Abstract
Rev Bras Ter Intensiva. 2018;30(2):160-165
DOI 10.5935/0103-507X.20180034
To compare the prevalence of malnutrition during two time periods in a pediatric intensive care unit.
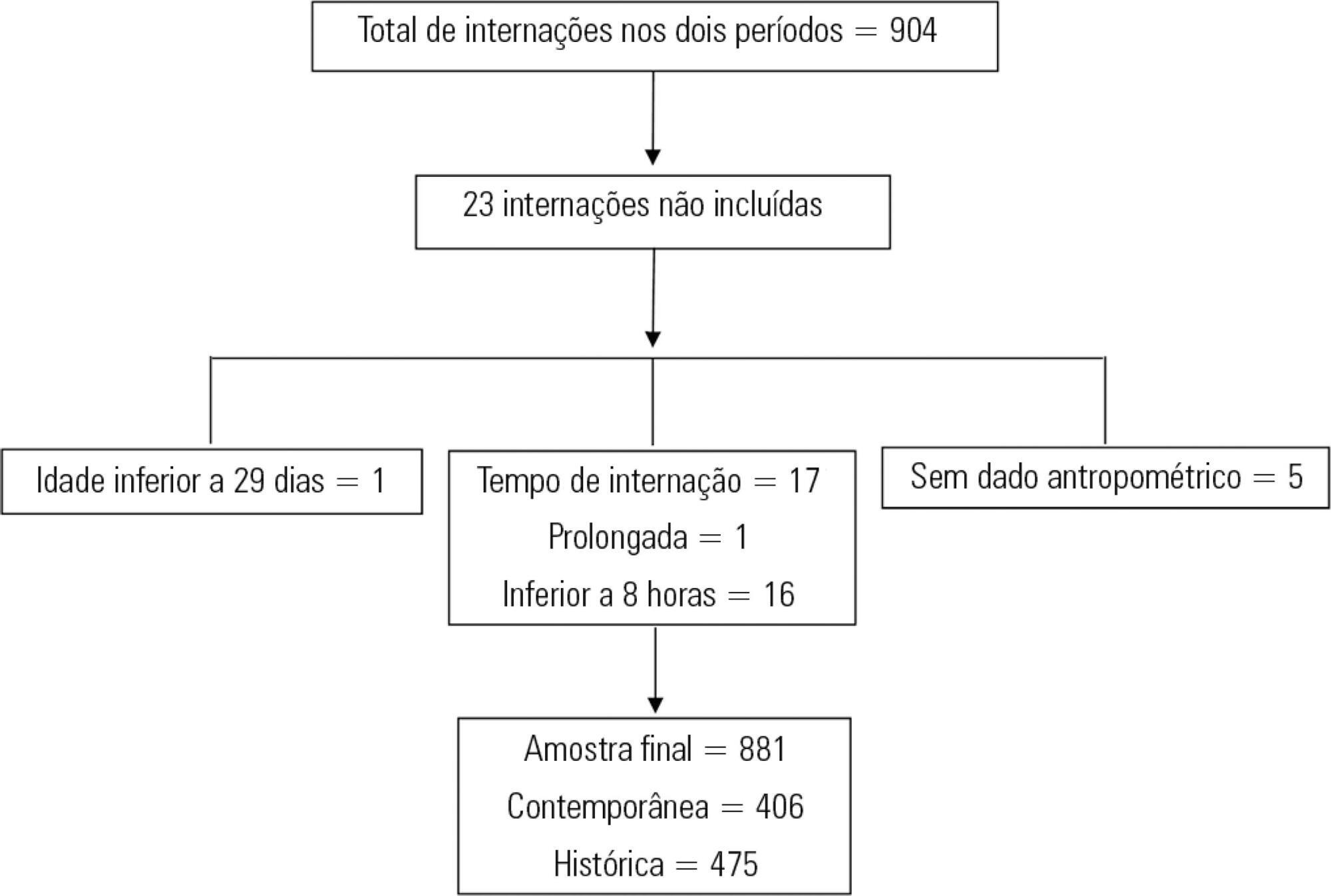
This was a retrospective cross-sectional study of patients admitted to the pediatric intensive care unit of a university hospital during two one-year periods with an interval of four years between them. Nutritional evaluation was conducted based on weight and height measured at admission. The body mass index-for-age was the parameter chosen to evaluate nutritional status, as classified according to the World Health Organization, according to age group.
The total sample size was 881 (406 in the contemporary sample and 475 in the historical sample). There was a significant reduction in malnutrition in the contemporary sample (p = 0.03). Malnourishment in patients in the historical sample was significantly associated with mortality and length of stay, while malnourishment in patients in the contemporary sample was not associated with worse outcomes.
There was a significant reduction in malnutrition among patients in the same pediatric intensive care unit when comparing the two time periods. Our findings of a change in nutritional profile in critically ill patients corroborate the nutritional status data of children and adolescents worldwide.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):366-375
DOI 10.5935/0103-507X.20180049
To evaluate the effectiveness of rapid response teams using early identification of clinical deterioration in reducing the occurrence of in-hospital mortality and cardiorespiratory arrest.
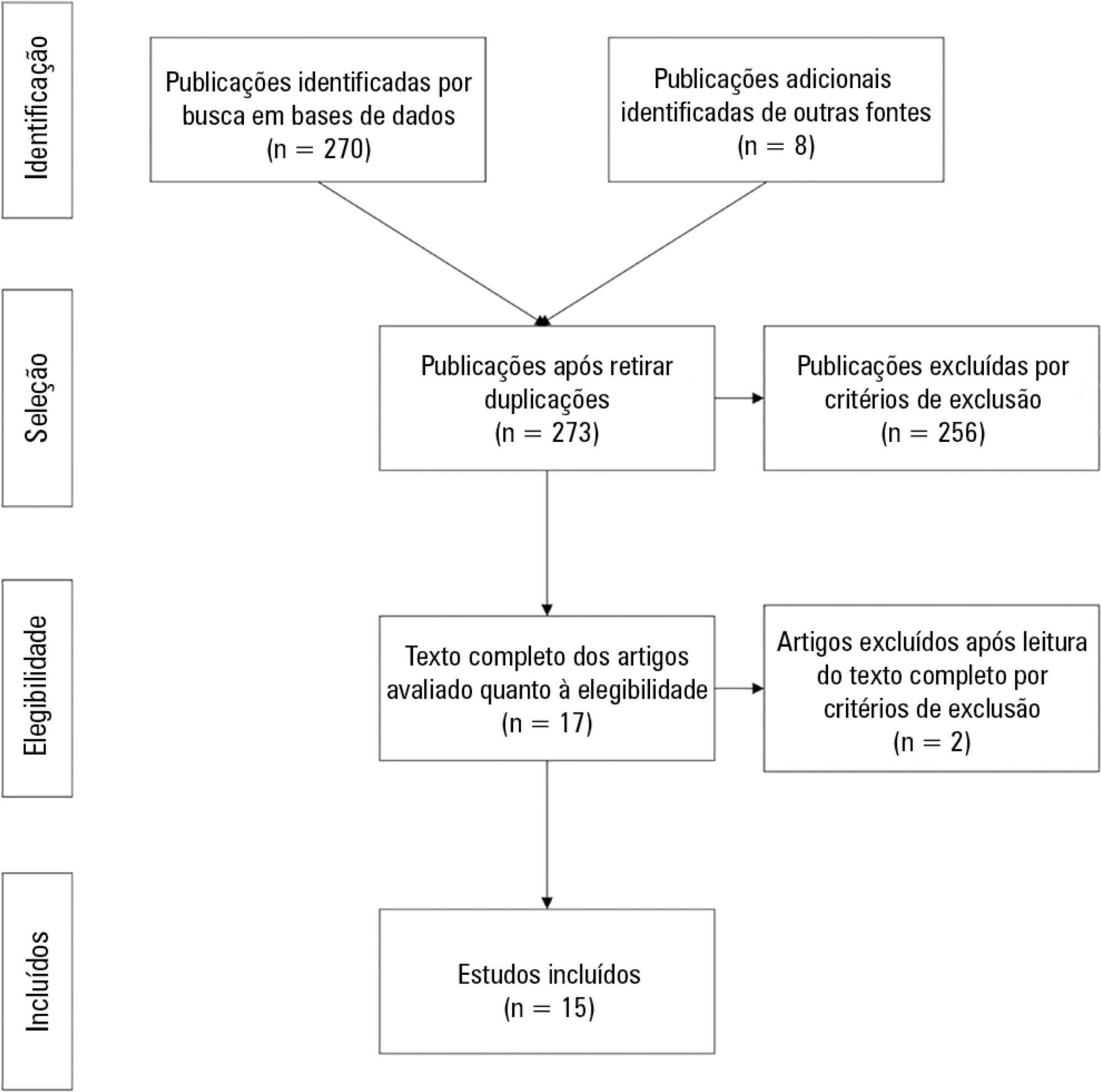
The MEDLINE, LILACS, Cochrane Library, Center for Reviews and Dissemination databases were searched.
We included studies that evaluated the effectiveness of rapid response teams in adult hospital units, published in English, Portuguese, or Spanish, from 2000 to 2016; systematic reviews, clinical trials, cohort studies, and prepost ecological studies were eligible for inclusion. The quality of studies was independently assessed by two researchers using the Newcastle-Ottawa, modified Jadad, and Assessment of Multiple Systematic Reviews scales.
The results were synthesized and tabulated. When risk measures were reported by the authors of the included studies, we estimated effectiveness as 1-RR or 1-OR. In pre-post studies, we estimated effectiveness as the percent decrease in rates following the intervention.
Overall, 278 studies were identified, 256 of which were excluded after abstract evaluation, and two of which were excluded after full text evaluation. In the meta-analysis of the studies reporting mortality data, we calculated a risk ratio of 0.85 (95%CI 0.76 - 0.94); and for studies reporting cardiac arrest data the estimated risk ratio was 0.65 (95%CI 0.49 - 0.87). Evidence was assessed as low quality due to the high heterogeneity and risk of bias in primary studies.
We conclude that rapid response teams may reduce in-hospital mortality and cardiac arrests, although the quality of evidence for both outcomes is low.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):444-452
DOI 10.5935/0103-507X.20170061
To describe the epidemiology of acute kidney injury, its relationship to chronic kidney disease, and the factors associated with its incidence.
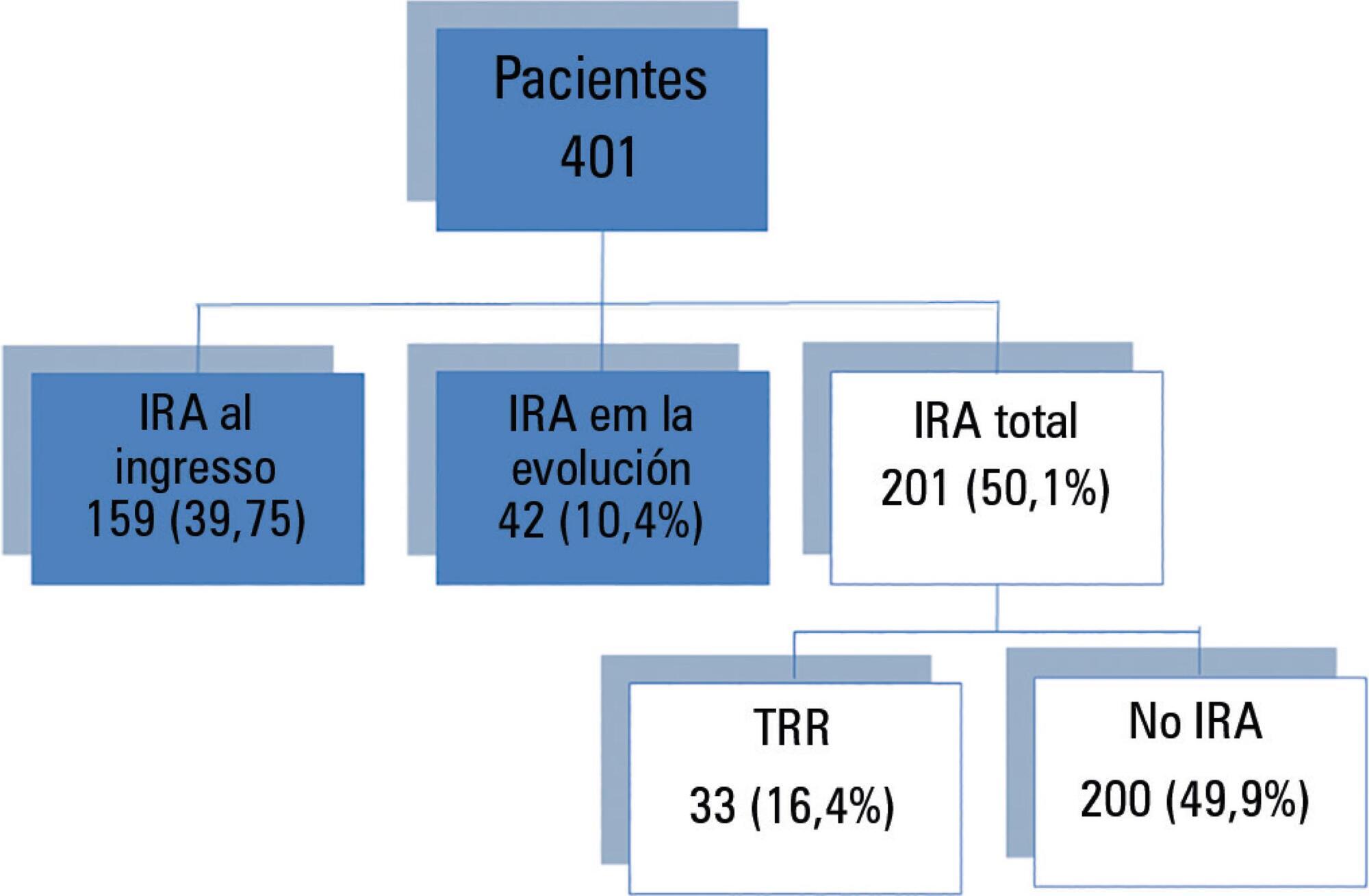
A cohort study and follow-up were conducted in an intensive care unit in Montevideo, Uruguay. We included patients admitted between November 2014 and October 2015 who were older than 15 years of age and who had at least two measurements of serum creatinine. We excluded patients who were hospitalized for less than 48 hours, patients who died at the time of hospitalization, and patients with chronic renal disease who were on hemodialysis or peritoneal dialysis. There were no interventions. Acute kidney injury was defined according to the criteria set forth in Acute Kidney Injury Disease: Improving Global Outcomes, and chronic kidney disease was defined according to the Chronic Kidney Disease Work Group.
We included 401 patients, 56.6% male, median age of 68 years (interquartile range (IQR) 51-79 years). The diagnosis at admission was severe sepsis 36.3%, neurocritical 16.3%, polytrauma 15.2%, and other 32.2%. The incidence of acute kidney injury was 50.1%, and 14.1% of the patients suffered from chronic kidney disease. The incidence of acute septic kidney injury was 75.3%. Mortality in patients with or without acute kidney injury was 41.8% and 14%, respectively (p < 0.001). In the multivariate analysis, the most significant variables for acute kidney injury were chronic kidney disease (odds ratio (OR) 5.39, 95%CI 2.04 - 14.29, p = 0.001), shock (OR 3.94, 95%CI 1.72 - 9.07, p = 0.001), and severe sepsis (OR 7.79, 95%CI 2.02 - 29.97, p = 0.003).
The incidence of acute kidney injury is high mainly in septic patients. Chronic kidney disease was independently associated with the development of acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):317-324
DOI 10.5935/0103-507X.20170047
This study intended to determine whether the systemic inflammatory response syndrome criteria can predict hospital mortality in a Brazilian cohort of critically ill patients.
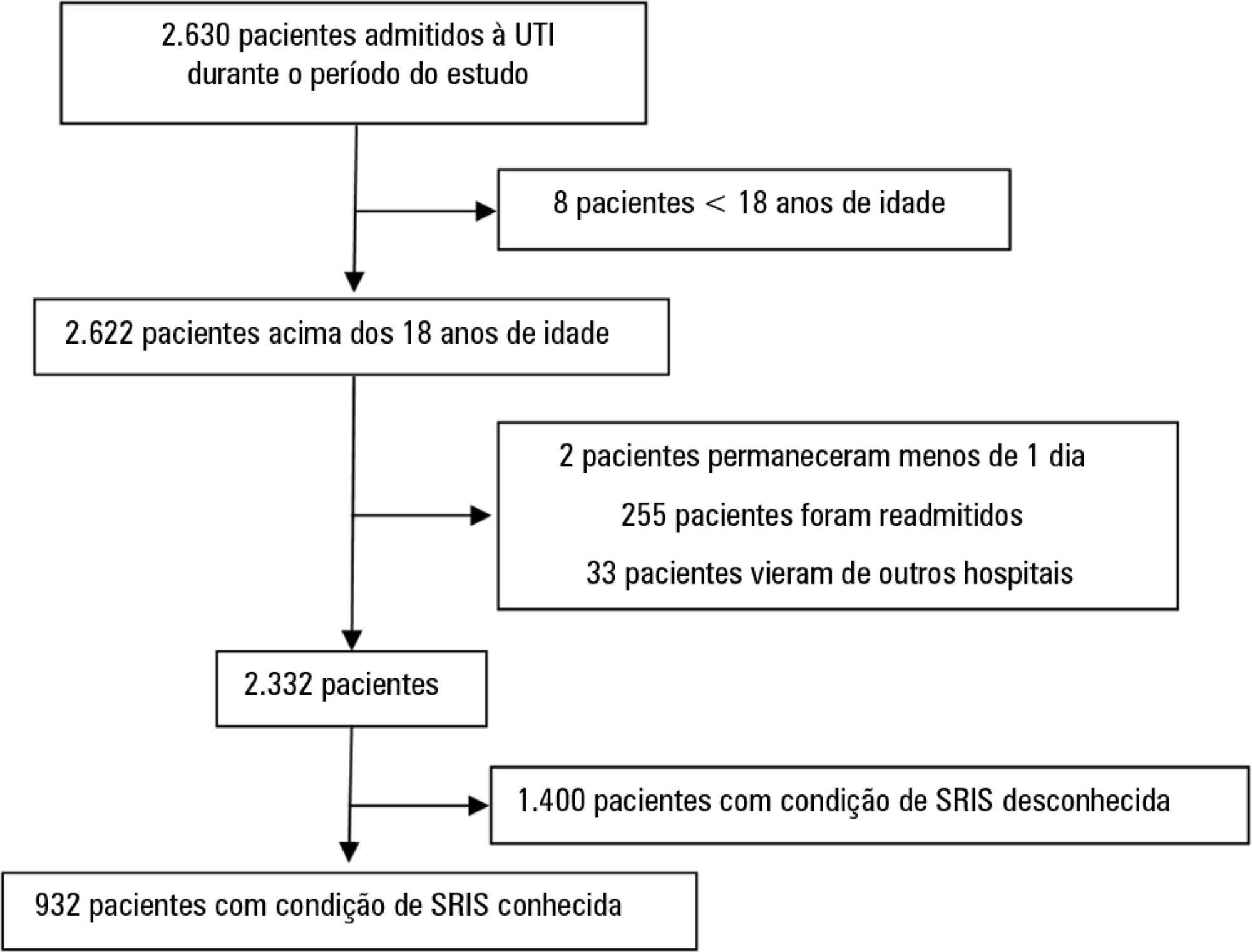
We performed a retrospective cohort study at a private tertiary hospital in São Paulo (SP), Brazil. We extracted information from the adult intensive care unit database (Sistema EpimedTM). We compared the SAPS 3 and the systemic inflammatory response syndrome model as dichotomous (≥ 2 criteria: systemic inflammatory response syndrome -positive versus 0 - 1 criterion: systemic inflammatory response syndrome -negative) and ordinal variables from 0 to 4 (according to the number of systemic inflammatory response syndrome criteria met) in the prediction of hospital mortality at intensive care unit admission. Model discrimination was compared using the area under the receiver operating characteristics (AUROC) curve.
From January to December 2012, we studied 932 patients (60.4% were systemic inflammatory response syndrome -positive). systemic inflammatory response syndrome -positive patients were more critically ill than systemic inflammatory response syndrome -negative patients and had higher hospital mortality (16.9% versus 8.1%, p < 0.001). In the adjusted analysis, being systemic inflammatory response syndrome -positive independently increased the risk of death by 82% (odds ratio 1.82; 95% confidence interval [CI] 1.12 - 2.96, p = 0.016). However, the AUROC curve for the SAPS 3 model was higher (0.81, 95%CI 0.78 - 0.85) compared to the systemic inflammatory response syndrome model with the systemic inflammatory response syndrome criteria as a dichotomous variable (0.60, 95%CI 0.55 - 0.65) and as an ordinal variable (0.62, 95%CI 0.57 - 0.68; p < 0.001) for hospital mortality.
Although systemic inflammatory response syndrome is associated with hospital mortality, the systemic inflammatory response syndrome criteria show low accuracy in the prediction of mortality compared with the SAPS 3.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):180-187
DOI 10.5935/0103-507X.20170028
To analyze patients after cardiac surgery that needed endotracheal reintubation and identify factors associated with death and its relation with the severity scores.
Retrospective analysis of information of 1,640 patients in the postoperative period of cardiac surgery between 2007 and 2015.
The reintubation rate was 7.26%. Of those who were reintubated, 36 (30.3%) underwent coronary artery bypass surgery, 27 (22.7%) underwent valve replacement, 25 (21.0%) underwent correction of an aneurysm, and 8 (6.7%) underwent a heart transplant. Among those with comorbidities, 54 (51.9%) were hypertensive, 22 (21.2%) were diabetic, and 10 (9.6%) had lung diseases. Among those who had complications, 61 (52.6%) had pneumonia, 50 (42.4%) developed renal failure, and 49 (51.0%) had a moderate form of the transient disturbance of gas exchange. Noninvasive ventilation was performed in 53 (44.5%) patients. The death rate was 40.3%, and mortality was higher in the group that did not receive noninvasive ventilation before reintubation (53.5%). Within the reintubated patients who died, the SOFA and APACHE II values were 7.9 ± 3.0 and 16.9 ± 4.5, respectively. Most of the reintubated patients (47.5%) belonged to the high-risk group, EuroSCORE (> 6 points).
The reintubation rate was high, and it was related to worse SOFA, APACHE II and EuroSCORE scores. Mortality was higher in the group that did not receive noninvasive ventilation before reintubation.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):337-345
DOI 10.5935/0103-507X.20170058
To establish the prevalence of delirium in a general intensive care unit and to identify associated factors, clinical expression and the influence on outcomes.
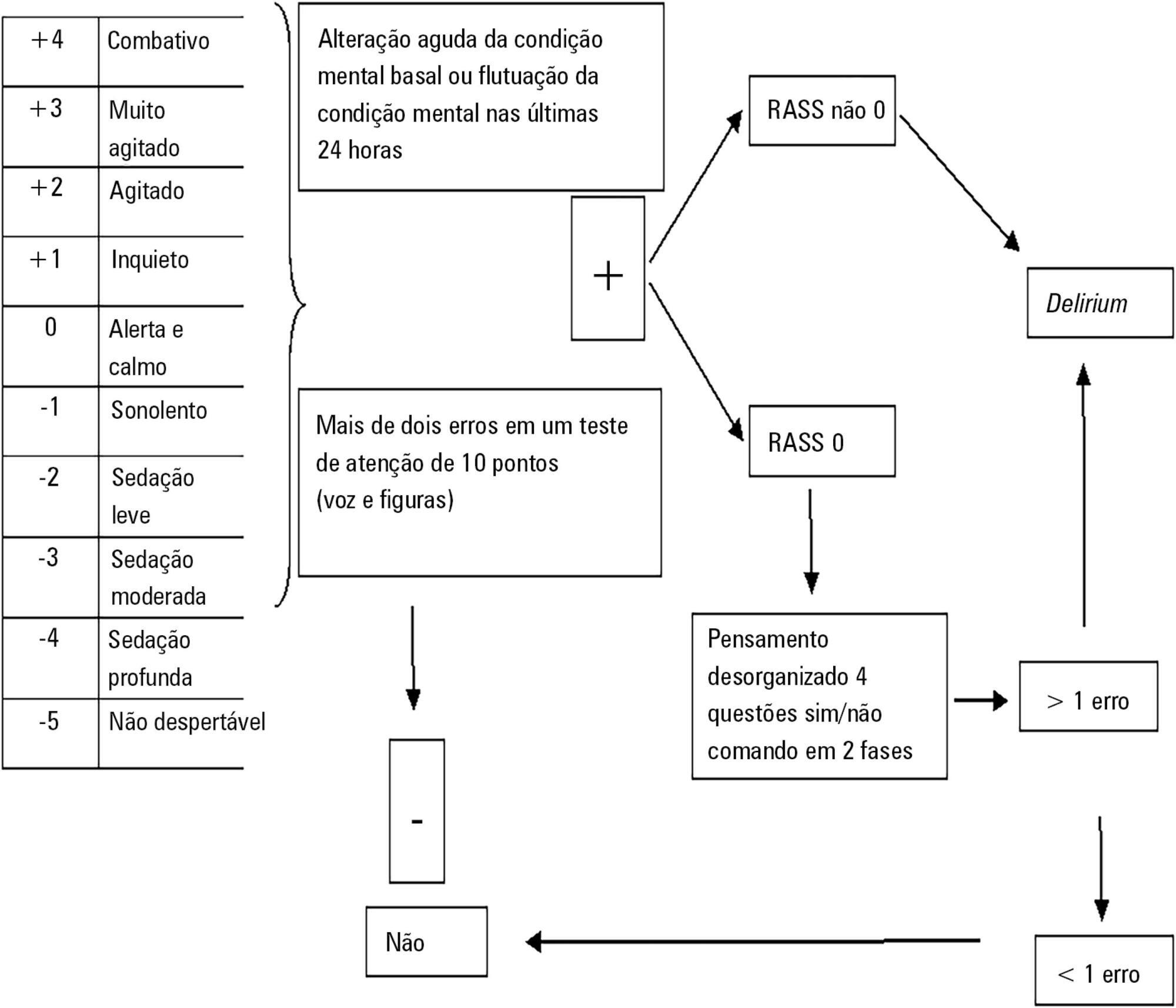
This was a prospective cohort study in a medical surgical intensive care unit. The Richmond Agitation-Sedation Scale and Confusion Assessment Method for the Intensive Care Unit were used daily to identify delirium in mechanically ventilated patients.
In this series, delirium prevalence was 80% (N = 184 delirious patients out of 230 patients). The number of patients according to delirium psychomotor subtypes was as follows: 11 hyperactive patients (6%), 9 hypoactive patients (5%) and 160 mixed patients (89%). Multiple logistic regression modeling using delirium as the dependent outcome variable (to study the risk factors for delirium) revealed that age > 65 years, history of alcohol consumption, and number of mechanical ventilation days were independent variables associated with the development of delirium. The multiple logistic regression model using hospital mortality as the dependent outcome variable (to study the risk factors for death) showed that severity of illness, according to the Acute Physiology and Chronic Health Evaluation II, mechanical ventilation for more than 7 days, and sedation days were all independent predictors for excess hospital mortality.
This Latin American prospective cohort investigation confirmed specific factors important for the development of delirium and the outcome of death among general intensive care unit patients. In both analyses, we found that the duration of mechanical ventilation was a predictor of untoward outcomes.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):364-372
DOI 10.5935/0103-507X.20170054
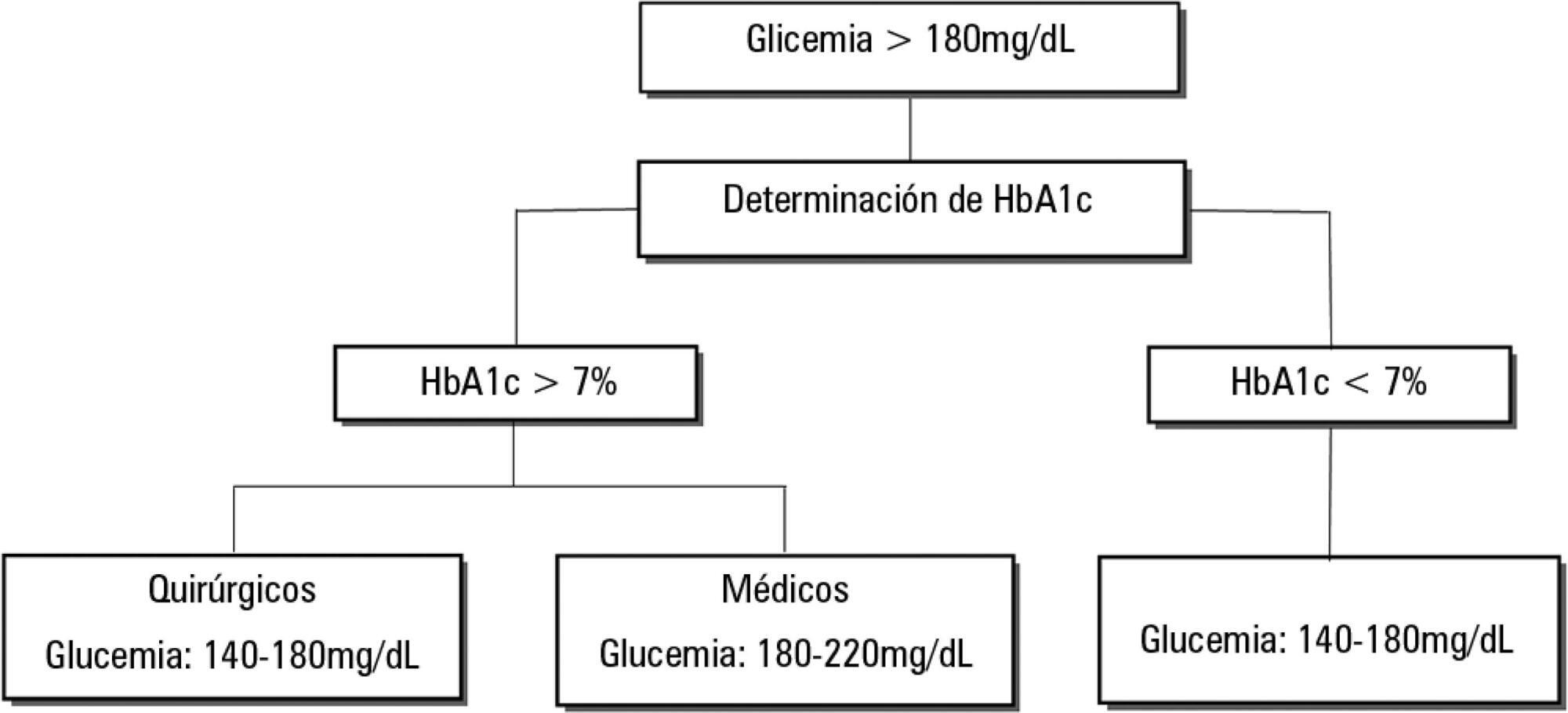
Dysglycemia in critically ill patients (hyperglycemia, hypoglycemia, glycemic variability and time in range) is a biomarker of disease severity and is associated with higher mortality. However, this impact appears to be weakened in patients with previous diabetes mellitus, particularly in those with poor premorbid glycemic control; this phenomenon has been called "diabetes paradox". This phenomenon determines that glycated hemoglobin (HbA1c) values should be considered in choosing glycemic control protocols on admission to an intensive care unit and that patients' target blood glucose ranges should be adjusted according to their HbA1c values. Therefore, HbA1c emerges as a simple tool that allows information that has therapeutic utility and prognostic value to be obtained in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2017;29(1):63-69
DOI 10.5935/0103-507X.20170010
To determine the impact of the day and time of admission and discharge from the intensive care unit on mortality.
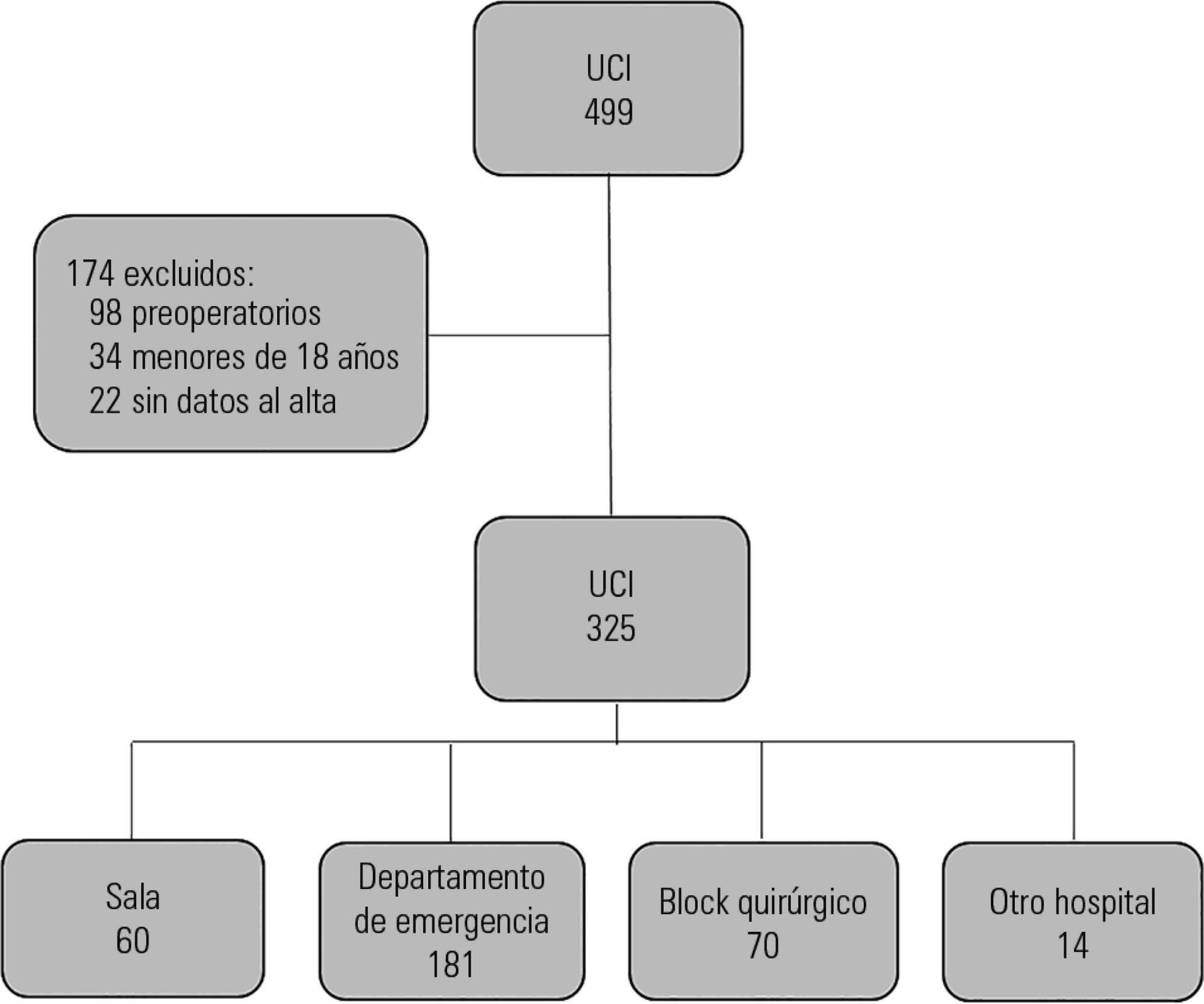
Prospective observational study that included patients admitted to the intensive care unit of the Hospital Maciel in Montevideo between April and November 2014.
We analyzed 325 patients with an average age of 55 (36 - 71) years and a SAPS II value of 43 (29 - 58) points. No differences were found in the mortality of patients in the intensive care unit when time of admission (35% on the weekend versus 31% on weekdays, p = ns) or the hour of entry (35% at night versus 31% in the daytime, p = ns) were compared. The time of discharge was associated with higher hospital mortality rates (57% for weekend discharges versus 14% for weekday discharges, p = 0.000). The factors independently associated with hospital mortality after discharge from the intensive care unit were age > 50 years (OR 2.4, 95%CI, 1.1 - 5.4) and weekend discharge (OR 7.7, 95%CI, 3.8-15.6).
This study identified the time of discharge from the intensive care unit as a factor that was independently associated with hospital mortality.