Abstract
Rev Bras Ter Intensiva. 2021;33(1):125-137
DOI 10.5935/0103-507X.20210014
To study the impact of delayed admission by more than 4 hours on the outcomes of critically ill patients.
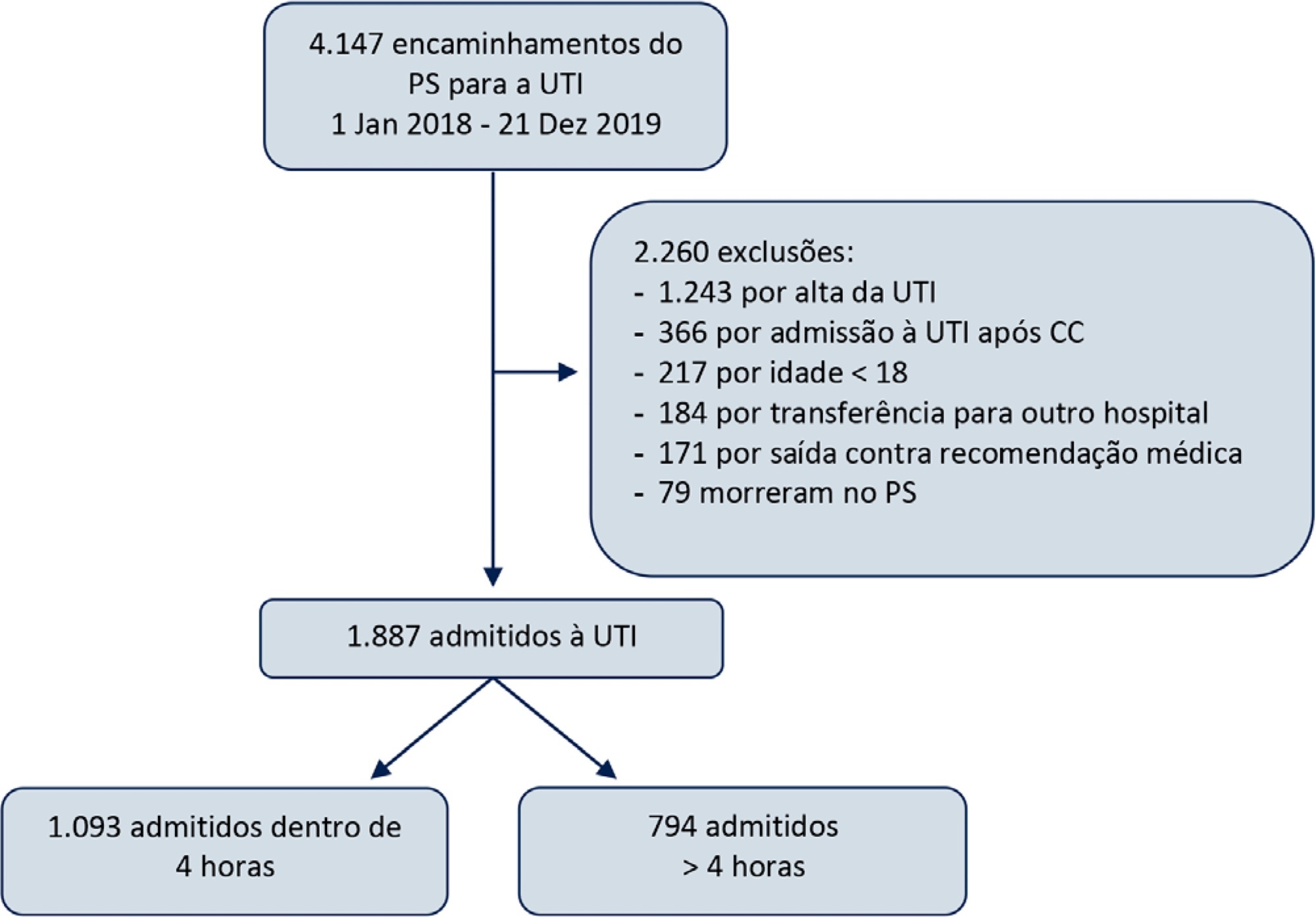
This was a retrospective observational study in which adult patients admitted directly from the emergency department to the intensive care unit were divided into two groups: Timely Admission if they were admitted within 4 hours and Delayed Admission if admission was delayed for more than 4 hours. Intensive care unit length of stay and hospital/intensive care unit mortality were compared between the groups. Propensity score matching was performed to correct for imbalances. Logistic regression analysis was used to explore delayed admission as an independent risk factor for intensive care unit mortality.
During the study period, 1,887 patients were admitted directly from the emergency department to the intensive care unit, with 42% being delayed admissions. Delayed patients had significantly longer intensive care unit lengths of stay and higher intensive care unit and hospital mortality. These results were persistent after propensity score matching of the groups. Delayed admission was an independent risk factor for intensive care unit mortality (OR = 2.6; 95%CI 1.9 - 3.5; p < 0.001). The association of delay and intensive care unit mortality emerged after a delay of 2 hours and was highest after a delay of 4 hours.
Delayed admission to the intensive care unit from the emergency department is an independent risk factor for intensive care unit mortality, with the strongest association being after a delay of 4 hours.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):138-145
DOI 10.5935/0103-507X.20210015
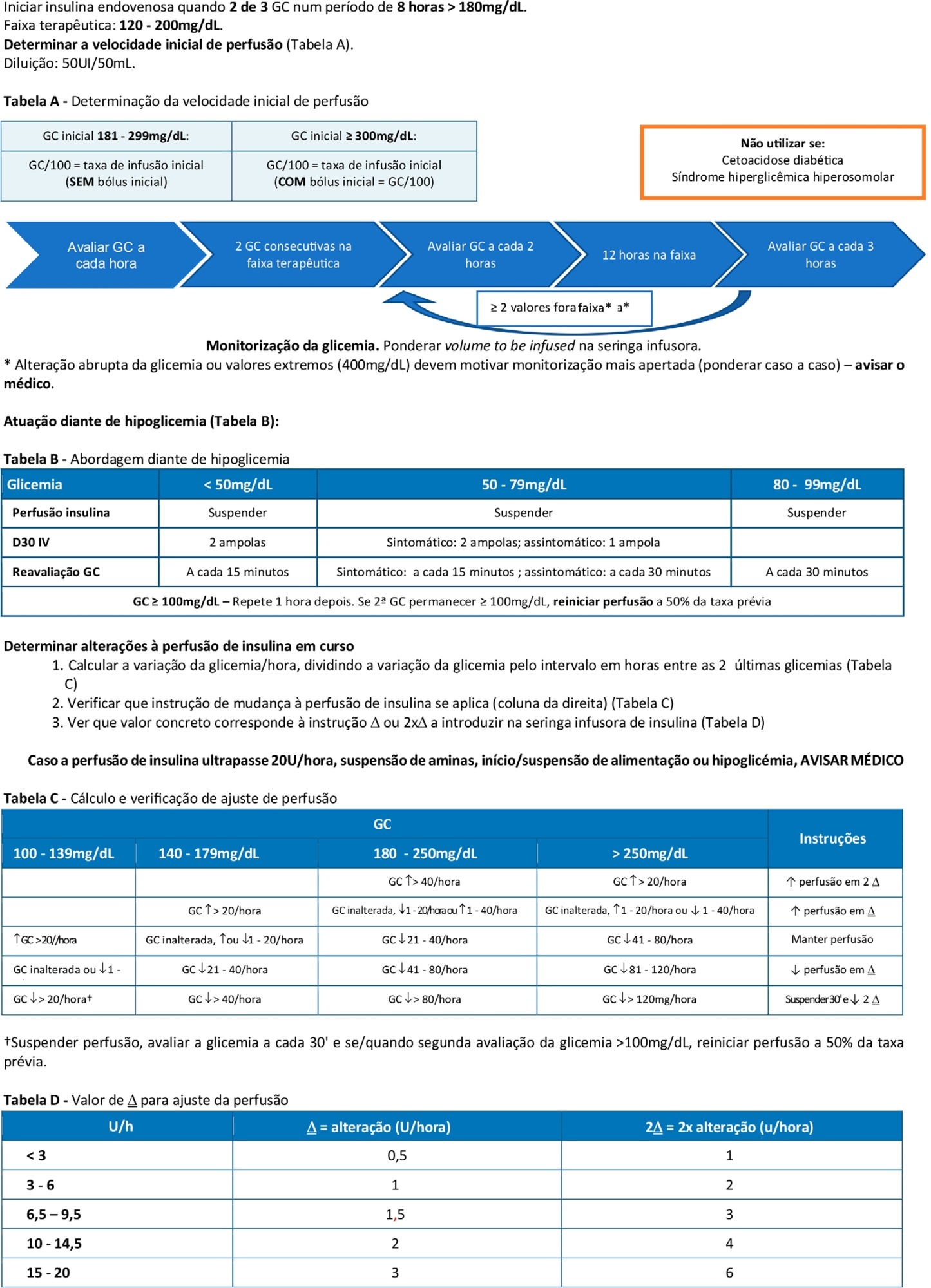
To double the percentage of time within the 100 - 180mg/dL blood glucose range in the first three months following a phased implementation of a formal education program, and then, of an insulin therapy protocol, without entailing an increased incidence of hypoglycemia.
The pre-intervention glycemic control was assessed retrospectively. Next, were carried out the implementation of a formal education program, distribution of manual algorithms for intravenous insulin therapy - optimized by the users, based on the modified Yale protocol - and informal training of the nursing staff. The use of electronic blood glucose control systems was supported, and the results were recorded prospectively.
The first phase of the program (formal education) lead to improvement of the time within the euglycemic interval (28% to 37%). In the second phase, euglycemia was achieved 66% of the time, and the incidence of hypoglycemia was decreased. The percentage of patients on intravenous insulin infusion at 48 hours from admission increased from 6% to 35%.
The phased implementation of a formal education program, fostering the use of electronic insulin therapy protocols and dynamic manuals, received good adherence and has shown to be safe and effective for blood glucose control in critically ill patients, with a concomitant decrease in hypoglycemia.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):146-153
DOI 10.5935/0103-507X.20210016
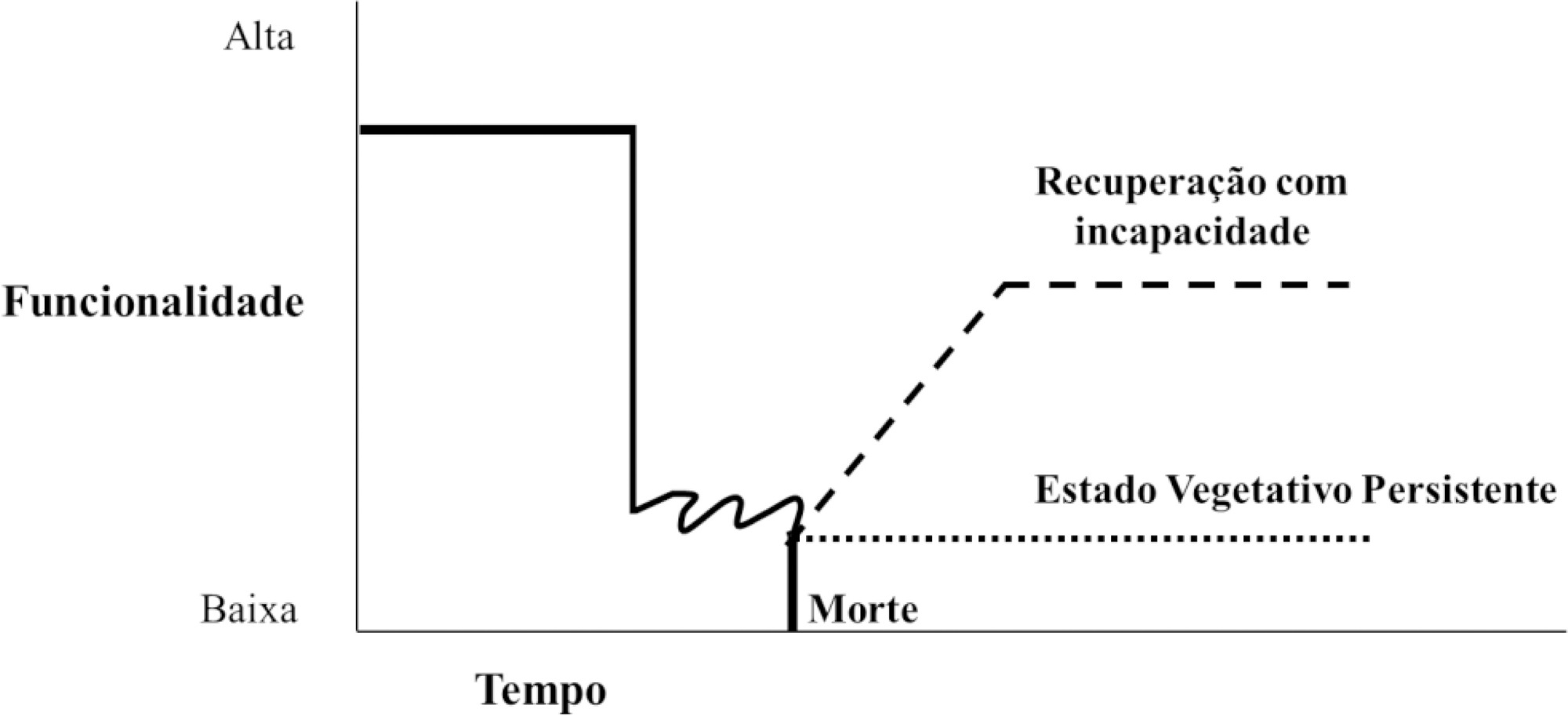
Neurological diseases are estimated to affect 1 billion people worldwide and are the cause of one in 10 deaths. In Brazil, they are responsible for approximately 14% of clinical admissions to intensive care units, 9% of elective neurosurgeries and 14% of emergency neurosurgeries. Many of these conditions are incurable, result in reduced life expectancy and quality of life and increased dependence, and are associated with symptoms that are likely to cause suffering, which justifies the integration of palliative care into usual care. In addition, factors unique to acute neurological injuries, such as their catastrophic clinical presentation, complex and uncertain prognosis, associated communication difficulties and issues related to quality of life, require a specific approach, which has recently been termed "neuropalliative care". Although the topic is relevant and current, it is still little discussed, and much of what is known about palliative care in this context is extrapolated from approaches used under other conditions. Therefore, the objective of this study was to conduct a narrative literature review to identify the challenges of applying the palliative care approach in the care of neurocritically ill patients, with a focus on three groups: neurocritically ill patients, families and intensive care teams. This review identified that in intensive care, the main demands for palliative care are for prognostic definitions and care planning. Training in primary palliative care and improving communication were also needs identified by intensivists and families, respectively. In contrast with what has been found under other conditions, the management of symptoms was not indicated as a complex issue, although it is still relevant.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):111-118
DOI 10.5935/0103-507X.20210012
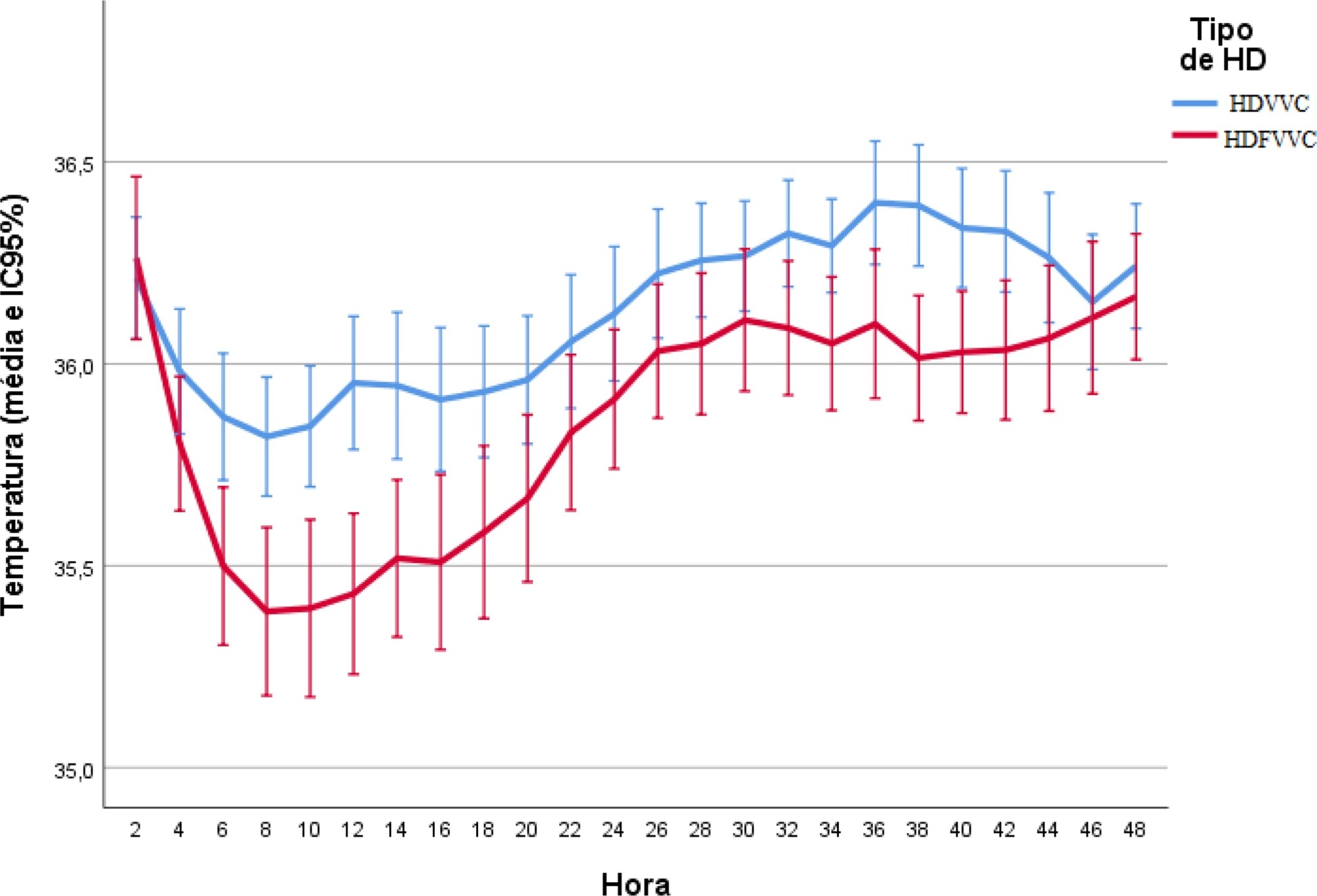
To evaluate the incidence of hypothermia in patients undergoing continuous renal replacement therapy in the intensive care unit. As secondary objectives, we determined associated factors and compared the occurrence of hypothermia between two modalities of continuous renal replacement therapy.
A prospective cohort study was conducted with adult patients who were admitted to a clinical-surgical intensive care unit and underwent continuous renal replacement therapy in a high-complexity public university hospital in southern Brazil from April 2017 to July 2018. Hypothermia was defined as a body temperature ≤ 35ºC. The patients included in the study were followed for the first 48 hours of continuous renal replacement therapy. The researchers collected data from medical records and continuous renal replacement therapy records.
A total of 186 patients were equally distributed between two types of continuous renal replacement therapy: hemodialysis and hemodiafiltration. The incidence of hypothermia was 52.7% and was higher in patients admitted for shock (relative risk of 2.11; 95%CI 1.21 - 3.69; p = 0.009) and in those who underwent hemodiafiltration with heating in the return line (relative risk of 1.50; 95%CI 1.13 - 1.99; p = 0.005).
Hypothermia in critically ill patients with continuous renal replacement therapy is frequent, and the intensive care team should be attentive, especially when there are associated risk factors.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):528-534
DOI 10.5935/0103-507X.20200090
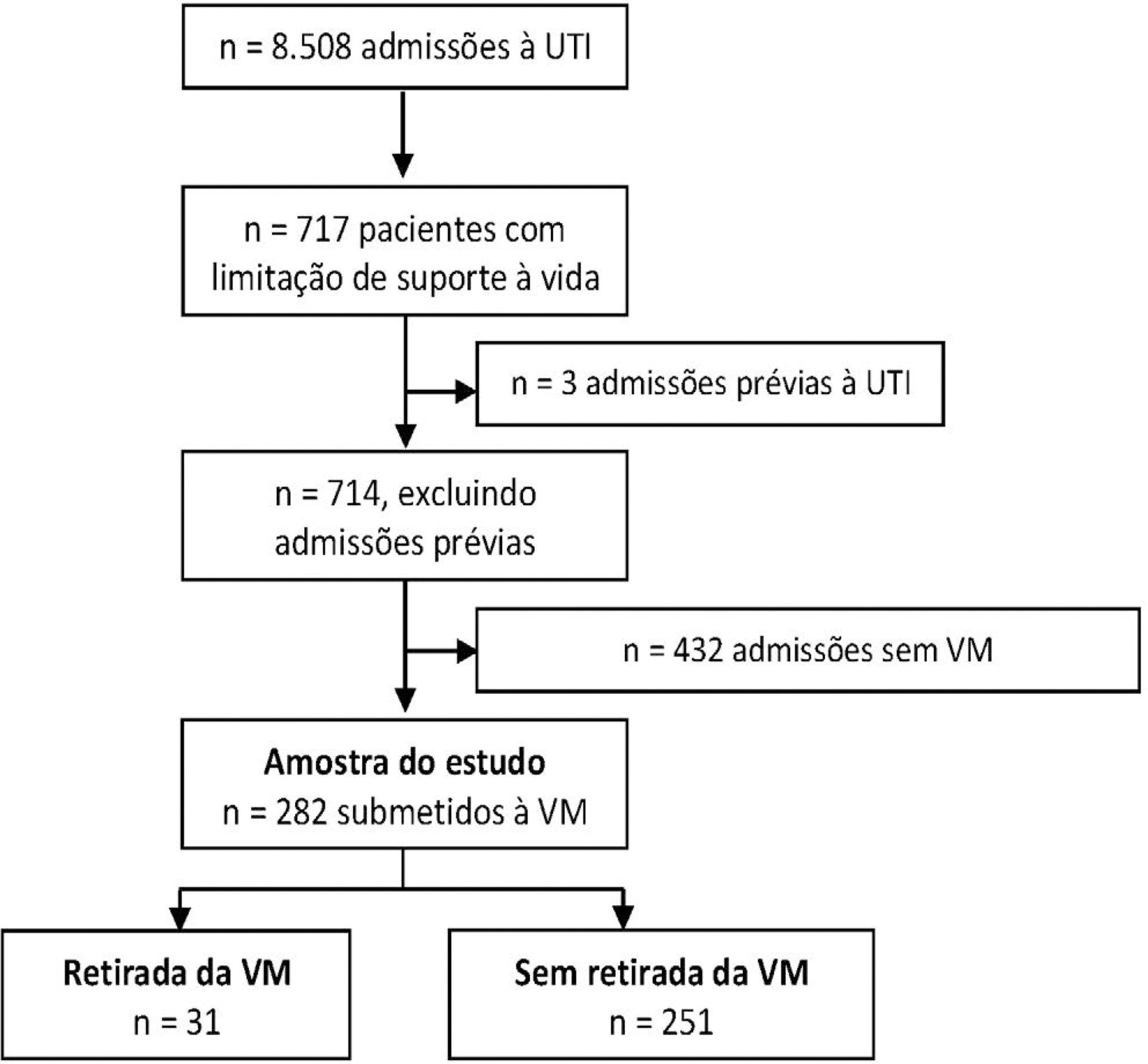
To describe the characteristics and outcomes of patients undergoing mechanical ventilation withdrawal and to compare them to mechanically ventilated patients with limitations (withhold or withdrawal) of life-sustaining therapies but who did not undergo mechanical ventilation withdrawal.
This was a retrospective cohort study from January 2014 to December 2018 of mechanically ventilated patients with any organ support limitation admitted to a single intensive care unit. We compared patients who underwent mechanical ventilation withdrawal and those who did not regarding intensive care unit and hospital mortality and length of stay in both an unadjusted analysis and a propensity score matched subsample. We also analyzed the time from mechanical ventilation withdrawal to death.
Out of 282 patients with life-sustaining therapy limitations, 31 (11%) underwent mechanical ventilation withdrawal. There was no baseline difference between groups. Intensive care unit and hospital mortality rates were 71% versus 57% and 93% versus 80%, respectively, among patients who underwent mechanical ventilation withdrawal and those who did not. The median intensive care unit length of stay was 7 versus 8 days (p = 0.6), and the hospital length of stay was 9 versus 15 days (p = 0.015). Hospital mortality was not significantly different (25/31; 81% versus 29/31; 93%; p = 0.26) after matching. The median time from mechanical ventilation withdrawal until death was 2 days [0 - 5], and 10/31 (32%) patients died within 24 hours after mechanical ventilation withdrawal.
In this Brazilian report, mechanical ventilation withdrawal represented 11% of all patients with treatment limitations and was not associated with increased hospital mortality after propensity score matching on relevant covariates.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):521-527
DOI 10.5935/0103-507X.20200089
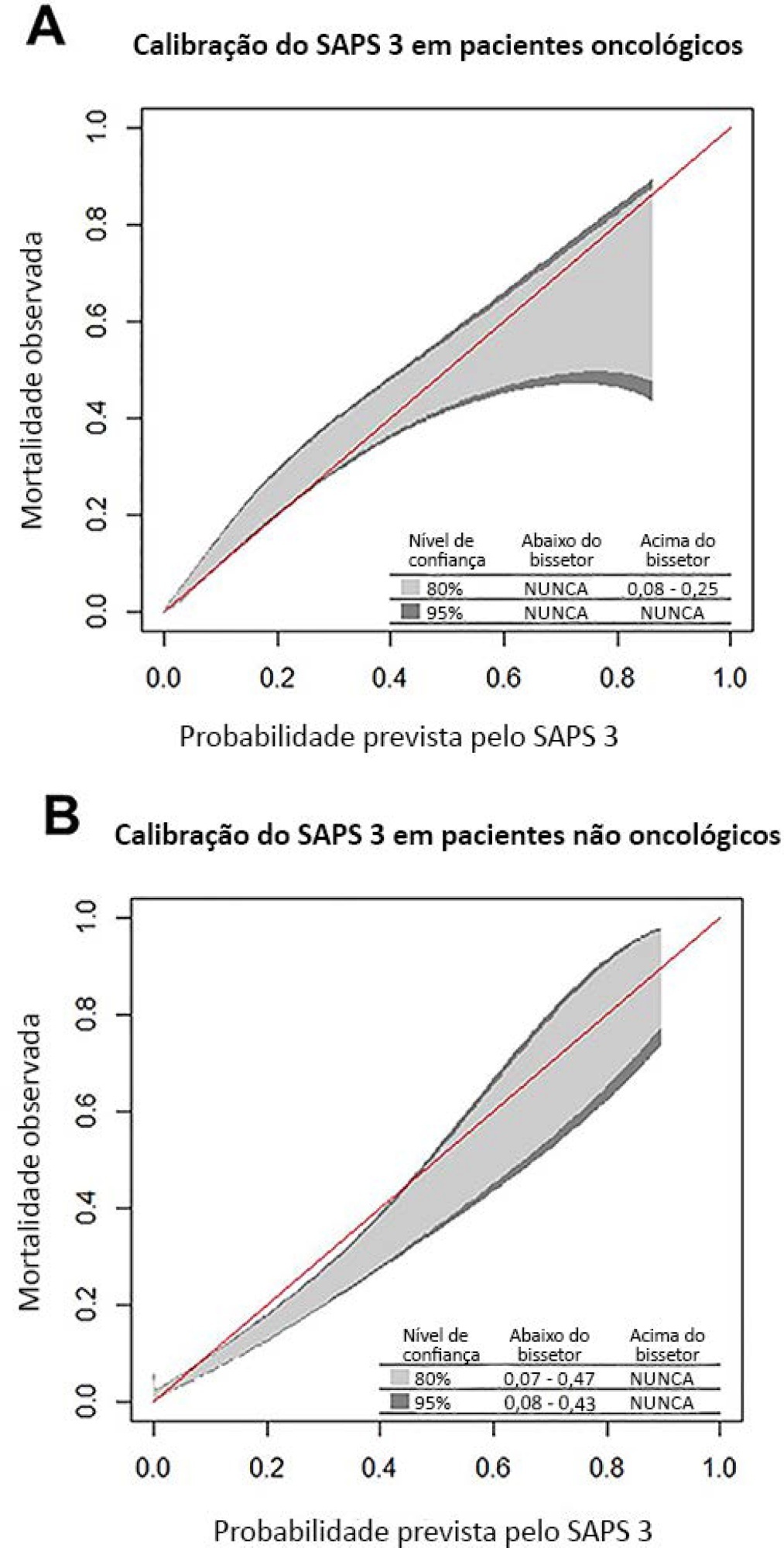
To compare the performance of the Simplified Acute Physiology Score 3 (SAPS 3) in patients with and without solid cancer who were admitted to the intensive care unit of a comprehensive oncological hospital in Brazil.
We performed a retrospective cohort analysis of our administrative database of the first admission of adult patients to the intensive care unit from 2012 to 2016. The patients were categorized according to the presence of solid cancer. We evaluated discrimination using the area under the Receiver Operating Characteristic curve (AUROC) and calibration using the calibration belt approach.
We included 7,254 patients (41.5% had cancer, and 12.1% died during hospitalization). Oncological patients had higher hospital mortality than nononcological patients (14.1% versus 10.6%, respectively; p < 0.001). SAPS 3 discrimination was better for oncological patients (AUROC = 0.85) than for nononcological patients (AUROC = 0.79) (p < 0.001). After we applied the calibration belt in oncological patients, the SAPS 3 matched the average observed rates with a confidence level of 95%. In nononcological patients, the SAPS 3 overestimated mortality in those with a low-middle risk. Calibration was affected by the time period only for nononcological patients.
SAPS 3 performed differently between oncological and nononcological patients in our single-center cohort, and variation over time (mainly calibration) was observed. This finding should be taken into account when evaluating severity-of-illness score performance.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):564-570
DOI 10.5935/0103-507X.20200094
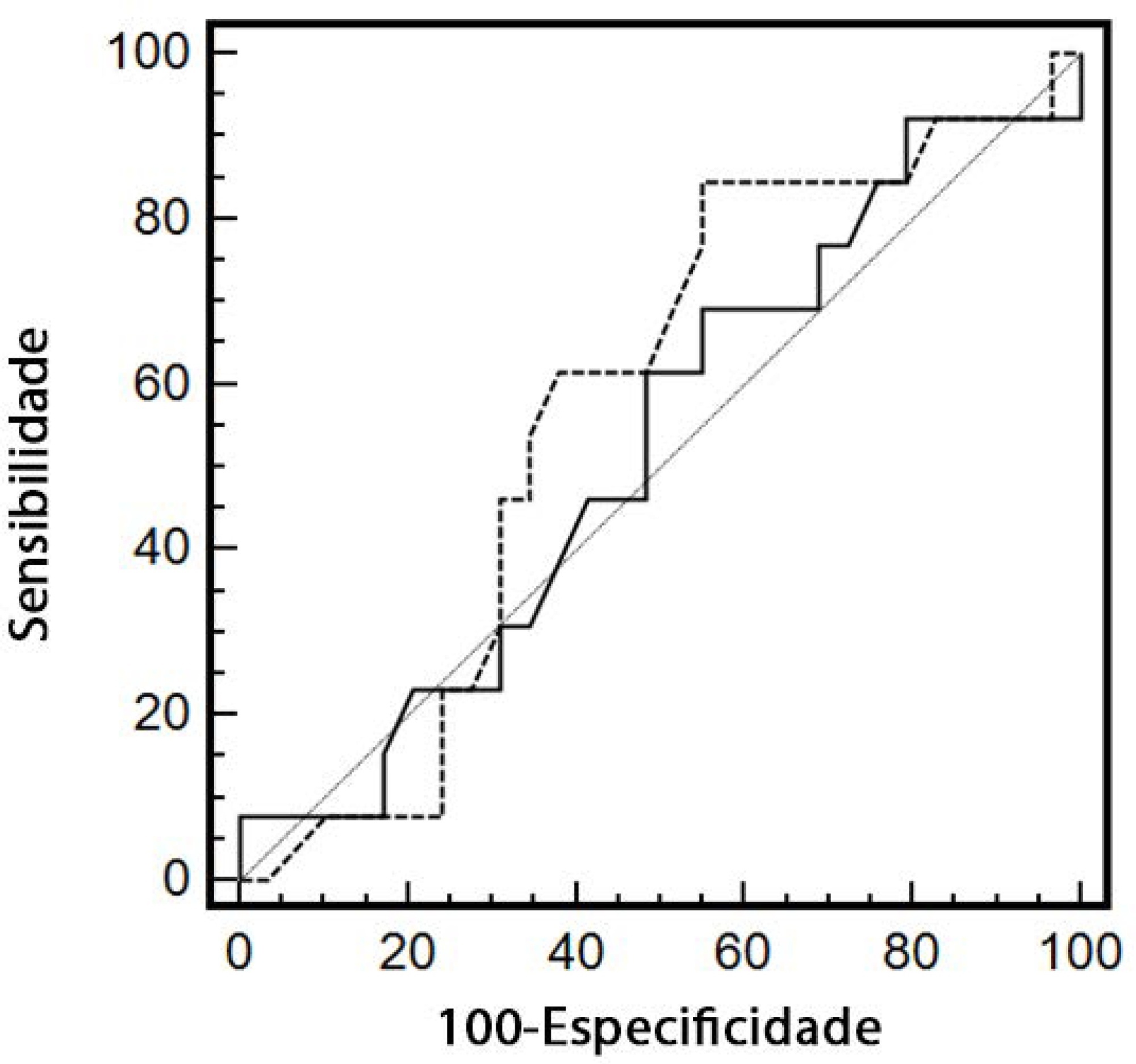
To evaluate renal responsiveness in oliguric critically ill patients after a fluid challenge.
We conducted a prospective observational study in one university intensive care unit. Patients with urine output < 0.5mL/kg/h for 3 hours with a mean arterial pressure > 60mmHg received a fluid challenge. We examined renal fluid responsiveness (defined as urine output > 0.5mL/kg/h for 3 hours) after fluid challenge.
Forty-two patients (age 67 ± 13 years; APACHE II score 16 ± 6) were evaluated. Patient characteristics were similar between renal responders and renal nonresponders. Thirteen patients (31%) were renal responders. Hemodynamic or perfusion parameters were not different between those who did and those who did not increase urine output before the fluid challenge. The areas under the receiver operating characteristic curves were calculated for mean arterial pressure, heart rate, creatinine, urea, creatinine clearance, urea/creatinine ratio and lactate before the fluid challenge. None of these parameters were sensitive or specific enough to predict reversal of oliguria.
After achieving hemodynamic stability, oliguric patients did not increase urine output after a fluid challenge. Systemic hemodynamic, perfusion or renal parameters were weak predictors of urine responsiveness. Our results suggest that volume replacement to correct oliguria in patients without obvious hypovolemia should be done with caution.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):603-605
DOI 10.5935/0103-507X.20200098
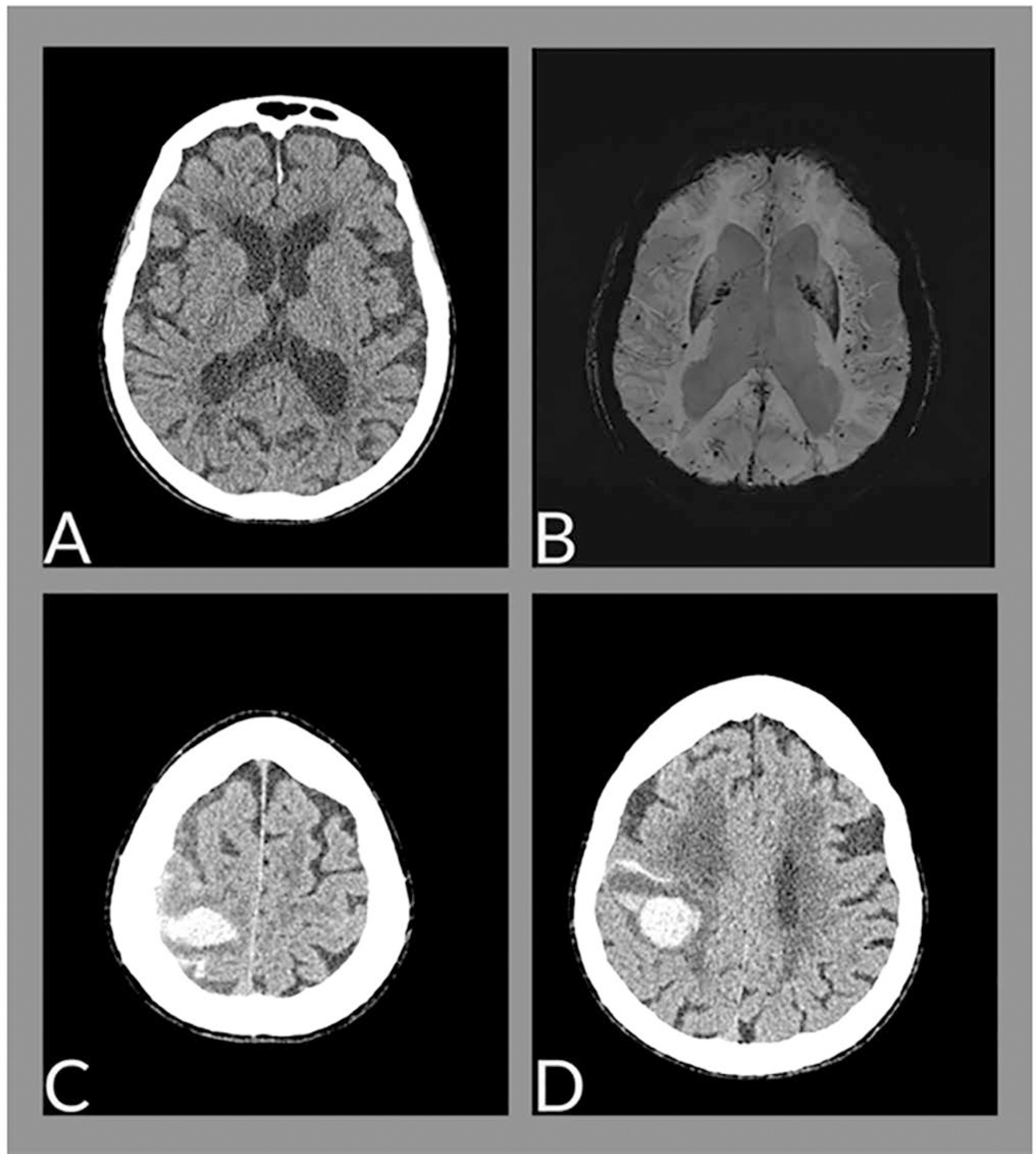
The neurological changes associated with COVID-19 have been frequently described, especially in cases of greater severity, and are related to multifactorial causes, such as endothelial dysfunction, inflammatory mediator release (cytokine storm), endothelial dysfunction and hypoxemia. We report the case of a female patient, 88 years old, with cerebral hemorrhage associated with amyloid angiopathy in the context of SARS-CoV-2 infection.