Abstract
Rev Bras Ter Intensiva. 2020;32(4):535-541
DOI 10.5935/0103-507X.20200083
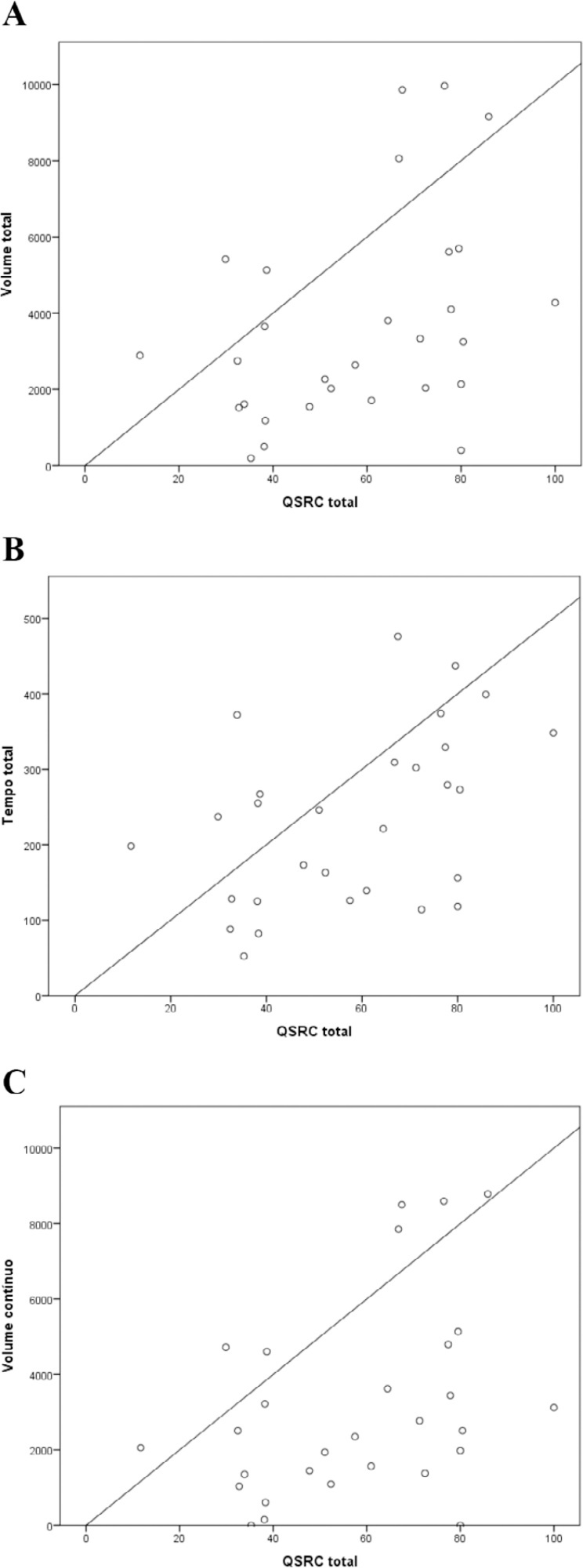
To investigate the viability of the bispectral index in the sleep evaluation of critically ill patients and to quantify the associations of sleep parameters measured by this index with the Richards-Campbell Sleep Questionnaire and environmental noise.
This was a cross-sectional observational study that evaluated critically ill adults with diseases of low or moderate severity. The following were measured: total sleep volume and time, deep sleep volume and time, continuous sleep volume and time, sleep onset latency, and environmental sound pressure level. The subjective perception of sleep was evaluated with the Richards-Campbell Sleep Questionnaire the morning after each night of observation.
Patients had a low total sleep time (234 minutes), a predominance of superficial sleep stages, and little deep sleep (1.7 minutes). The total, deep, and continuous sleep volumes were 3,679, 9.4, and 3,143 (bispectral index units × minutes), respectively. The sleep latency was 94 minutes. The mean score of the Richards-Campbell Sleep Questionnaire was 57.9. Total sleep volume, total sleep time, and continuous sleep volume were weakly correlated with the Richards-Campbell Sleep Questionnaire depth of sleep domain score, overall sleep quality domain score, and total score. Total volume, total time, and continuous volume were moderately correlated with the occurrence of awakenings domain score.
The bispectral index is an instrument with limited viability to monitor the sleep of lucid patients and patients with low to moderate disease severity in the intensive care unit. Patients with higher total sleep volume, total sleep time, and continuous sleep volume had better overall sleep perception.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):458-467
DOI 10.5935/0103-507X.20200076
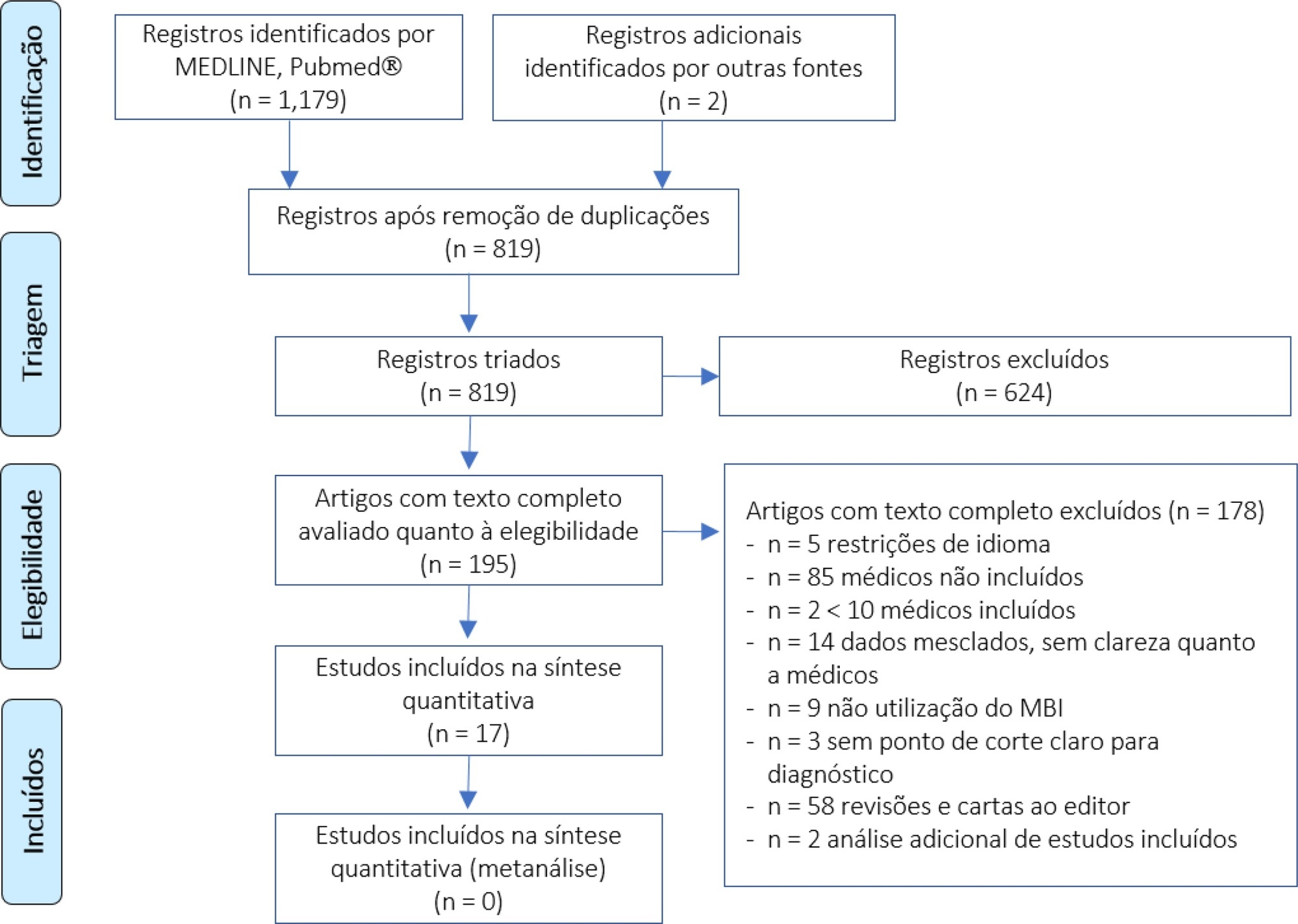
We performed a systematic review to summarize the knowledge regarding the prevalence of burnout among intensive care unit physicians.
We conducted a systematic review of the MEDLINE and PubMed® databases (last update 04.02.2019) with the goal of summarizing the evidence on burnout among intensive care unit physicians. We included all studies reporting burnout in intensive care unit personnel according to the Maslach Burnout Inventory questionnaire and then screened studies for data on burnout among intensive care unit physician specifically.
We found 31 studies describing burnout in intensive care unit staff and including different healthcare profiles. Among these, 5 studies focused on physicians only, and 12 others investigated burnout in mixed intensive care unit personnel but provided separate data on physicians. The prevalence of burnout varied greatly across studies (range 18% - 49%), but several methodological discrepancies, among them cut-off criteria for defining burnout and variability in the Likert scale, precluded a meaningful pooled analysis.
The prevalence of burnout syndrome among intensive care unit physicians is relatively high, but significant methodological heterogeneities warrant caution being used in interpreting our results. The lower reported levels of burnout seem higher than those found in studies investigating mixed intensive care unit personnel. There is an urgent need for consensus recommending a consistent use of the Maslach Burnout Inventory test to screen burnout, in order to provide precise figures on burnout in intensive care unit physicians.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):374-380
DOI 10.5935/0103-507X.20200065
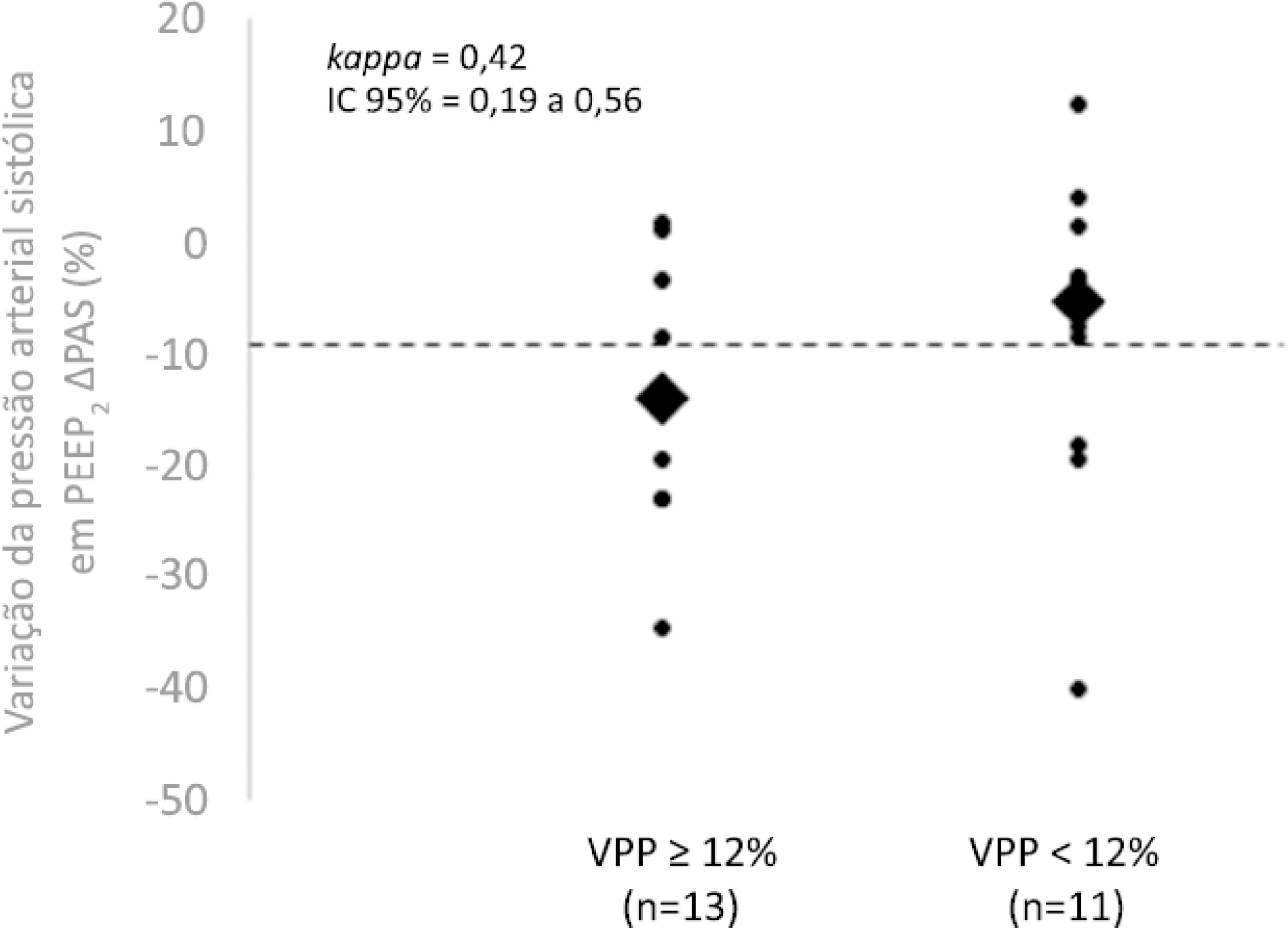
To evaluate whether the decrease in blood pressure caused by the increase in the positive end-expiratory pressure corresponds to the pulse pressure variation as an indicator of fluid responsiveness.
This exploratory study prospectively included 24 patients with septic shock who were mechanically ventilated and subjected to three stages of elevation of the positive end-expiratory pressure: from 5 to 10cmH2O (positive end-expiratory pressure level 1), from 10 to 15cmH2O (positive end-expiratory pressure level 2), and from 15 to 20cmH2O (positive end-expiratory pressure level 3). Changes in systolic blood pressure, mean arterial pressure, and pulse pressure variation were evaluated during the three maneuvers. The patients were classified as responsive (pulse pressure variation ≥ 12%) or unresponsive to volume replacement (pulse pressure variation < 12%).
The best performance at identifying patients with pulse pressure variation ≥ 12% was observed at the positive end-expiratory pressure level 2: -9% systolic blood pressure variation (area under the curve 0.73; 95%CI: 0.49 - 0.79; p = 0.04), with a sensitivity of 63% and specificity of 80%. Concordance was low between the variable with the best performance (variation in systolic blood pressure) and pulse pressure variation ≥ 12% (kappa = 0.42; 95%CI: 0.19 - 0.56). The systolic blood pressure was < 90mmHg at positive end-expiratory pressure level 2 in 29.2% of cases and at positive end-expiratory pressure level 3 in 41.63% of cases.
Variations in blood pressure in response to the increase in positive end-expiratory pressure do not reliably reflect the behavior of the pulse pressure as a measure to identify the fluid responsiveness status.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):381-390
DOI 10.5935/0103-507X.20200066
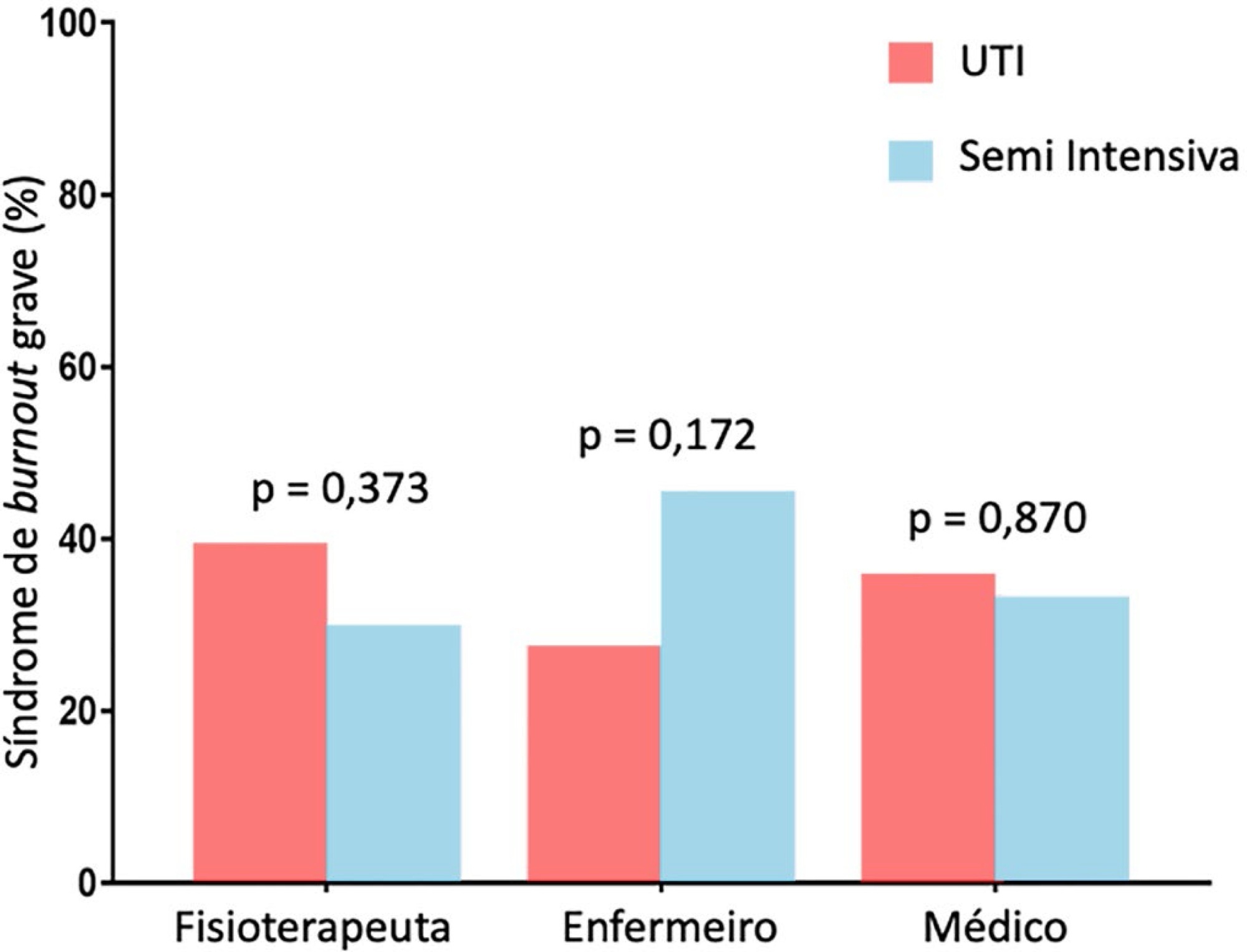
To evaluate the frequency of severe burnout syndrome among critical care providers and to correlate it with work engagement.
A self-administered survey including the Maslach Burnout Inventory, Depression Anxiety and Stress Scales, and Gallup questionnaire was distributed. All analyses were stratified by setting (intensive care unit or step-down unit) and by professional group (nurses versus physicians versus physiotherapists).
Between February 2017 and June 2017, 206 out of 325 invited professionals (63.4%) answered the questionnaires. Of these, 55 were physicians (26.7%), 88 were physiotherapists (42.7%) and 63 were nurses (30.6%). The frequency of severe burnout was 34.3% (27.9 - 41.4%), and no difference was found between professional groups or settings. The frequency of severe or very severe cases of depression, anxiety or stress was 12.9%, 11.4% and 10.5%, respectively. The median (interquartile range) score observed on the Gallup questionnaire was 41 (34 - 48), and no differences were found between professional groups or settings. There was a negative correlation between burnout and work engagement (r = -0.148; p = 0.035).
There is a high frequency of severe burnout among critical care providers working in the intensive care unit and step-down unit. There was a negative correlation between burnout and work engagement.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):412-417
DOI 10.5935/0103-507X.20200070
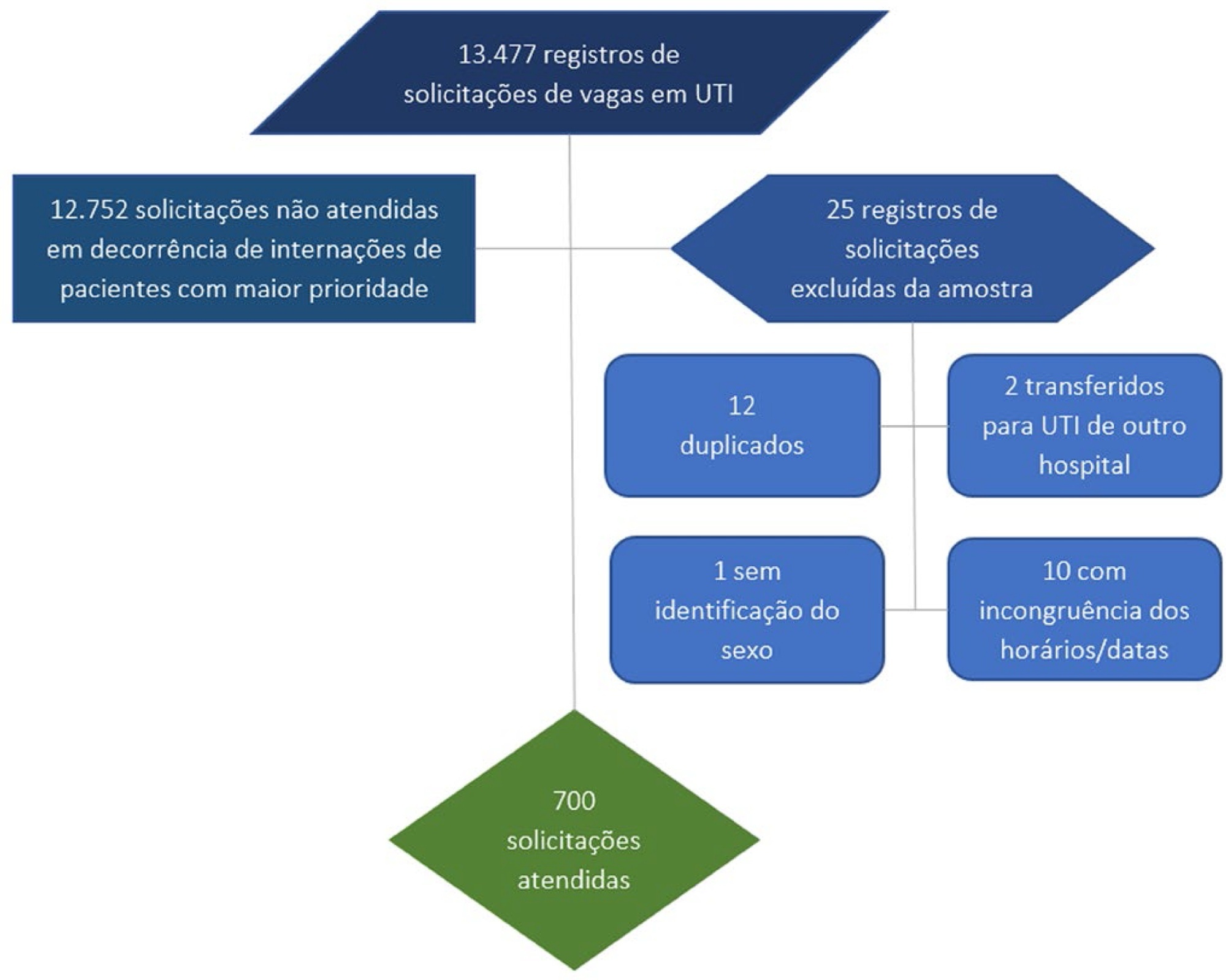
To evaluate the vacancy and occupancy times of intensive care unit beds; to analyze differences in these times between the day and night shifts and weekdays, weekends, and holidays; and to identify predictors of vacancy and occupancy times.
This was a cross-sectional, observational, descriptive, analytical, inferential study. A total of 700 vacancy-to-occupancy records from 54 beds of an adult intensive care unit of a public hospital in Sergipe, Brazil, dated between January and December 2018 were analyzed. The nonparametric Mann-Whitney test was used for comparisons between groups. Several predictive models of length of stay were constructed. The incidence rate ratio was used to estimate the effect size.
During the study period, there were 13,477 requests for the 54 intensive care unit beds, and only 5% (700 patients) were granted. The vacancy-to-occupancy times were shorter when beds were occupied at night (incidence rate ratio of 0.658; 95%CI 0.550 - 0.787; p < 0.0001) or on weekends (incidence rate ratio of 0.566; 95%CI 0.382 - 0.838; p = 0.004). Female sex (incidence rate ratio of 0.749; 95%CI 0.657 - 0.856; p < 0.0001) was a predictor of shorter vacancy-to-occupancy time. This time tended to increase with patient age (incidence rate ratio of 1.006; 95% CI 1.003 - 1.009; p < 0.0001).
Disparities in the waiting time for intensive care unit beds were identified, as the time was greater in the daytime and on weekdays, and women and younger patients experienced shorter vacancy-to-occupancy times.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):426-432
DOI 10.5935/0103-507X.20200072
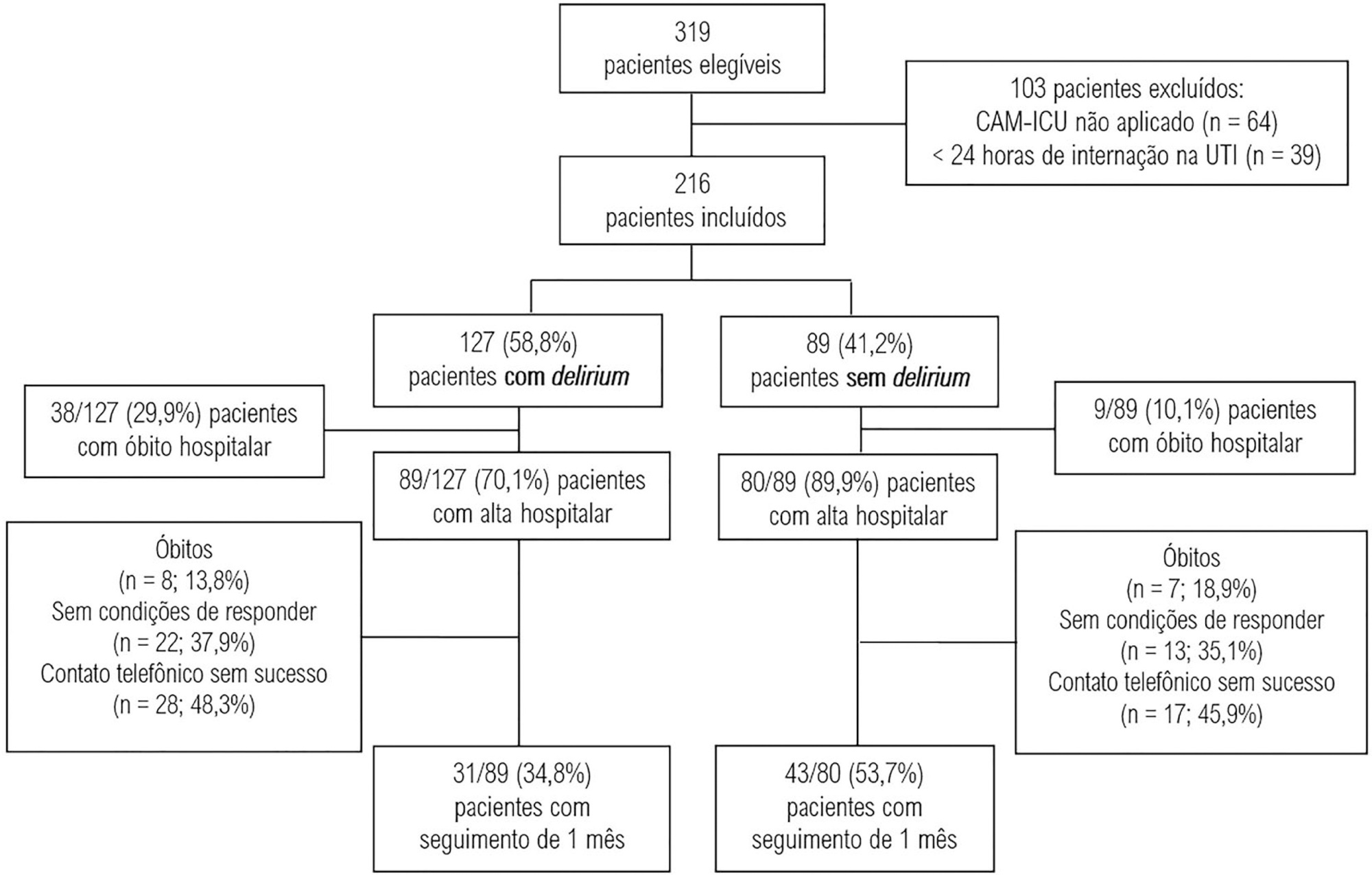
To evaluate the association between the incidence of delirium in the intensive care unit and quality of life 1 month after hospital discharge.
This was a prospective cohort study conducted in the intensive care units of two medium-complexity hospitals from December 2015 to December 2016. Delirium was identified using the Confusion Assessment Method for the Intensive Care Unit scale. At the time of hospital discharge, functional capacity and cognition were assessed with the Barthel index and the Mini Mental State Examination, respectively. Thirty days after patient discharge, the World Health Organization Quality of Life-BREF questionnaire was administered by telephone.
A total of 216 patients were included. Delirium was identified in 127 (58.8%) of them. Patients with delirium exhibited greater functional dependence (median Barthel index 50.0 [21.2 - 70.0] versus 80.0 [60.0 - 95.0]; p < 0.001) and lower cognition (Mini Mental State Examination score 12.9 ± 7.5 versus 20.7 ± 9.8; p < 0.001) at hospital discharge. There was no difference in any of the quality-of-life domains evaluated 1 month after hospital discharge between patients with and without delirium.
Our findings suggest that patients with delirium in the intensive care unit do not have worse quality of life 1 month after hospital discharge, despite presenting greater cognitive impairment and functional disability at the time of hospital discharge.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):433-438
DOI 10.5935/0103-507X.20200073
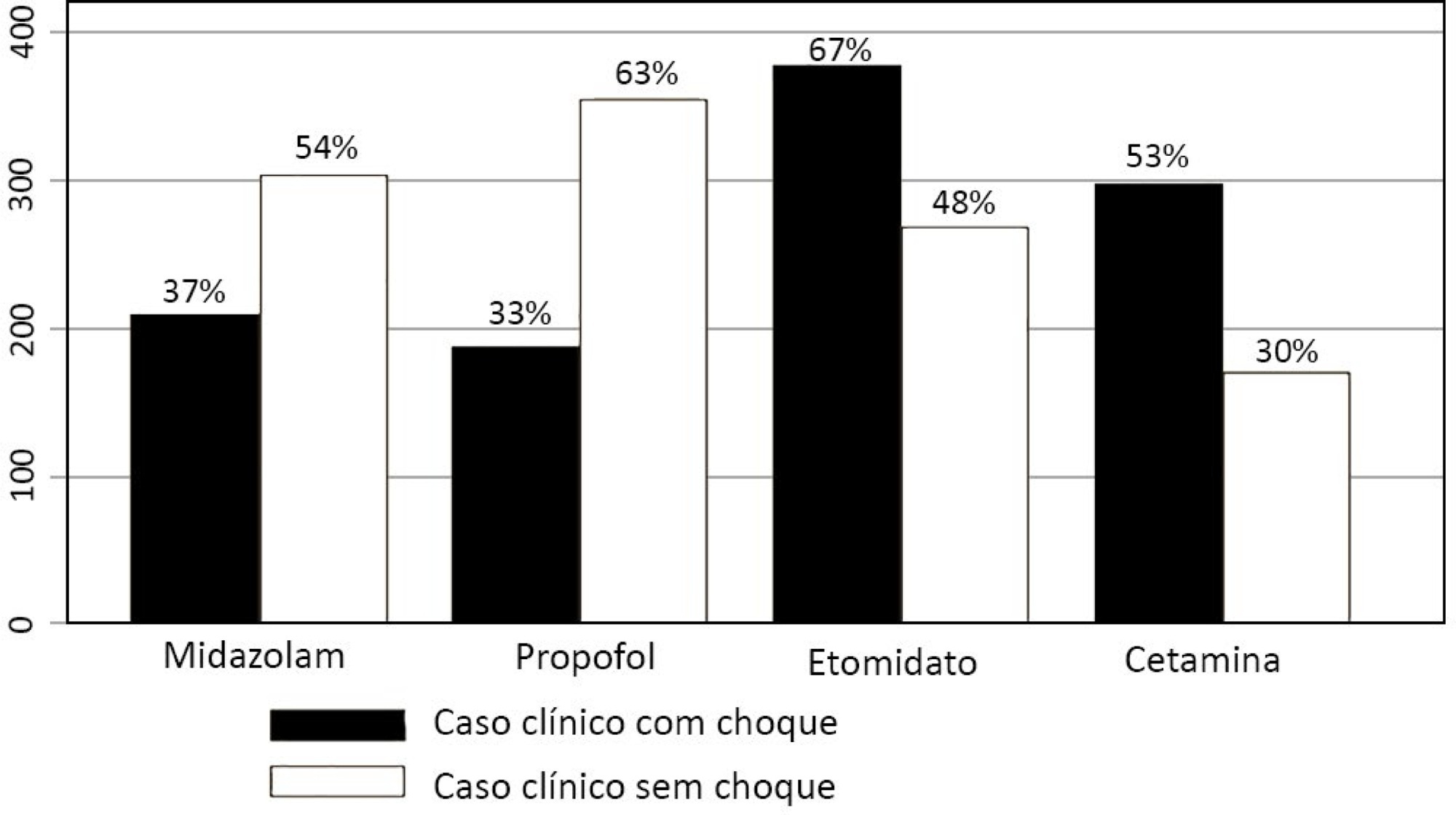
To describe the use of neuromuscular blockade as well as other practices among Brazilian physicians in adult intensive care units.
An online national survey was designed and administered to Brazilian intensivists. Questions were selected using the Delphi method and assessed physicians’ demographic data, intensive care unit characteristics, practices regarding airway management, use of neuromuscular blockade and sedation during endotracheal intubation in the intensive care unit. As a secondary outcome, we applied a multivariate analysis to evaluate factors associated with the use of neuromuscular blockade.
Five hundred sixty-five intensivists from all Brazilian regions responded to the questionnaire. The majority of respondents were male (65%), with a mean age of 38 ( 8.4 years, and 58.5% had a board certification in critical care. Only 40.7% of the intensivists reported the use of neuromuscular blockade during all or in more than 75% of endotracheal intubations. In the multivariate analysis, the number of intubations performed monthly and physician specialization in anesthesiology were directly associated with frequent use of neuromuscular blockade. Etomidate and ketamine were more commonly used in the clinical situation of hypotension and shock, while propofol and midazolam were more commonly prescribed in the situation of clinical stability.
The reported use of neuromuscular blockade was low among intensivists, and sedative drugs were chosen in accordance with patient hemodynamic stability. These results may help the design of future studies regarding airway management in Brazil.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):251-260
DOI 10.5935/0103-507X.20200036
To assess the prevalence of and factors associated with Burnout syndrome among intensive care unit professionals.
In this cross-sectional population-based study, a questionnaire assessing sociodemographic, behavioral, and occupational data was administered to 241 nurses and physicians working in 17 public intensive care units in São Luis (MA), Brazil. The Maslach Burnout Inventory - Human Services Survey was used to identify Burnout syndrome based on Maslach’s and Grunfeld’s criteria. The prevalence of each dimension of the syndrome was estimated with a 95% confidence interval. Associations were estimated by the odds ratios via multiple logistic regression analyses (α = 5%).
The prevalence of Burnout syndrome was 0.41% (0.01 - 2.29) according to Maslach’s criteria and 36.9% (30.82 - 43.36) according to Grunfeld’s criteria. Infant intensive care unit professionals were more likely to develop emotional exhaustion than other intensive care professionals (OR = 3.16). Respondents over the age of 35 were less likely to develop emotional exhaustion (OR = 0.32) and depersonalization (OR = 0.06). Longer working hours in intensive care units were associated with a reduced sense of personal accomplishment (OR = 1.13). Among nurses, males had a lower sense of professional accomplishment, and not exercising regularly was associated with more emotional exhaustion and less depersonalization. Among physicians, working in infant and cardiology intensive care units made them less likely to have a reduced sense of personal accomplishment, and physicians without a postgraduate degree who worked in intensive care units had a higher chance of having a lower sense of personal accomplishment.
This study demonstrated the low prevalence of Burnout syndrome. Most of the professionals reported low levels for each dimension of Burnout, including low levels of emotional exhaustion, low levels of depersonalization, and a lower likelihood of having a reduced sense of personal accomplishment. Nurses and physicians have different characteristics associated with Burnout syndrome.