Abstract
Crit Care Sci. 2024;36:e20240144en
DOI 10.62675/2965-2774.20240144-pt
To determine whether enteral melatonin decreases the incidence of delirium in critically ill adults.
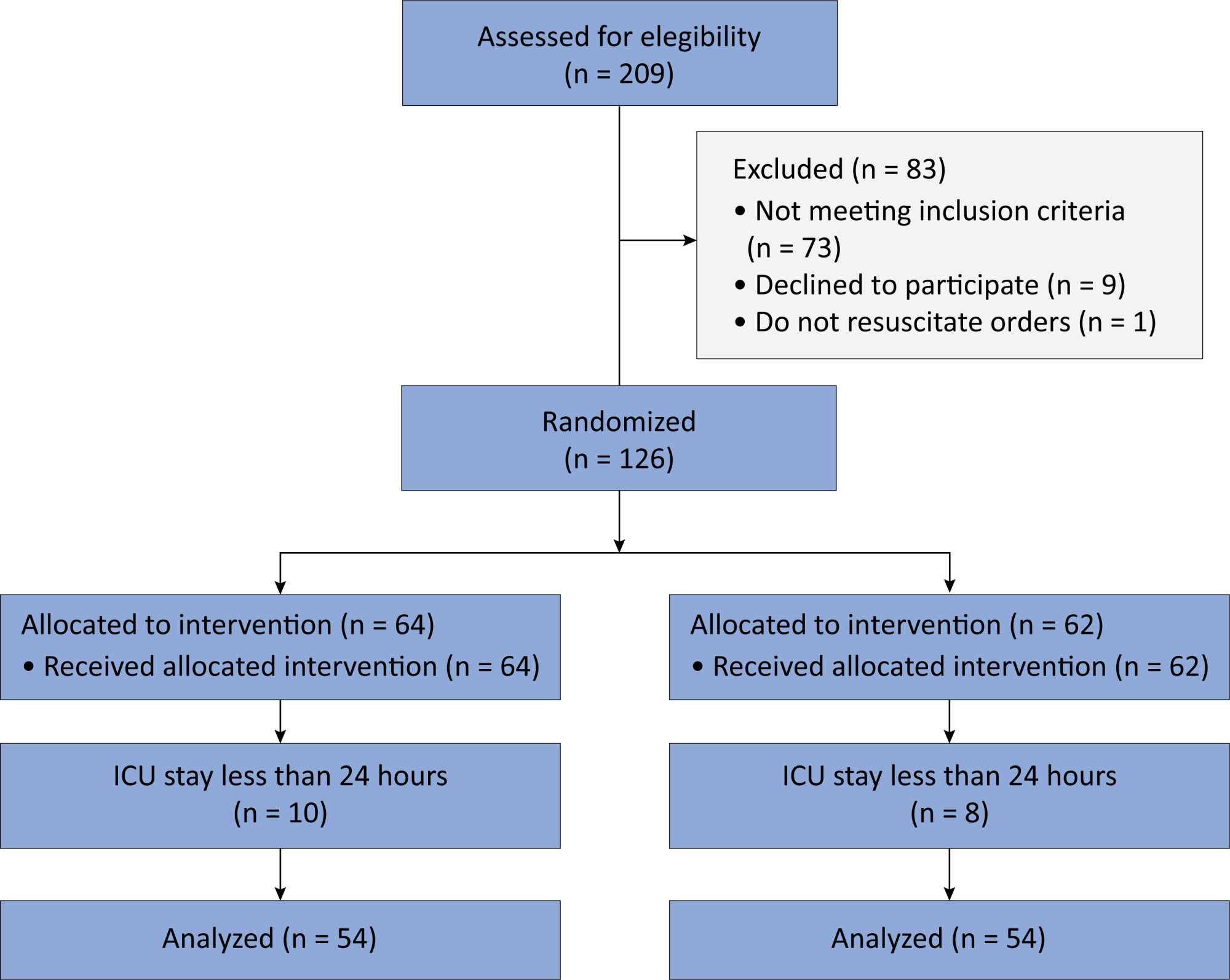
In this randomized controlled trial, adults were admitted to the intensive care unit and received either usual standard care alone (Control Group) or in combination with 3mg of enteral melatonin once a day at 9 PM (Melatonin Group). Concealment of allocation was done by serially numbered opaque sealed envelopes. The intensivist assessing delirium and the investigator performing the data analysis were blinded to the group allocation. The primary outcome was the incidence of delirium within 24 hours of the intensive care unit stay. The secondary outcomes were the incidence of delirium on Days 3 and 7, intensive care unit mortality, length of intensive care unit stay, duration of mechanical ventilation and Glasgow outcome score (at discharge).
We included 108 patients in the final analysis, with 54 patients in each group. At 24 hours of intensive care unit stay, there was no difference in the incidence of delirium between Melatonin and Control Groups (29.6 versus 46.2%; RR = 0.6; 95%CI 0.38 - 1.05; p = 0.11). No secondary outcome showed a statistically significant difference.
Enteral melatonin 3mg is not more effective at decreasing the incidence of delirium than standard care is in critically ill adults.
Abstract
Crit Care Sci. 2023;35(3):320-327
DOI 10.5935/2965-2774.20230165-pt
To translate and cross-culturally adapt the Cornell Assessment of Pediatric Delirium anchor points from English to Brazilian Portuguese.
For the translation and cross-cultural adaptation of the anchor points, all steps recommended internationally were followed after authorization for use by the lead author. The stages were as follows: translation of the original version into Portuguese by two bilingual translators who were native speakers of the target language, synthesis of the versions, reverse translation by two translators who were native speakers of the source language, review and synthesis of the back-translation, review by a committee of experts and preparation of the final version.
The translation and cross-cultural adaptation of the anchor points was conducted in accordance with recommendations. The linguistic and semantic issues that arose were discussed by a committee of judges, with 91.8% agreement, as determined using a Likert scale, after changes by consensus. After reanalysis by the authors, there were no changes, resulting in the final version, which was easy to understand and administer.
The translation and cross-cultural adaptation of the anchor points of the Cornell Assessment of Pediatric Delirium scale into Portuguese spoken in Brazil were successful, maintaining the linguistic and semantic properties of the original instrument. The table of anchor points is easy to understand and will be helpful during the assessment of children younger than 24 months using the Cornell Assessment of Pediatric Delirium scale.
Abstract
Crit Care Sci. 2023;35(2):147-155
DOI 10.5935/2965-2774.20230422-pt
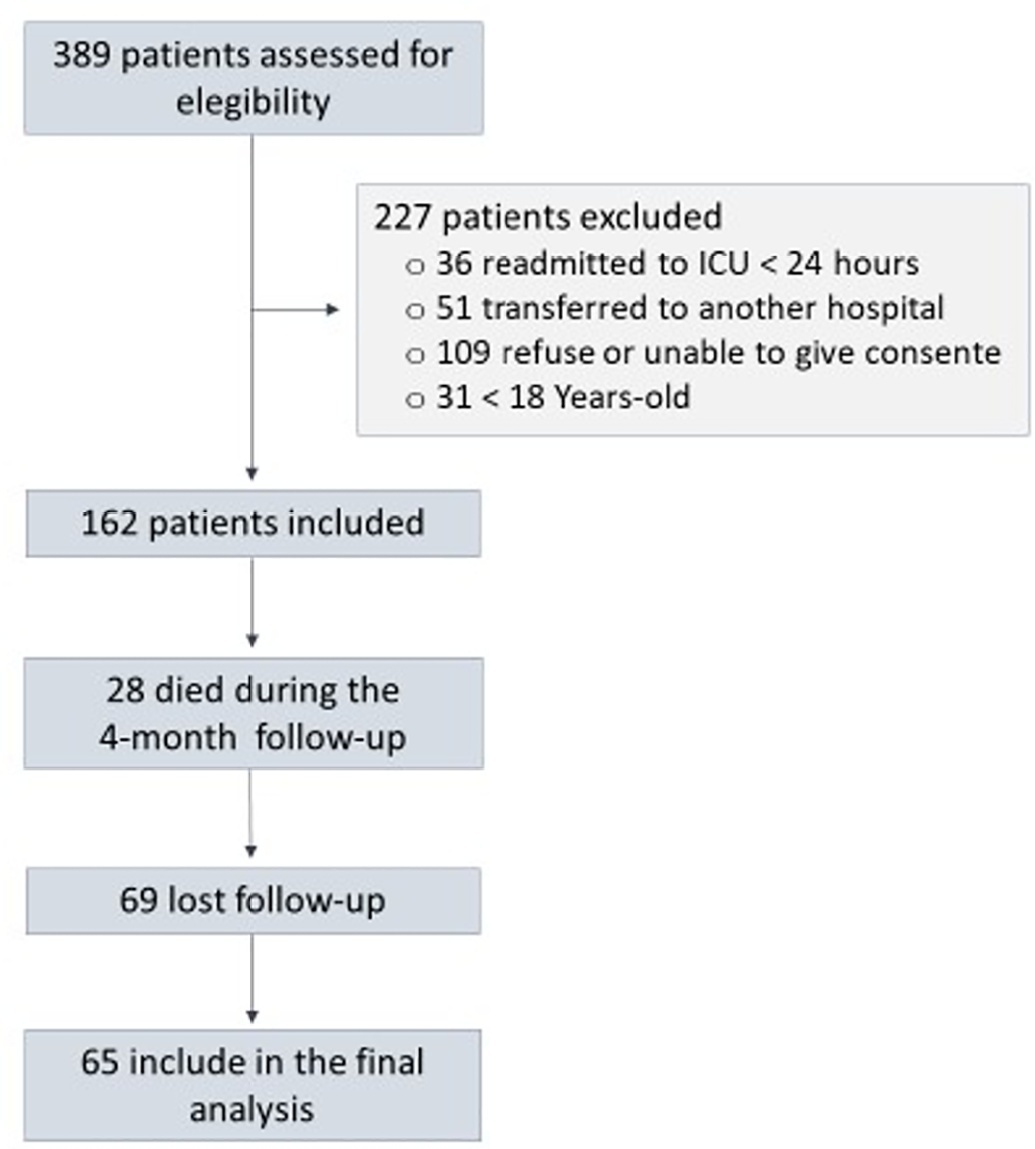
To assess factors associated with long-term neuropsychiatric outcomes, including biomarkers measured after discharge from the intensive care unit.
A prospective cohort study was performed with 65 intensive care unit survivors. The cognitive evaluation was performed through the Mini-Mental State Examination, the symptoms of anxiety and depression were evaluated using the Hospital Anxiety and Depression Scale, and posttraumatic stress disorder was evaluated using the Impact of Event Scale-6. Plasma levels of amyloid-beta (1-42) [Aβ (1-42)], Aβ (1-40), interleukin (IL)-10, IL-6, IL-33, IL-4, IL-5, tumor necrosis factor alpha, C-reactive protein, and brain-derived neurotrophic factor were measured at intensive care unit discharge.
Of the variables associated with intensive care, only delirium was independently related to the occurrence of long-term cognitive impairment. In addition, higher levels of IL-10 and IL-6 were associated with cognitive dysfunction. Only IL-6 was independently associated with depression. Mechanical ventilation, IL-33 levels, and C-reactive protein levels were independently associated with anxiety. No variables were independently associated with posttraumatic stress disorder.
Cognitive dysfunction, as well as symptoms of depression, anxiety, and posttraumatic stress disorder, are present in patients who survive a critical illness, and some of these outcomes are associated with the levels of inflammatory biomarkers measured at discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):227-236
DOI 10.5935/0103-507X.20220020-en
To establish current Portuguese critical care practices regarding analgesia, sedation, and delirium based on a comparison between the activities reported and daily clinical practice.
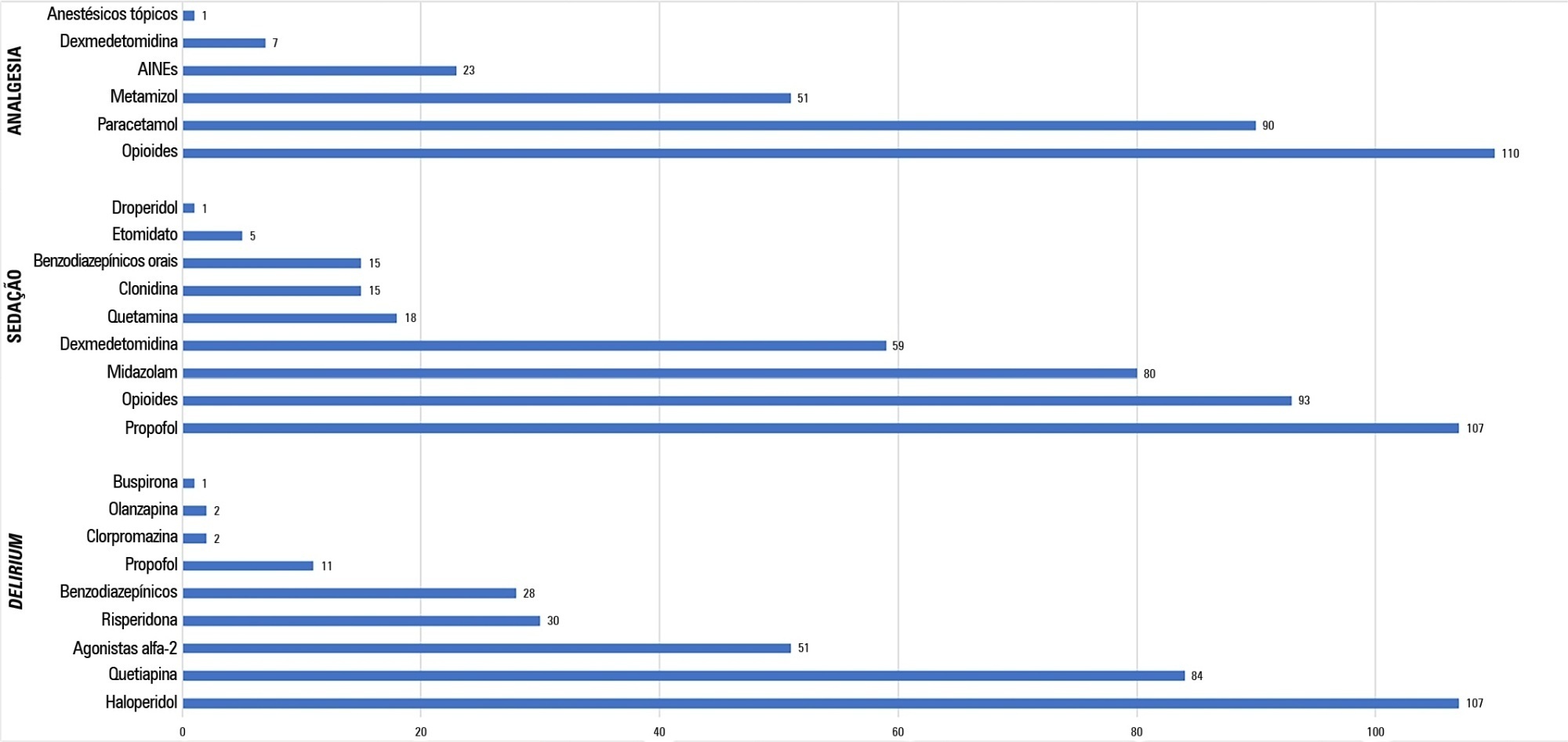
A national survey was conducted among physicians invited to report their practice toward analgesia, sedation, and delirium in intensive care units. A point prevalence study was performed to analyze daily practices.
A total of 117 physicians answered the survey, and 192 patients were included in the point prevalence study. Survey and point prevalence studies reflect a high sedation assessment (92%; 88.5%), with the Richmond Agitated Sedation Scale being the most reported and used scale (41.7%; 58.2%) and propofol being the most reported and used medication (91.4%; 58.6%). Midazolam prescribing was reported by 68.4% of responders, but a point prevalence study revealed a use of 27.6%.
The results from the survey did not accurately reflect the common practices in Portuguese intensive care units, as reported in the point prevalence study. Efforts should be made specifically to avoid oversedation and to promote delirium assessment.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):426-432
DOI 10.5935/0103-507X.20200072
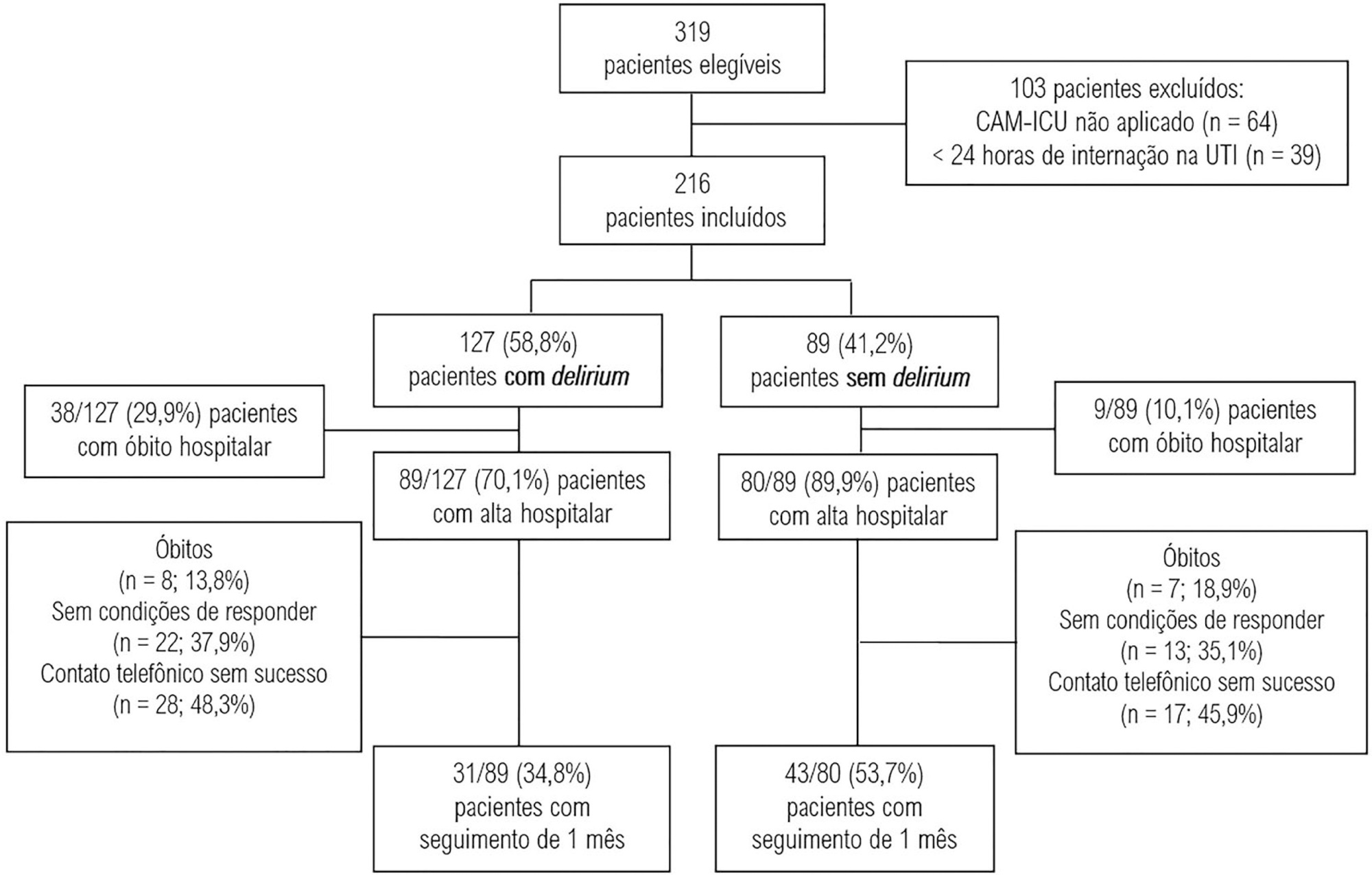
To evaluate the association between the incidence of delirium in the intensive care unit and quality of life 1 month after hospital discharge.
This was a prospective cohort study conducted in the intensive care units of two medium-complexity hospitals from December 2015 to December 2016. Delirium was identified using the Confusion Assessment Method for the Intensive Care Unit scale. At the time of hospital discharge, functional capacity and cognition were assessed with the Barthel index and the Mini Mental State Examination, respectively. Thirty days after patient discharge, the World Health Organization Quality of Life-BREF questionnaire was administered by telephone.
A total of 216 patients were included. Delirium was identified in 127 (58.8%) of them. Patients with delirium exhibited greater functional dependence (median Barthel index 50.0 [21.2 - 70.0] versus 80.0 [60.0 - 95.0]; p < 0.001) and lower cognition (Mini Mental State Examination score 12.9 ± 7.5 versus 20.7 ± 9.8; p < 0.001) at hospital discharge. There was no difference in any of the quality-of-life domains evaluated 1 month after hospital discharge between patients with and without delirium.
Our findings suggest that patients with delirium in the intensive care unit do not have worse quality of life 1 month after hospital discharge, despite presenting greater cognitive impairment and functional disability at the time of hospital discharge.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):268-276
DOI 10.5935/0103-507X.20200043
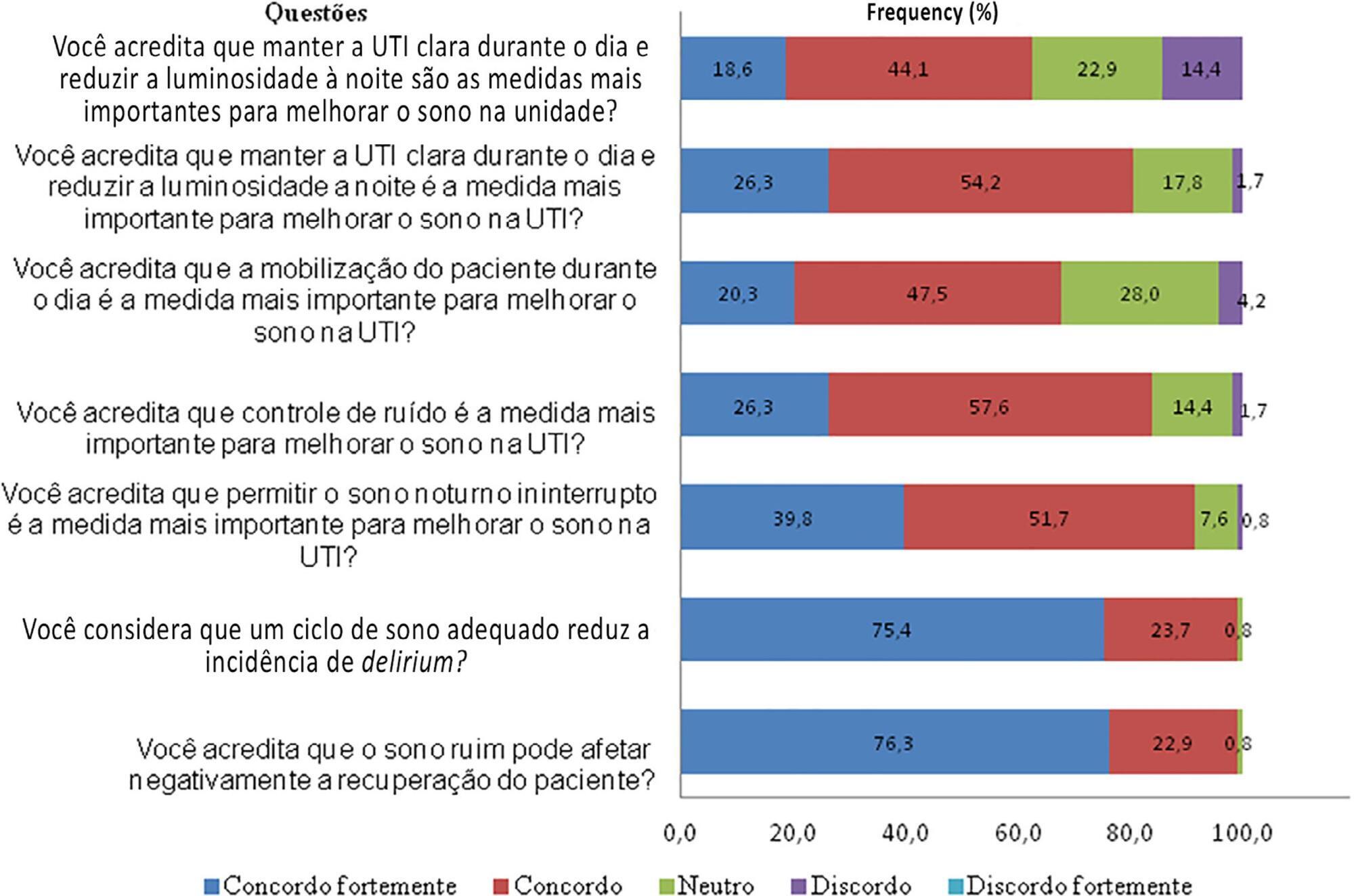
To conduct a national survey of intensive care professionals to identify the practices for promoting sleep in adult intensive care units in Brazil and describe the professionals’ perceptions of the importance of sleep for patients.
An electronic questionnaire was distributed by the clinical research cooperation network of the Associação de Medicina Intensiva Brasileira and by the Brazilian Research in Intensive Care Network to physicians and nurses registered with the association. The questionnaire evaluated the profile of the respondents, the profile of their intensive care units, whether protocols for promoting sleep were present, the pharmacological and nonpharmacological measures typically employed in the unit, and the professionals’ perceptions regarding sleep in critically ill patients.
A total of 118 questionnaires were evaluated. The Southeast region of the country was the most represented (50 questionnaires, 42.4%). The majority of units had a clinical-surgical profile (93 questionnaires; 78.8%), and 26 had a continuous visitation policy (22.0%). Only 18 intensive care units (15.3%) reported having protocols for promoting sleep. The most cited measure for sleep promotion was reducing light during the night (95 questionnaires; 80.5%), which was more often performed in private intensive care units. Almost all of the responders (99%) believed that poor-quality sleep has a negative impact on patient recovery.
The responses to this Brazilian survey revealed that few intensive care units had a program for promoting sleep, although almost all participants recognized the importance of sleep in patient recovery.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):466-475
DOI 10.5935/0103-507X.20170063
This paper sought to determine the accumulated incidence and analyze the risk factors associated with the development of weakness acquired in the intensive care unit and its relationship to inspiratory weakness.
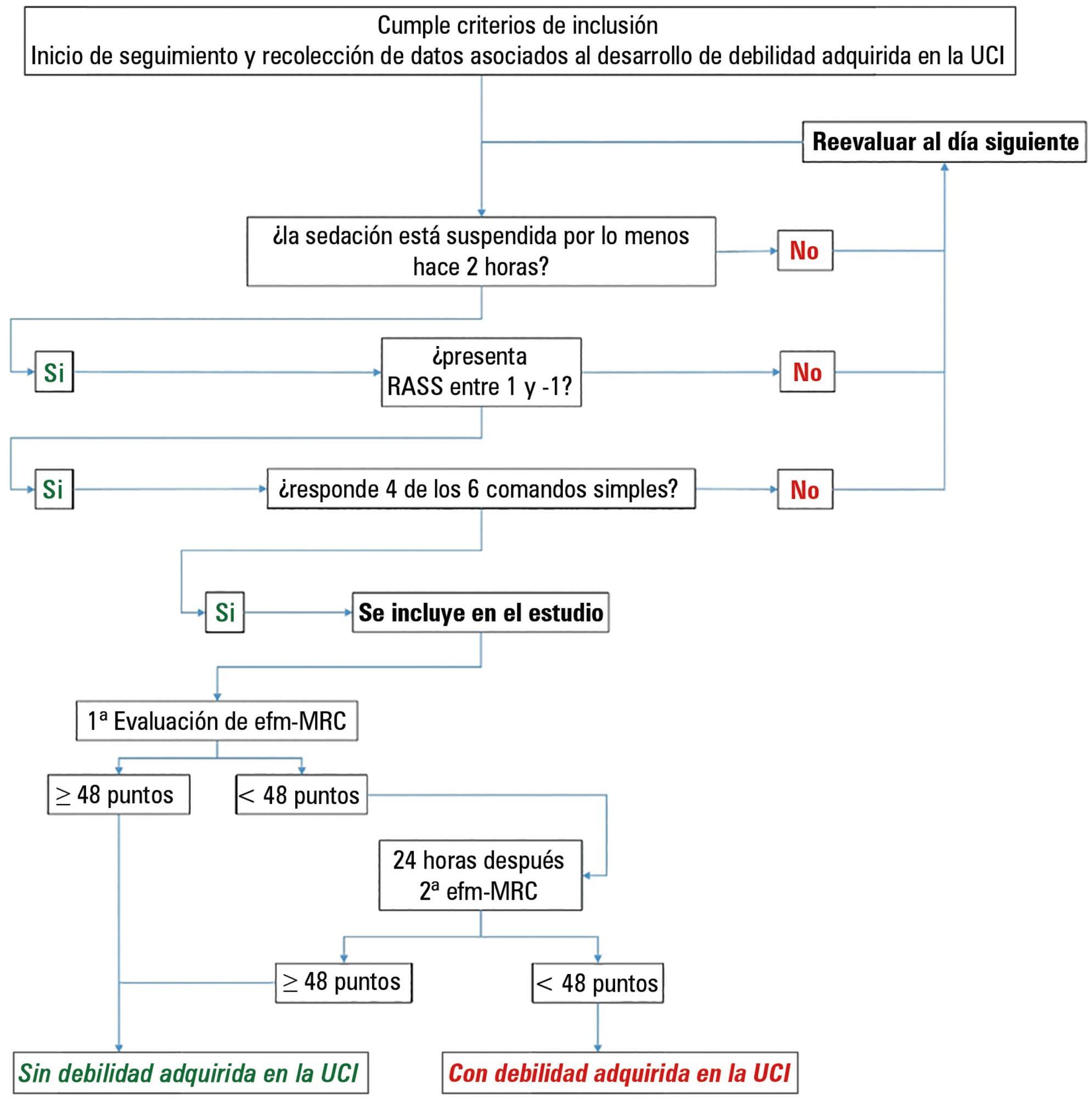
We conducted a prospective cohort study at a single center, multipurpose medical-surgical intensive care unit. We included adult patients who required mechanical ventilation ≥ 24 hours between July 2014 and January 2016. No interventions were performed. Demographic data, clinical diagnoses, the factors related to the development of intensive care unit -acquired weakness, and maximal inspiratory pressure were recorded.
Of the 111 patients included, 66 developed intensive care unit -acquired weakness, with a cumulative incidence of 40.5% over 18 months. The group with intensive care unit-acquired weakness were older (55.9 ± 17.6 versus 45.8 ± 16.7), required more mechanical ventilation (7 [4 - 10] days versus 4 [2 - 7.3] days), and spent more time in the intensive care unit (15.5 [9.2 - 22.8] days versus 9 [6 - 14] days). More patients presented with delirium (68% versus 39%), hyperglycemia > 3 days (84% versus 59%), and positive balance > 3 days (73.3% versus 37%). All comparisons were significant at p < 0.05. A multiple logistic regression identified age, hyperglycemia ≥ 3 days, delirium, and mechanical ventilation > 5 days as independent predictors of intensive care unit-acquired weakness. Low maximal inspiratory pressure was associated with intensive care unit-acquired weakness (p < 0.001), and the maximum inspiratory pressure cut-off value of < 36cmH2O had sensitivity and specificity values of 31.8% and 95.5%, respectively, when classifying patients with intensive care unit-acquired weakness.
The intensive care unit acquired weakness is a condition with a high incidence in our environment. The development of intensive care unit-acquired weakness was associated with age, delirium, hyperglycemia, and mechanical ventilation > 5 days. The maximum inspiratory pressure value of ≥ 36cmH2O was associated with a high diagnostic value to exclude the presence of intensive care unit -acquired weakness.