Abstract
Rev Bras Ter Intensiva. 2010;22(1):11-18
DOI 10.1590/S0103-507X2010000100004
OBJECTIVE: This study aimed to evaluate the outcome of cirrhotic patients admitted to Intensive Care Unit. METHODS: We conducted a prospective cohort of cirrhotic patients admitted to two intensive care unit between June 1999 to September 2004. We collected demographic, comorbid conditions, diagnosis, vital signs, laboratory data, prognostic scores and evolution in intensive care unit and hospital. The patients were divided in groups: non surgical, non liver surgery, surgery for portal hypertension, liver surgery, liver transplantation, and urgent surgery. RESULTS: We studied 304 patients, which 190 (62.5%) were male. The median of age was 54 (47-61) years. The mortality rate in intensive care unit and hospital were 29.3 and 39.8%, respectively, more elevated than in the other patients admitted critically ill patients (19.6 and 28.3%; p<0.001). Non surgical patients and those submitted to urgent surgery presented high mortality rate in the intensive care unit (64.3 and 65.4%) and in the hospital (80.4 and 76.9%). The variables related to hospital mortality were [Odds ratio (confidence interval 95%)]: mean arterial pressure [0.985 (0.974-0.997)]; mechanical ventilation in the first 24 h [4.080 (1.990-8.364)]; confirmed infection in the first 24 h [7.899 (2.814-22.175)]; acute renal failure [5.509 (1.708-17.766)] and APACHE II score (points) [1.078 (1.017-1.143)]. CONCLUSIONS: Cirrhotic patients had higher mortality rate compared to non cirrhotic critically ill patients. Those admitted after urgent surgery and non surgical had higher mortality rate.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):398-403
DOI 10.1590/S0103-507X2009000400010
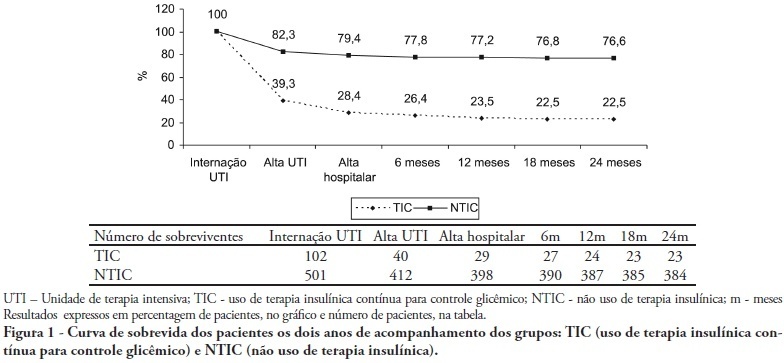
OBJECTIVES: Stress-induced hyperglycemia is frequent in critically ill patients and has been associated with increased mortality and morbidity (both in diabetic and non-diabetic patients). This study objective was to evaluate the profile and long-term prognosis of critically ill patients undergoing tight glucose-control. METHODS: Prospective cohort. All patients admitted to the intensive care unit over 1-year were enrolled. We analyzed demographic data, therapeutic intervention, and short- (during the stay) and long-term (2 years after discharge) mortality. The patients were categorized in 2 groups: tight glucose control and non-tight glucose-control, based on the unit staff decision. RESULTS: From the 603 enrolled patients, 102 (16.9%) underwent tight control (glucose <150 mg/dL) while 501 patients (83.1%) non-tight control. Patients in the TGC-group were more severely ill than those in the non-tight control group [APACHE II score (14 ± 3 versus 11 ± 4, P=0.04), SOFA (4.9 ± 3.2 versus 3.5 ± 3.4, P<0.001) and TISS-24h (25.7 ± 6.9 versus 21.1 ± 7.2, P< 0.001)]. The tight control group patients also had worse prognosis: [acute renal failure (51% versus 18.5%, P<0.001), critical illness neuropathy (16.7% versus 5.6%, P<0.001)] and increased mortality (during the ICU-stay [60.7% versus 17.7%, P<0.001] and within 2-years of the discharge [77.5% versus 23.4%; P<0.001]). CONCLUSION: Critically ill patients needing tight glucose control during the unit stay have more severe disease and have worse short and long-term prognosis.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):425-431
DOI 10.1590/S0103-507X2009000400013
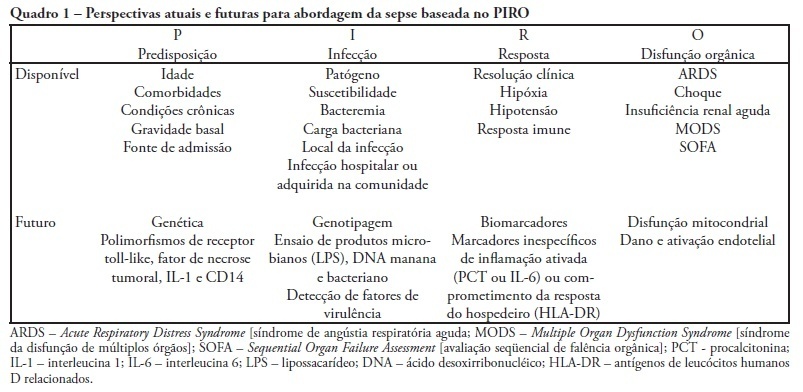
Despite recent advances in diagnosis and care of critically ill patients sepsis related mortality rate remains unacceptably high. Therefore, new methods of evaluation are necessary to provide an earlier and more accurate characterization of septic patients. Based on the (oncologic) TNM system, the PIRO concept was introduced as a new staging system for sepsis in order to assess risk and predict prognosis, with potential to assist in inclusion of patients in clinical studies and estimate the probability of response of patients to specific therapeutic interventions.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):255-261
DOI 10.1590/S0103-507X2009000300004
Currently, aging of the population is a widespread global phenomenon. Therefore, the assessment of prognosis in elderly patients is needed. This study aims to identify risk factors in a population of elderly patients admitted in the intensive care unit METHODS: A prospective study in the intensive care unit of a general tertiary hospital was carried out for five months. Patients with 65 years or more of age, who stayed in the intensive care unit for 24 hours or more were included and those at the-end-of-life, patients readmitted to intensive care unit during the same hospital stay were excluded. RESULTS: In this study 199 patients were involved, with a mean age of 75.4±6.8 years, and 58.8% were female. Mortality was 57.3%. The mean APACHE II, SOFA, MODS and Katz index (assessment of daily activities) were respectively 20.0±5.8, 6.8±3.9, 2.4±1.9 and 5.3±1.6. Most patients were postoperative 59.3% and 41.6% were under invasive mechanical ventilation. At regression analysis, the independent determinants of higher mortality were: older age (76.9±6.7 years death versus 73.3±6.5 years discharge, P<0.001, OR=1.08, CI 95% 1.01-1. 16), the Katz index (4.9±1.9 deaths versus 5.7±0.9 discharge, p=0.001, OR=0.66, CI 95% 0.45-0.98), hyperglycemia (158.1±69.0 death versus 139.6±48.5 discharge p=0.041; OR=1.02; CI 95% 1.01-1.03) and need for mechanical ventilation at admission to the intensive care unit (57.0% death versus 20.5% discharge p <0.001, OR=3.57, CI 95% 1.24-10.3). CONCLUSION: Elderly patients admitted to the intensive care unit that have difficulties in performing daily activities, hyperglycemia and who are under invasive mechanical ventilation had a worse hospital prognosis.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):1-8
DOI 10.1590/S0103-507X2009000100001
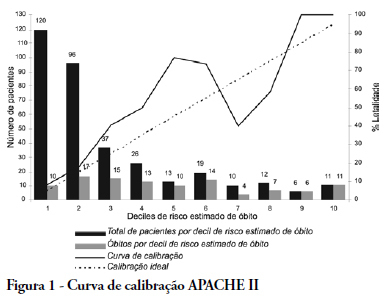
OBJECTIVE: The elderly constitute a population with their own features and frequent admissions in intensive care units. This study has the objective to evaluate the ability to predict the survival of these patients through the APACHE II, UNICAMP II, SAPS II and SAPS 3 indexes, global and Central America/South equations. METHODS: Elderly patients admitted from 01/01/2006 to 12/3/2006, defined as age > 60 years, were included in this study. Those who were readmitted were excluded. The rate of lethality standardized, calibration and discrimination for each index in the remaining patients were analysed. The outcome were death or hospital discharge. RESULTS: Three hundred eighty six elderly patients were included in this study, being 36 excluded by readmission, remaining 350 for analysis. The rate of lethality standardized came near to the unit in all indexes, except the SAPS II (TLP=1.5455) which underestimated the lethality. The calibration, via Hosmer-Lemeshow tests was inadequate (p < 0.05), except for the UNICAMP II (p > 0.5). On the calibration curve, the models have distanced themselves from the pattern line. All of them presented an excellent discrimination via receiver operating characteristics curves (> 0.8). CONCLUSIONS: In the studied population, the models presented an excellent discrimination and inadequate calibration. SAPS II underestimated the lethality.
Abstract
Rev Bras Ter Intensiva. 2009;21(1):9-17
DOI 10.1590/S0103-507X2009000100002
OBJECTIVES: The objective of this study was to evaluate variables related to intra hospital mortality at 28 days, of aged persons with severe sepsis and septic shock in a clinical ICU. METHODS: One hundred and fifty-two patients aged > 65 years with severe sepsis and septic shock were followed for 28 days and the variables were collected on days 1, 3, 5, 7, 14 and 28 of stay. To compare categorical variables the Chi-square test was used and the Mann-Whitney or t test for continuous variables. All tests were double-tailed, alpha error of 0.05. RESULTS: Mean age was 82.0 ± 9.0 years and 64.5% were female. Mortality was of 47.4%. Related to death were the following: Acute Physiological and Chronic Heath Evaluation II score (p < 0.001), Sequential Organ Failure Assessment score on days 1, 3, 5, 7 (p < 0.001), length of stay in intensive care (p < 0.001), number of organ failures (p < 0.001), high serum lactate on day 3 (p = 0.05), positive troponin I (p < 0.01), echocardiographic variables (systolic diameter p = 0.005; diastolic diameter p = 0.05; shortening fraction p = 0.02), previous renal disease (p = 0.03), shock (p < 0.001), mechanical ventilation (p < 0.001) and Lawton scale (p = 0.04). CONCLUSIONS: Shock, elevated lactate, organ failure, especially respiratory were more prevalent in non-survivors. Heart dysfunction detected by echocardiographic variables and positive troponin I may play an important role in the mortality of aged patients with sepsis.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):411-421
DOI 10.1590/S0103-507X2008000400015
Trauma is the leading cause of death of people from 1 to 44 years of age. Traumatic brain injury is the main determinant for mortality and morbidity caused by trauma. Outcome prediction is one of the major problems related to severe traumatic brain injury because clinical evaluation has an unreliable predictive value and complicates identification of patients with higher risk of developing secondary lesions and fatal outcome. That is why, there is considerable interest in development of biomarkers that reflect the severity of brain injury and correlate with mortality and functional outcome. Proteins S100B and neuron specific enolases are among the markers most studied for this purpose, however some studies are investigating glial fibrillary acidic protein, creatinine phospokinase, isoenzime B, myelin basic protein, plasma desoxiribonucleic acid, heat shock protein 70, von Willebrand factor, metalloproteinases and brain-derived neurotrophic factor, among others. Evidence suggests that inflammation, oxidative stress, excitotoxicity, neuroendocrine responses and apoptosis play an important role in the development of secondary lesions. Markers involved in these processes are being studied in traumatic brain injury. We reviewed these biomarkers, some of which present promising results for future clinical application.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):226-234
DOI 10.1590/S0103-507X2008000300004
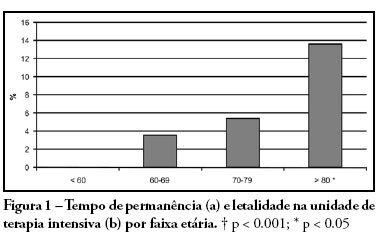
PURPOSE: Due to the increasing longevity of the and high prevalence of coronary heart disease in the aged , coronary artery bypass graft surgery has become frequent in older patients. The purpose of this study is to describe operative features, length of stay, complications and short term outcomes after coronary artery bypass graft in such patients. METHODS: From February 2005 to October 2007, 269 patients underwent coronary artery bypass graft. Demographic data, comorbidities, prognostic scores, coronary artery bypass graft elective versus urgent indication, intensive care unit length of stay, postoperative complications and intensive care unit mortality were recorded. Intra-operative characteristics, such as total surgery time, use of bypass device, on-pump time, urine output, fluid balance, use of blood products and number of grafts, were analyzed. Patients were divided in four age groups: group I (< 60 n = 68), II (60 to 69 n = 86), III (70 to 79 n = 93) IV and older than 80 years (n = 22). RESULTS: Group IV patients were more frequently submitted to coronary artery bypass graft combined with valve replacement, emergency surgery, and had longer stay in the intensive care unit (p < 0.01). The incidence of at least one postoperative complication was also higher among patients older than 80 (p < 0.001). Multivariate analysis identified age and on-pump time as independent risk factors for development of complications. Mortality increased in patients older than 70 years (p = 0.03). CONCLUSIONS: Octogenarian patients undergoing coronary artery bypass graft have longer intensive care unit length of stay, incidence of complications and mortality. Age and on-pump time were independent risk factors associated with the incidence of postoperative complications.