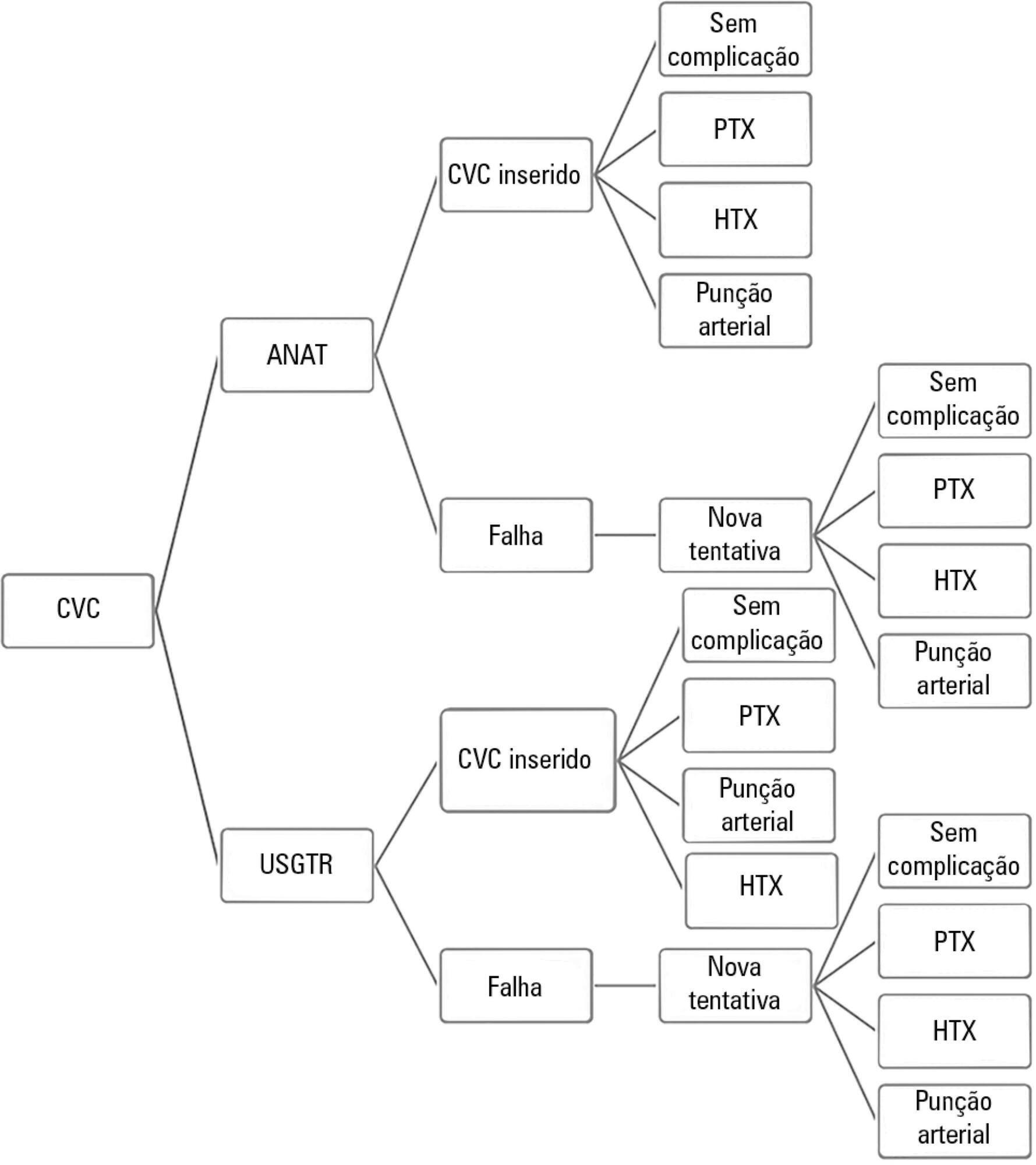
-
Editorial
Critical care medicine: extracorporeal oxygenation is feasible in Brazil?
Rev Bras Ter Intensiva. 2014;26(3):200-202
Abstract
EditorialCritical care medicine: extracorporeal oxygenation is feasible in Brazil?
Rev Bras Ter Intensiva. 2014;26(3):200-202
DOI 10.5935/0103-507X.20140029
Views0Ventilatory support has been a major reason for hospitalization in intensive care units (ICU) since the creation of these units, which came about precisely for that immediate need during the polio epidemic in Europe.( , ) In 1967, Ashbaugh described a series of severe cases marked by respiratory failure, cyanosis, hypoxemia refractory to oxygen therapy […]See more
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis