Abstract
Rev Bras Ter Intensiva. 2021;33(4):537-543
DOI 10.5935/0103-507X.20210081
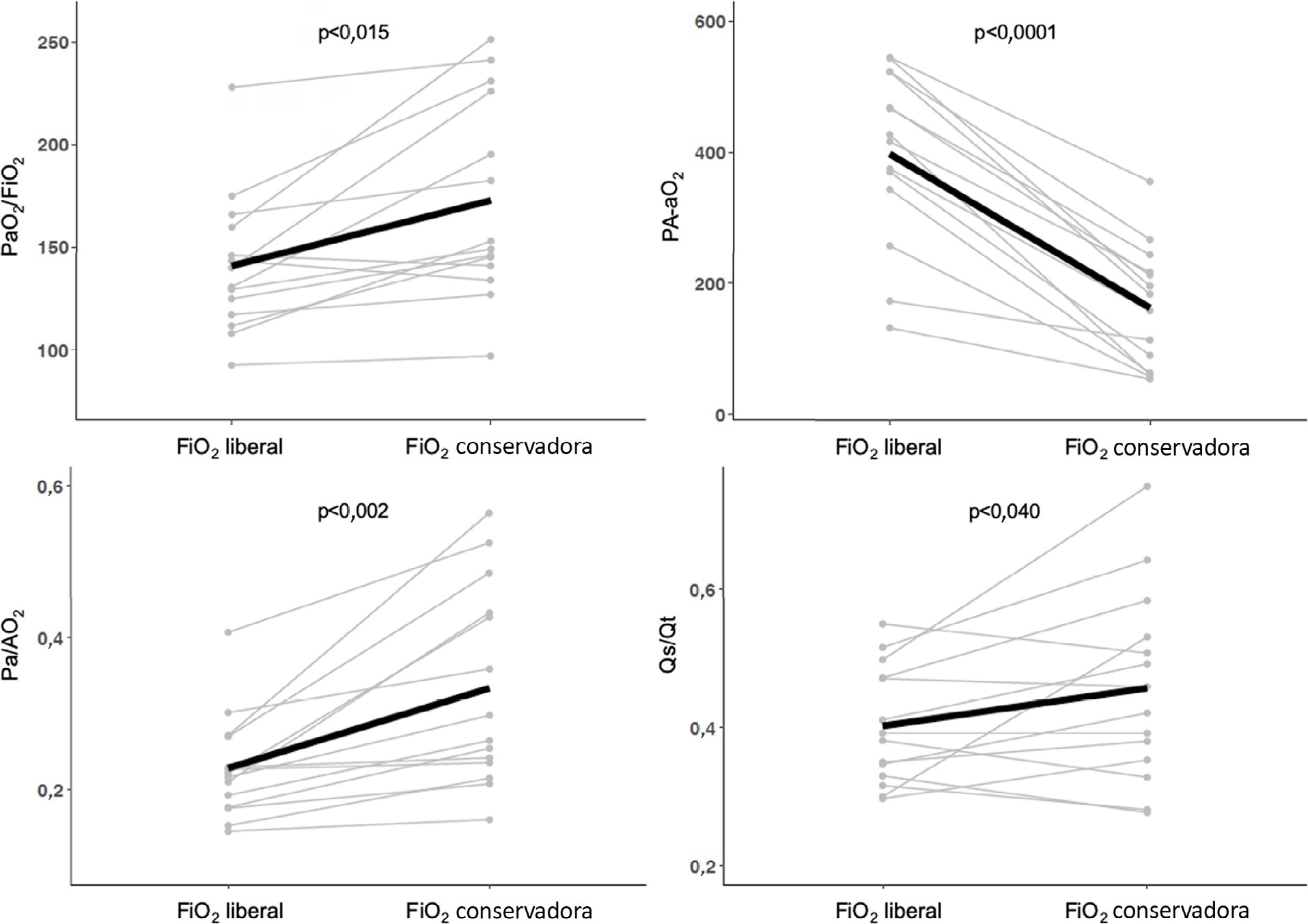
To compare gas exchange indices behavior by using liberal versus conservative oxygenation targets in patients with moderate to severe acute respiratory distress syndrome secondary to COVID-19 under invasive mechanical ventilation. We also assessed the influence of high FiO2 on respiratory system mechanics.
We prospectively included consecutive patients aged over 18 years old with a diagnosis of COVID-19 and moderate-severe acute respiratory distress syndrome. For each patient, we randomly applied two FiO2 protocols to achieve SpO2 88% - 92% or 96%. We assessed oxygenation indices and respiratory system mechanics.
We enrolled 15 patients. All the oxygenation indices were significantly affected by the FiO2 strategy (p < 0.05) selected. The PaO2/FiO2 deteriorated, PA-aO2 increased and Pa/AO2 decreased significantly when using FiO2 to achieve SpO2 96%. Conversely, the functional shunt fraction was reduced. Respiratory mechanics were not affected by the FiO2 strategy.
A strategy aimed at liberal oxygenation targets significantly deteriorated gas exchange indices, except for functional shunt, in COVID-19-related acute respiratory distress syndrome. The respiratory system mechanics were not altered by the FiO2 strategy.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):572-582
DOI 10.5935/0103-507X.20210084
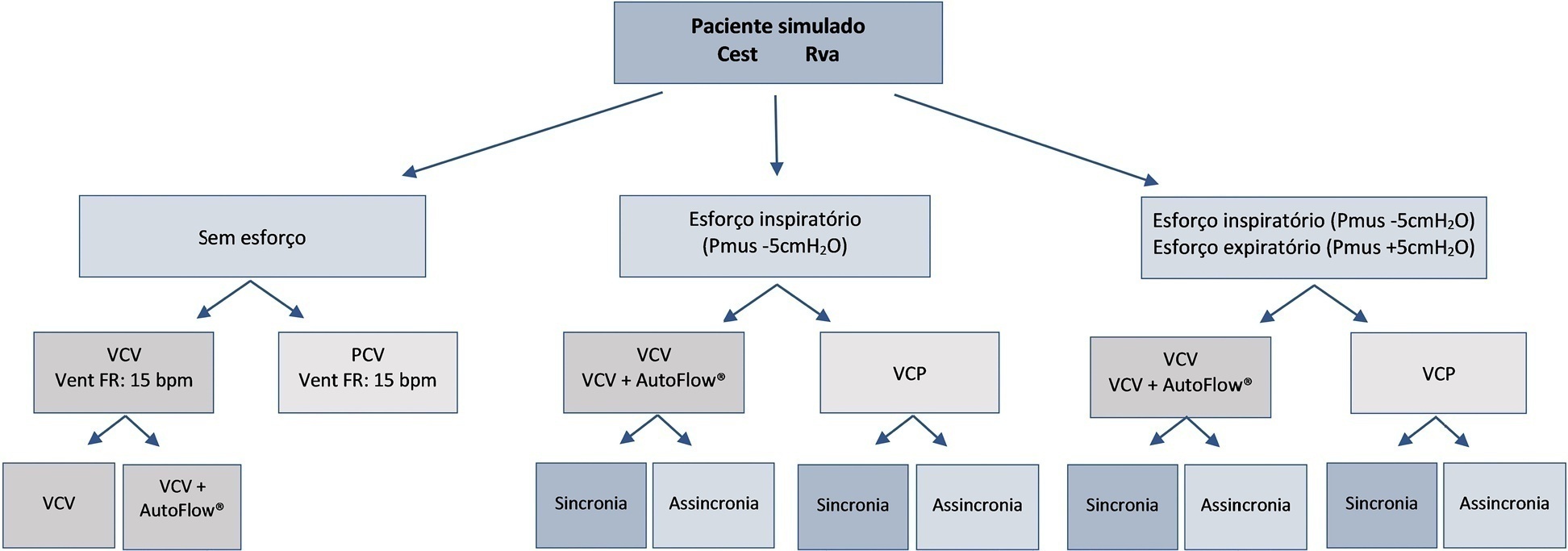
To evaluate the influences of respiratory muscle efforts and respiratory rate setting in the ventilator on tidal volume and alveolar distending pressures at end inspiration and expiration in volume-controlled ventilation and pressure-controlled ventilation modes in acute respiratory distress syndrome.
An active test lung (ASL 5000™) connected to five intensive care unit ventilators was used in a model of acute respiratory distress syndrome. Respiratory muscle efforts (muscle pressure) were configured in three different ways: no effort (muscle pressure: 0cmH2O); inspiratory efforts only (muscle pressure:-5cmH2O, neural inspiratory time of 0.6s); and both inspiratory and expiratory muscle efforts (muscle pressure:-5/+5cmH2O). Volume-controlled and pressure-controlled ventilation modes were set to deliver a target tidal volume of 420mL and positive end-expiratory pressure of 10cmH2O. The tidal volume delivered to the lungs, alveolar pressures at the end of inspiration, and alveolar pressures at end expiration were evaluated.
When triggered by the simulated patient, the median tidal volume was 27mL lower than the set tidal volume (range-63 to +79mL), and there was variation in alveolar pressures with a median of 25.4cmH2O (range 20.5 to 30cmH2O). In the simulated scenarios with both spontaneous inspiratory and expiratory muscle efforts and with a mandatory respiratory rate lower than the simulated patient's efforts, the median tidal volume was higher than controlled breathing.
Adjusting respiratory muscle effort and pulmonary ventilator respiratory rate to a value above the patient’s respiratory rate in assisted/controlled modes generated large variations in tidal volume and pulmonary pressures, while the controlled mode showed no variations in these outcomes.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
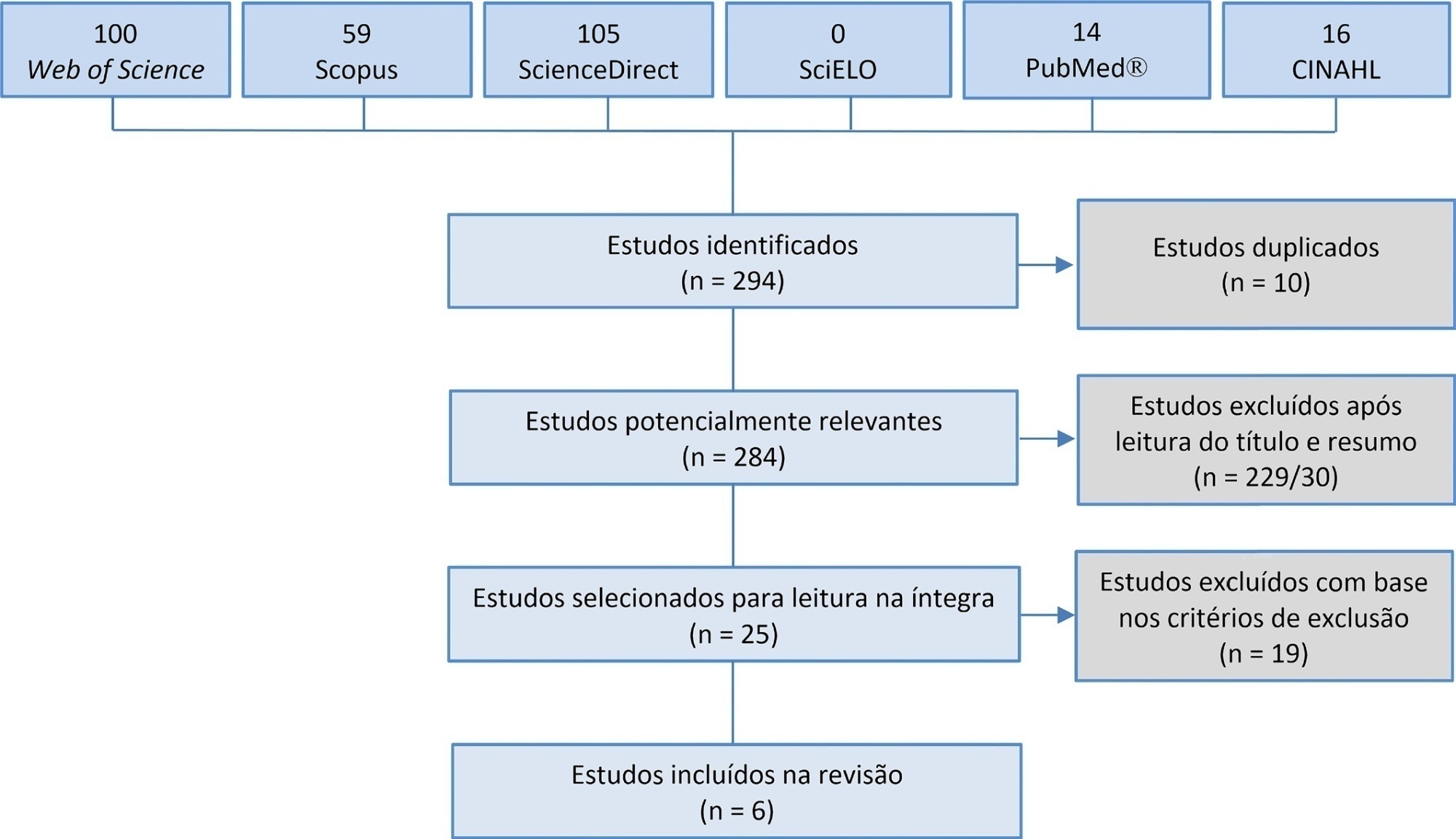
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):428-433
DOI 10.5935/0103-507X.20210068
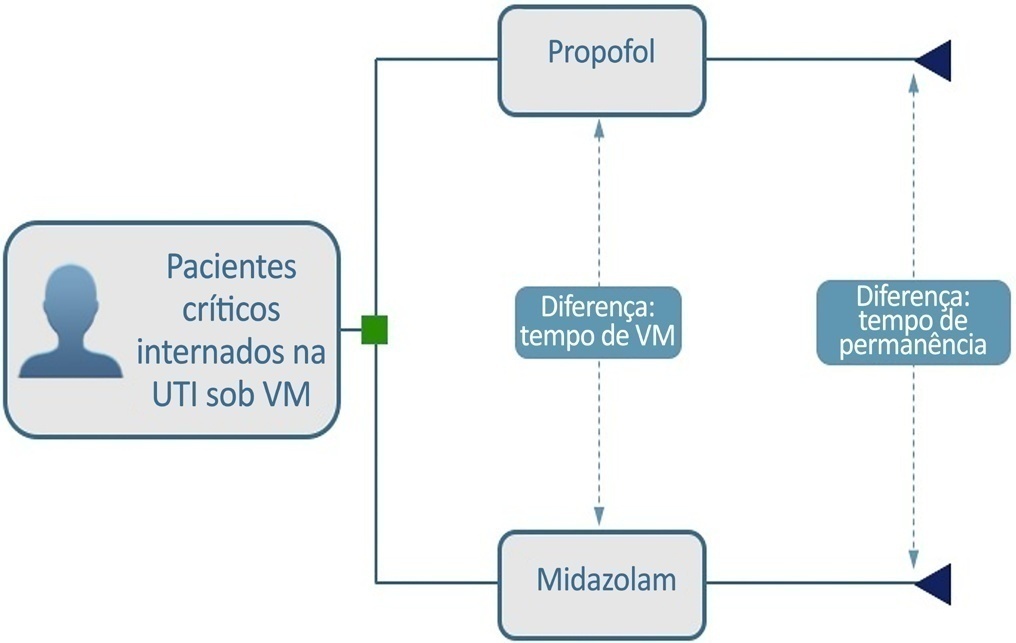
To build a cost-effectiveness model to compare the use of propofol versus midazolam in critically ill adult patients under mechanical ventilation.
We built a decision tree model for critically ill patients submitted to mechanical ventilation and analyzed it from the Brazilian private health care system perspective. The time horizon was that of intensive care unit hospitalization. The outcomes were cost-effectiveness per hour of intensive care unit stay avoided and cost-effectiveness per hour of mechanical ventilation avoided. We retrieved data for the model from a previous meta-analysis. We assumed that the cost of medication was embedded in the intensive care unit cost. We conducted univariate and probabilistic sensitivity analyses.
Mechanically ventilated patients using propofol had their intensive care unit stay and the duration of mechanical ventilation decreased by 47.97 hours and 21.65 hours, respectively. There was an average cost reduction of US$ 2,998.971 for propofol when compared to midazolam. The cost-effectiveness per hour of intensive care unit stay and mechanical ventilation avoided were dominant 94.40% and 80.8% of the time, respectively.
There was a significant reduction in costs associated with propofol use related to intensive care unit stay and duration of mechanical ventilation for critically ill adult patients.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):445-456
DOI 10.5935/0103-507X.20210060
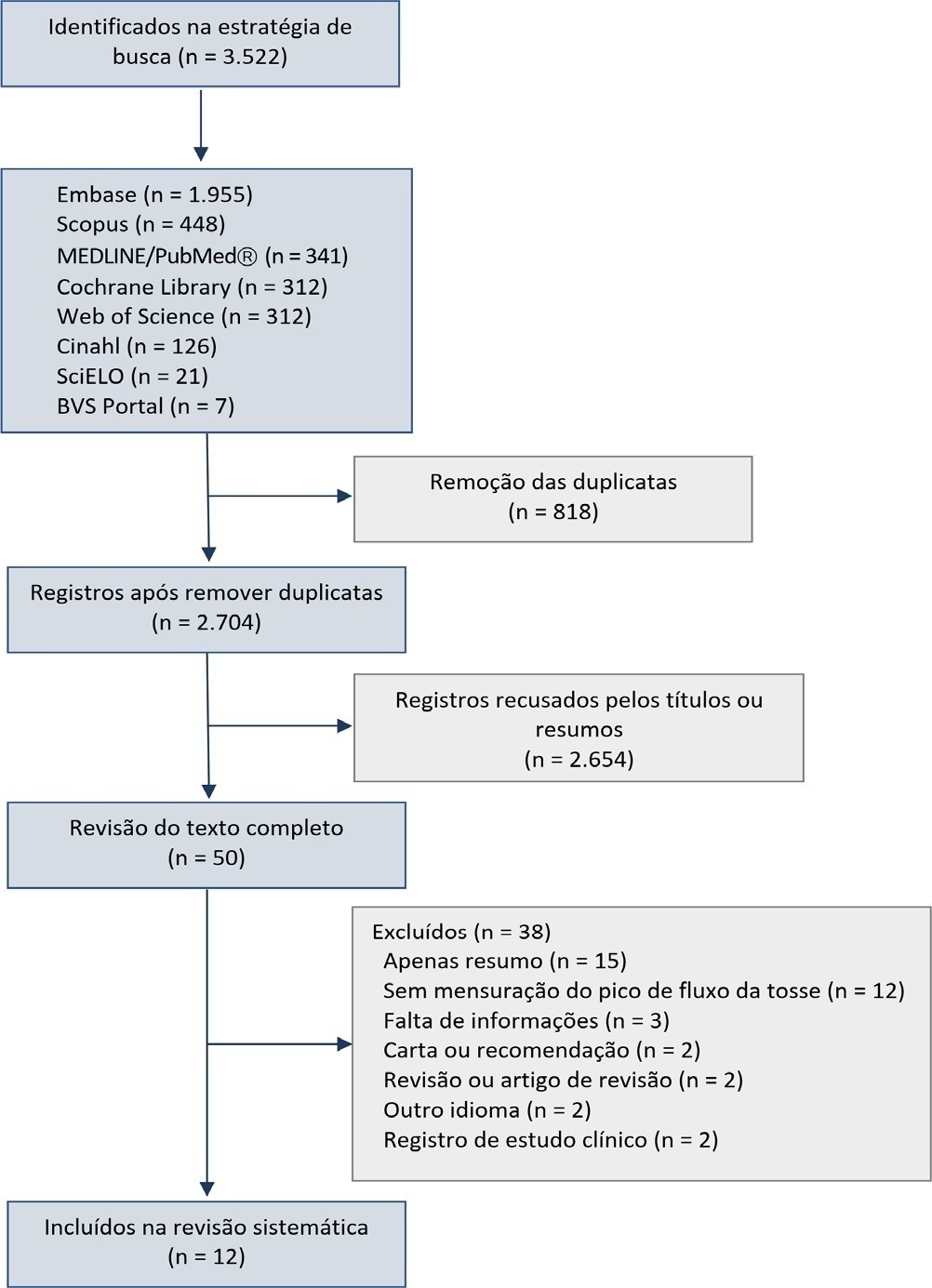
This systematic review was designed to assess the usefulness of cough peak flow to predict the extubation outcome in subjects who passed a spontaneous breathing trial.
The search covered the scientific databases MEDLINE, Lilacs, Ibecs, Cinahl, SciELO, Cochrane, Scopus, Web of Science and gray literature. The Quality Assessment of Diagnostic Accuracy Studies was used to assess the methodological quality and risk of study bias. The statistical heterogeneity of the likelihood (LR) and diagnostic odds ratios were evaluated using forest plots and Cochran’s Q statistic, and a crosshair summary Receiver Operating Characteristic plot using the multiple cutoffs model was calculated.
We initially retrieved 3,522 references from the databases; among these, 12 studies including 1,757 subjects were selected for the qualitative analysis. Many studies presented an unclear risk of bias in the “patient selection” and “flow and time” criteria. Among the 12 included studies, seven presented “high risk” and five “unclear risk” for the item “reference standard.” The diagnostic performance of the cough peak flow for the extubation outcome was low to moderate when we considered the results from all included studies, with a +LR of 1.360 (95%CI 1.240 - 1.530), -LR of 0.218 (95%CI 0.159 - 0.293) and a diagnostic odds ratio of 6.450 (95%CI 4.490 - 9.090). A subgroup analysis including only the studies with a cutoff between 55 and 65 L/minute showed a slightly better, although still moderate, performance.
A cough peak flow assessment considering a cutoff between 55 and 65L/minute may be useful as a complementary measurement prior to extubation. Additional well-designed studies are necessary to identify the best method and equipment to record the cough peak flow as well as the best cutoff.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):461-468
DOI 10.5935/0103-507X.20210061
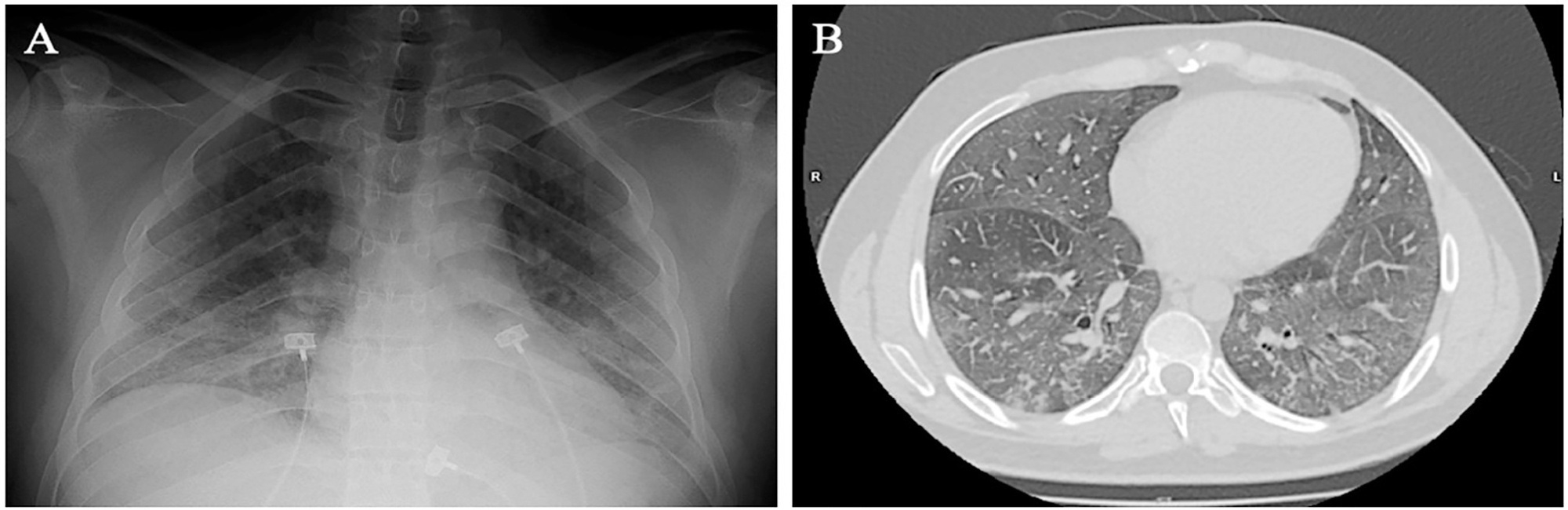
Spontaneous breathing can be deleterious in patients with previously injured lungs, especially in acute respiratory distress syndrome. Moreover, the failure to assume spontaneous breathing during mechanical ventilation and the need to switch back to controlled mechanical ventilation are associated with higher mortality. There is a gap of knowledge regarding which parameters might be useful to predict the risk of patient self-inflicted lung injury and to detect the inability to assume spontaneous breathing. We report a case of patient self-inflicted lung injury, the corresponding basic and advanced monitoring of the respiratory system mechanics and physiological and clinical results related to spontaneous breathing. The patient was a 33-year-old Caucasian man with a medical history of AIDS who developed acute respiratory distress syndrome and needed invasive mechanical ventilation after noninvasive ventilatory support failure. During the controlled ventilation periods, a protective ventilation strategy was adopted, and the patient showed clear clinical and radiographic improvement. However, during each spontaneous breathing period under pressure support ventilation, despite adequate initial parameters and a strictly adjusted ventilatory setting and monitoring, the patient developed progressive hypoxemia and worsening of respiratory system mechanics with a clearly correlated radiographic deterioration (patient self-inflicted lung injury). After failing three spontaneous breathing assumption trials, he died on day 29 due to refractory hypoxemia. Conventional basic and advanced monitoring variables in this case were not sufficient to identify the aptitude to breathe spontaneously or to predict the risk and development of patient self-inflicted lung injury during partial support ventilation.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):284-292
DOI 10.5935/0103-507X.20150048
Evidence-based practices search for the best available scientific evidence to support problem solving and decision making. Because of the complexity and amount of information related to health care, the results of methodologically sound scientific papers must be integrated by performing literature reviews. Although endotracheal suctioning is the most frequently performed invasive procedure in intubated newborns in neonatal intensive care units, few Brazilian studies of good methodological quality have examined this practice, and a national consensus or standardization of this technique is lacking. Therefore, the purpose of this study was to review secondary studies on the subject to establish recommendations for endotracheal suctioning in intubated newborns and promote the adoption of best-practice concepts when conducting this procedure. An integrative literature review was performed, and the recommendations of this study are to only perform endotracheal suctioning in newborns when there are signs of tracheal secretions and to avoid routinely performing the procedure. In addition, endotracheal suctioning should be conducted by at least two people, the suctioning time should be less than 15 seconds, the negative suction pressure should be below 100 mmHg, and hyperoxygenation should not be used on a routine basis. If indicated, oxygenation is recommended with an inspired oxygen fraction value that is 10 to 20% greater than the value of the previous fraction, and it should be performed 30 to 60 seconds before, during and 1 minute after the procedure. Saline instillation should not be performed routinely, and the standards for invasive procedures must be respected.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)