Abstract
Revista Brasileira de Terapia Intensiva. 2021;33(2):231-242
DOI 10.5935/0103-507X.20210030
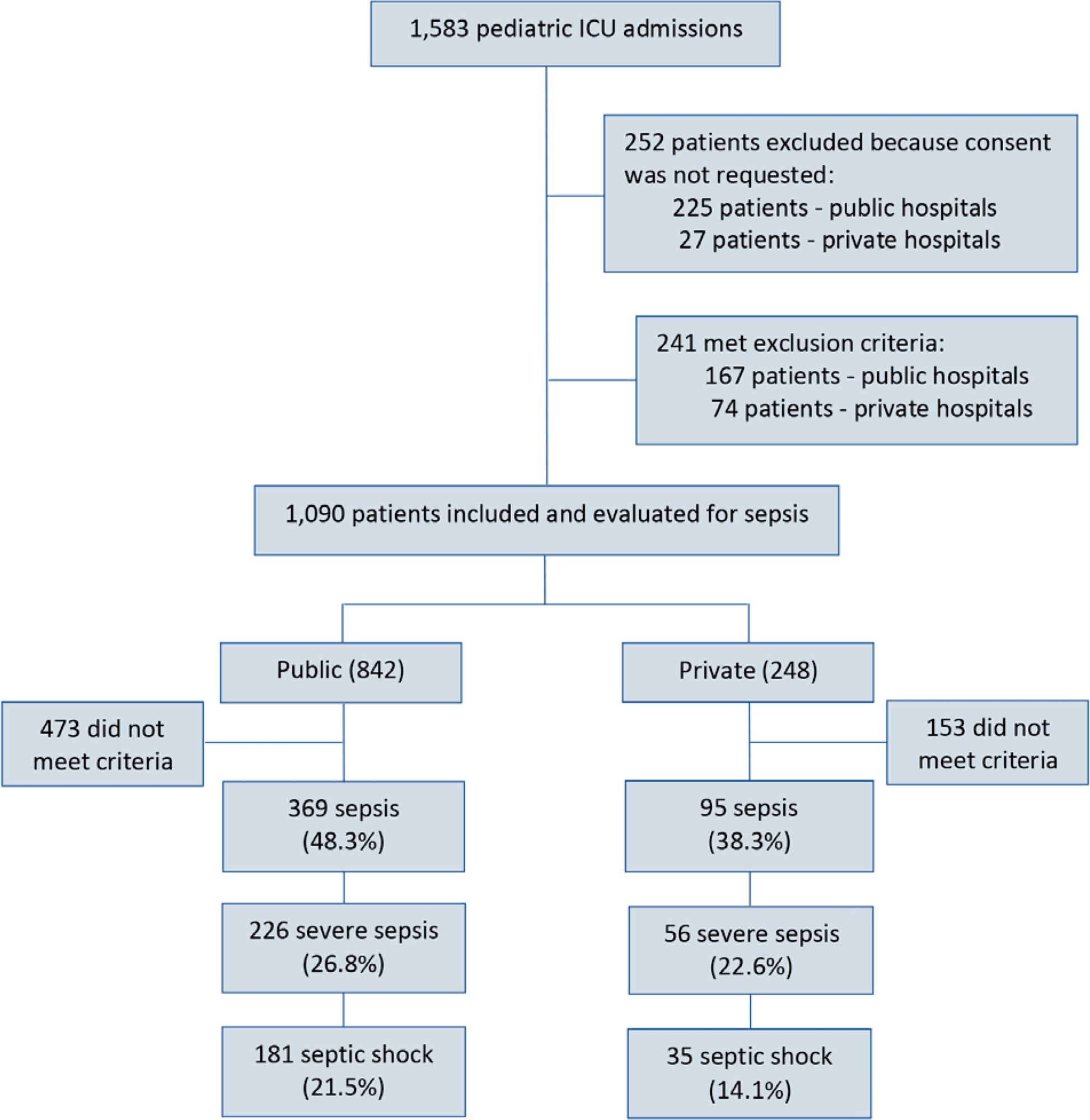
To report the prevalence and outcomes of sepsis in children admitted to public and private hospitals.
Post hoc analysis of the Latin American Pediatric Sepsis Study (LAPSES) data, a cohort study that analyzed the prevalence and outcomes of sepsis in critically ill children with sepsis on admission at 21 pediatric intensive care units in five Latin American countries.
Of the 464 sepsis patients, 369 (79.5%) were admitted to public hospitals and 95 (20.5%) to private hospitals. Compared to those admitted to private hospitals, sepsis patients admitted to public hospitals did not differ in age, sex, immunization status, hospital length of stay or type of admission but had higher rates of septic shock, higher Pediatric Risk of Mortality (PRISM), Pediatric Index of Mortality 2 (PIM 2), and Pediatric Logistic Organ Dysfunction (PELOD) scores, and higher rates of underlying diseases and maternal illiteracy. The proportion of patients admitted from pediatric wards and sepsis-related mortality were higher in public hospitals. Multivariate analysis did not show any correlation between mortality and the type of hospital, but mortality was associated with greater severity on pediatric intensive care unit admission in patients from public hospitals.
In this sample of critically ill children from five countries in Latin America, the prevalence of septic shock within the first 24 hours at admission and sepsis-related mortality were higher in public hospitals than in private hospitals. Higher sepsis-related mortality in children admitted to public pediatric intensive care units was associated with greater severity on pediatric intensive care unit admission but not with the type of hospital. New studies will be necessary to elucidate the causes of the higher prevalence and mortality of pediatric sepsis in public hospitals.
Abstract
Revista Brasileira de Terapia Intensiva. 2021;33(2):298-303
DOI 10.5935/0103-507X.20210038
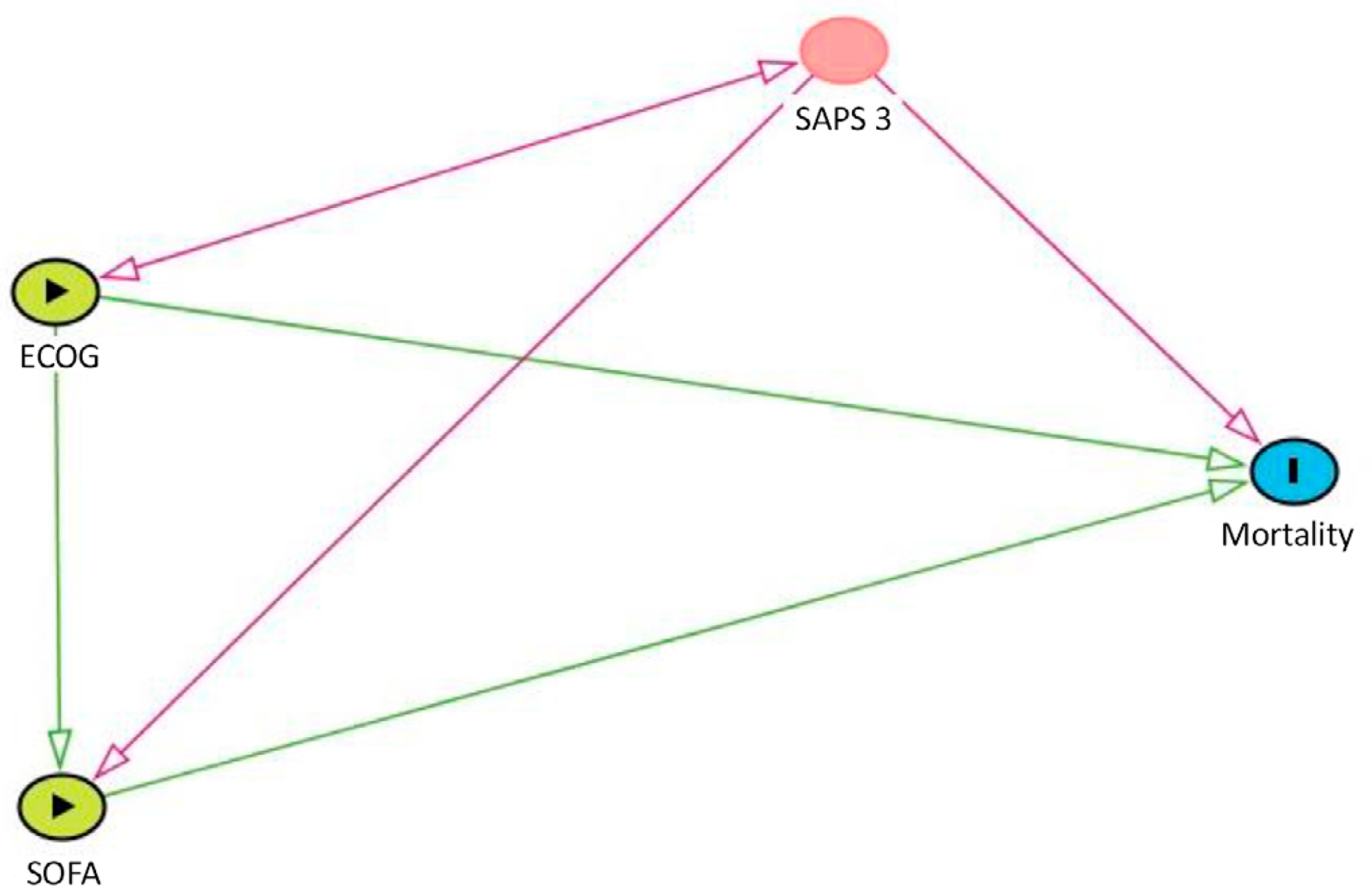
To evaluate how performance status impairment and acute organ dysfunction influence hospital mortality in critically ill patients with cancer who were admitted with suspected sepsis.
Data were obtained from a retrospective cohort of patients, admitted to an intensive care unit, with cancer and with a suspected infection who received parenteral antibiotics and underwent the collection of bodily fluid samples. We used logistic regression with hospital mortality as the outcome and the Sequential Organ Failure Assessment score, Eastern Cooperative Oncology Group status, and their interactions as predictors.
Of 450 patients included, 265 (58.9%) died in the hospital. For patients admitted to the intensive care unit with lower Sequential Organ Failure Assessment (≤ 6), performance status impairment influenced the in-hospital mortality, which was 32% among those with no and minor performance status impairment and 52% among those with moderate and severe performance status impairment, p < 0.01. However, for those with higher Sequential Organ Failure Assessment (> 6), performance status impairment did not influence the in-hospital mortality (73% among those with no and minor impairment and 84% among those with moderate and severe impairment; p = 0.1).
Performance status impairment seems to influence hospital mortality in critically ill cancer patients with suspected sepsis when they have less severe acute organ dysfunction at the time of intensive care unit admission.
Abstract
Revista Brasileira de Terapia Intensiva. 2020;32(1):49-57
DOI 10.5935/0103-507X.20200009
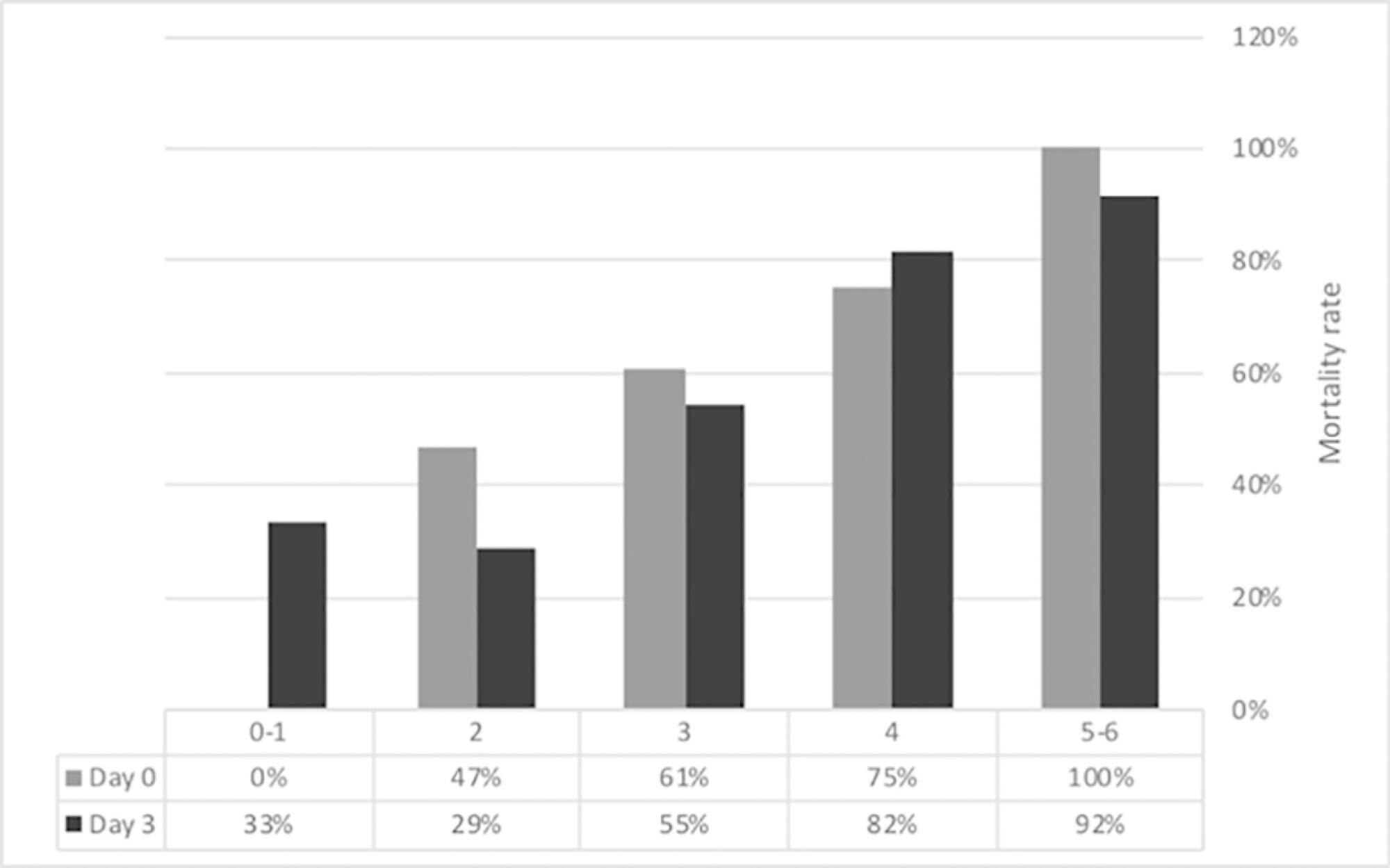
To characterize a cohort of acute-on-chronic liver failure patients in Intensive Care and to analyze the all-cause 28-day mortality risk factors assessed at ICU admission and day 3.
This was a retrospective cohort study of consecutive patients admitted to the intensive care unit between March 2013 and December 2016.
Seventy-one patients were included. The median age was 59 (51 - 64) years, and 81.7% of patients were male. Alcohol consumption alone (53.5%) was the most frequent etiology of cirrhosis and infection (53.5%) was the most common acute-on-chronic liver failure precipitating event. At intensive care unit admission, the clinical severity scores were APACHE II 21 (16 - 23), CLIF-SOFA 13 (11 - 15), Child-Pugh 12 (10 - 13) and MELD 27 (20 - 32). The acute-on-chronic liver failure scores were no-acute-on-chronic liver failure: 11.3%; one: 14.1%; two: 28.2% and three: 46.5%; and the number of organ failures was one: 4.2%; two: 42.3%; three: 32.4%; four: 16.9%; and five: 4.2%. Liver transplantation was performed in 15.5% of patients. The twenty-eight-day mortality rate was 56.3%, and the in-ICU mortality rate was 49.3%. Organ failure at intensive care unit admission (p = 0.02; OR 2.1; 95%CI 1.2 - 3.9), lactate concentration on day 3 (p = 0.02; OR 6.3; 95%CI 1.4 - 28.6) and the international normalized ratio on day 3 (p = 0.03; OR 10.2; 95%CI 1.3 - 82.8) were independent risk factors.
Acute-on-chronic liver failure patients presented with high clinical severity and mortality rates. The number of organ failures at intensive care unit admission and the lactate and international normalized ratio on day 3 were independent risk factors for 28-day mortality. We consider intensive care essential for acute-on-chronic liver failure patients and timely liver transplant was vital for selected patients.
Abstract
Revista Brasileira de Terapia Intensiva. 2020;32(1):37-42
DOI 10.5935/0103-507X.20200007
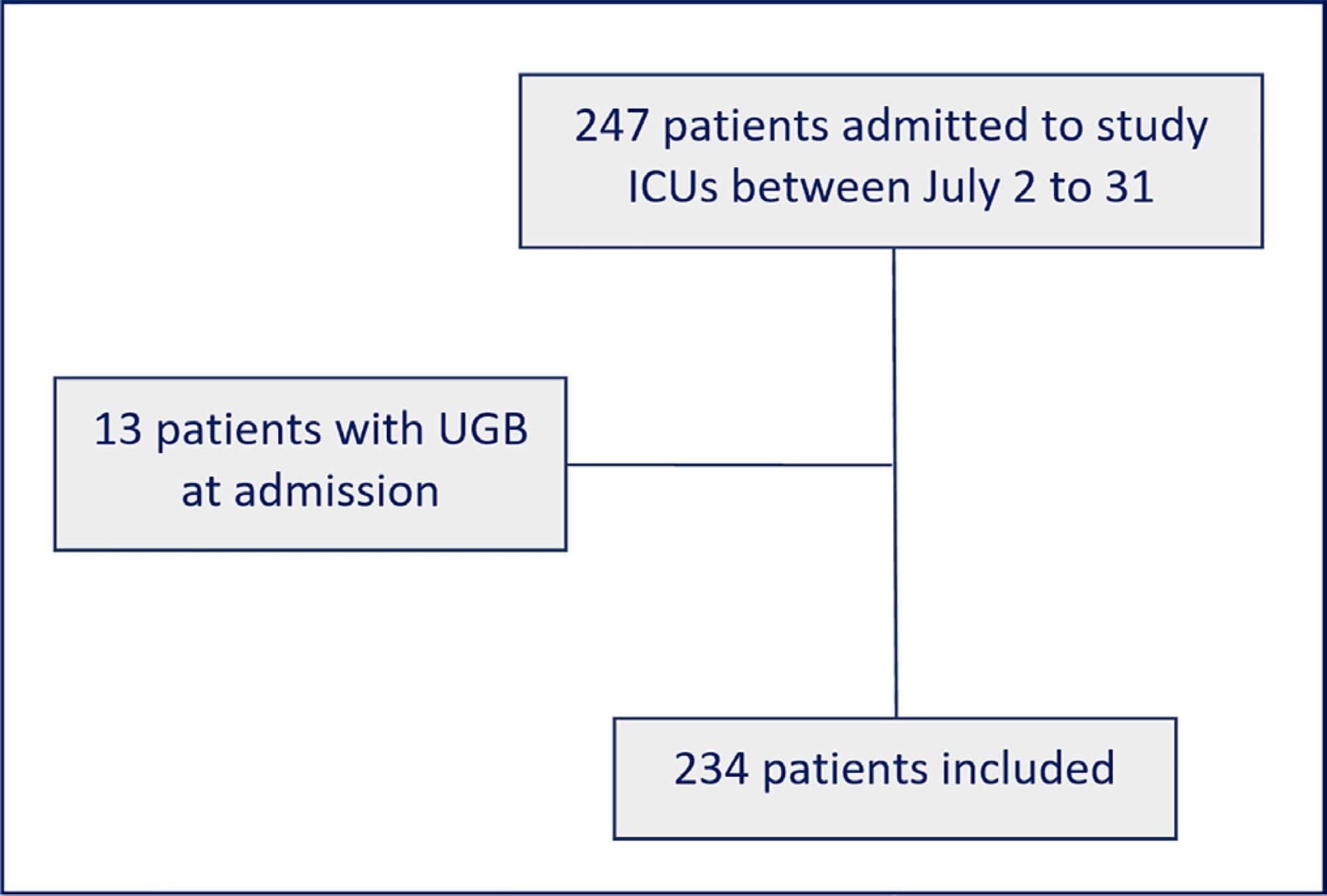
To evaluate adherence to the stress ulcer prophylaxis protocol in critically ill patients at a tertiary university hospital.
In this prospective cohort study, we included all adult patients admitted to the medical and surgical intensive care units of an academic tertiary hospital. Our sole exclusion criterion was upper gastrointestinal bleeding at intensive care unit admission. We collected baseline variables and stress ulcer prophylaxis indications according to the institutional protocol and use of prophylaxis. Our primary outcome was adherence to the stress ulcer prophylaxis protocol. Secondary outcomes were appropriate use of stress ulcer prophylaxis, upper gastrointestinal bleeding incidence and factors associated with appropriate use of stress ulcer prophylaxis.
Two hundred thirty-four patients were enrolled from July 2nd through July 31st, 2018. Patients were 52 ± 20 years old, 125 (53%) were surgical patients, and the mean SAPS 3 was 52 ± 20. In the longitudinal follow-up, 1499 patient-days were studied; 1069 patient-days had stress ulcer prophylaxis indications, and 777 patient-days contained prophylaxis use (73% stress ulcer prophylaxis protocol adherence). Of the 430 patient-days without stress ulcer prophylaxis indications, 242 involved prophylaxis (56% inappropriate stress ulcer prophylaxis use). The overall appropriate use of stress ulcer prophylaxis was 64%. Factors associated with proper stress ulcer prophylaxis prescription were mechanical ventilation OR 2.13 (95%CI 1.64 - 2.75) and coagulopathy OR 2.77 (95%CI 1.66 - 4.60). The upper gastrointestinal bleeding incidence was 12.8%.
Adherence to the stress ulcer prophylaxis protocol was low and inappropriate use of stress ulcer prophylaxis was frequent in this cohort of critically ill patients.
Abstract
Revista Brasileira de Terapia Intensiva. 2020;32(1):133-142
DOI 10.5935/0103-507X.20200019
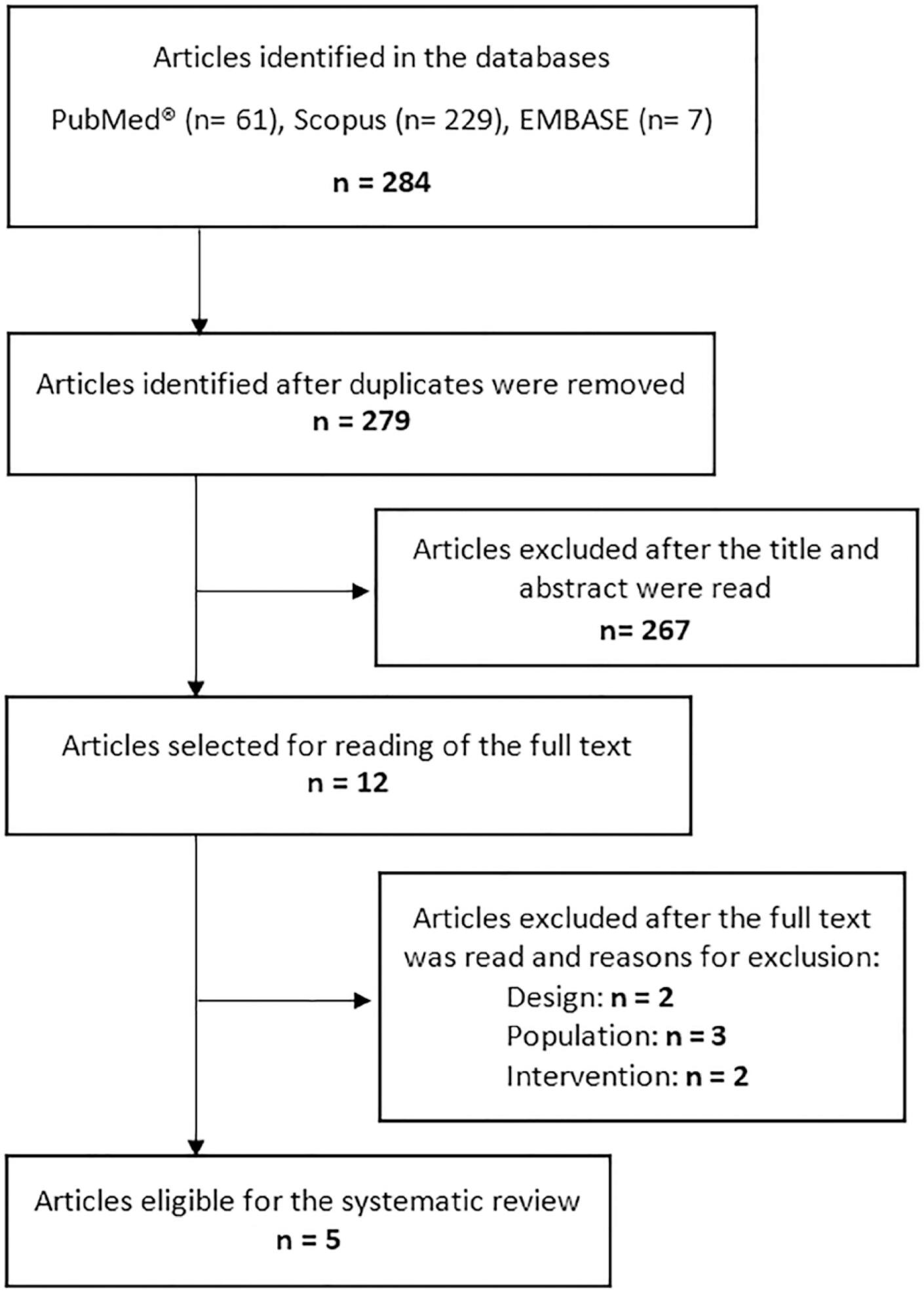
This systematic review of longitudinal studies aimed to evaluate the effect of enteral feeding of critically ill adult and pediatric patients in the prone position on gastric residual volume and other clinical outcomes. A literature search was conducted in the databases PubMed, Scopus and Embase using terms related to population and intervention. Two independent reviewers analyzed the titles and abstracts, and data collection was performed using a standardized form. Discrepancies were resolved by a third reviewer. The methodological quality of the studies was evaluated considering the potential for systematic errors, and the data were qualitatively analyzed. Four studies with adult patients and one with preterm patients were included. The gastric residual volume was evaluated as the main outcome: three studies did not show differences in the gastric residual volume between the prone and supine positions (p > 0.05), while one study showed a higher gastric residual volume during enteral feeding in the prone position (27.6mL versus 10.6mL; p < 0.05), and another group observed a greater gastric residual volume in the supine position (reduction of the gastric residual volume by 23.3% in the supine position versus 43.9% in the prone position; p < 0.01). Two studies evaluated the frequency of vomiting; one study found that it was higher in the prone position (30 versus 26 episodes; p < 0.001), while the other study found no significant difference (p > 0.05). The incidence of aspiration pneumonia and death were evaluated in one study, with no difference between groups (p > 0.05). The literature on the administration of enteral feeding in the prone position in critically ill patients is sparse and of limited quality, and the results regarding gastric residual volume are contradictory. Observational studies with appropriate sample sizes should be conducted to support conclusions on the subject.
Abstract
Revista Brasileira de Terapia Intensiva. 2020;32(1):115-122
DOI 10.5935/0103-507X.20200017
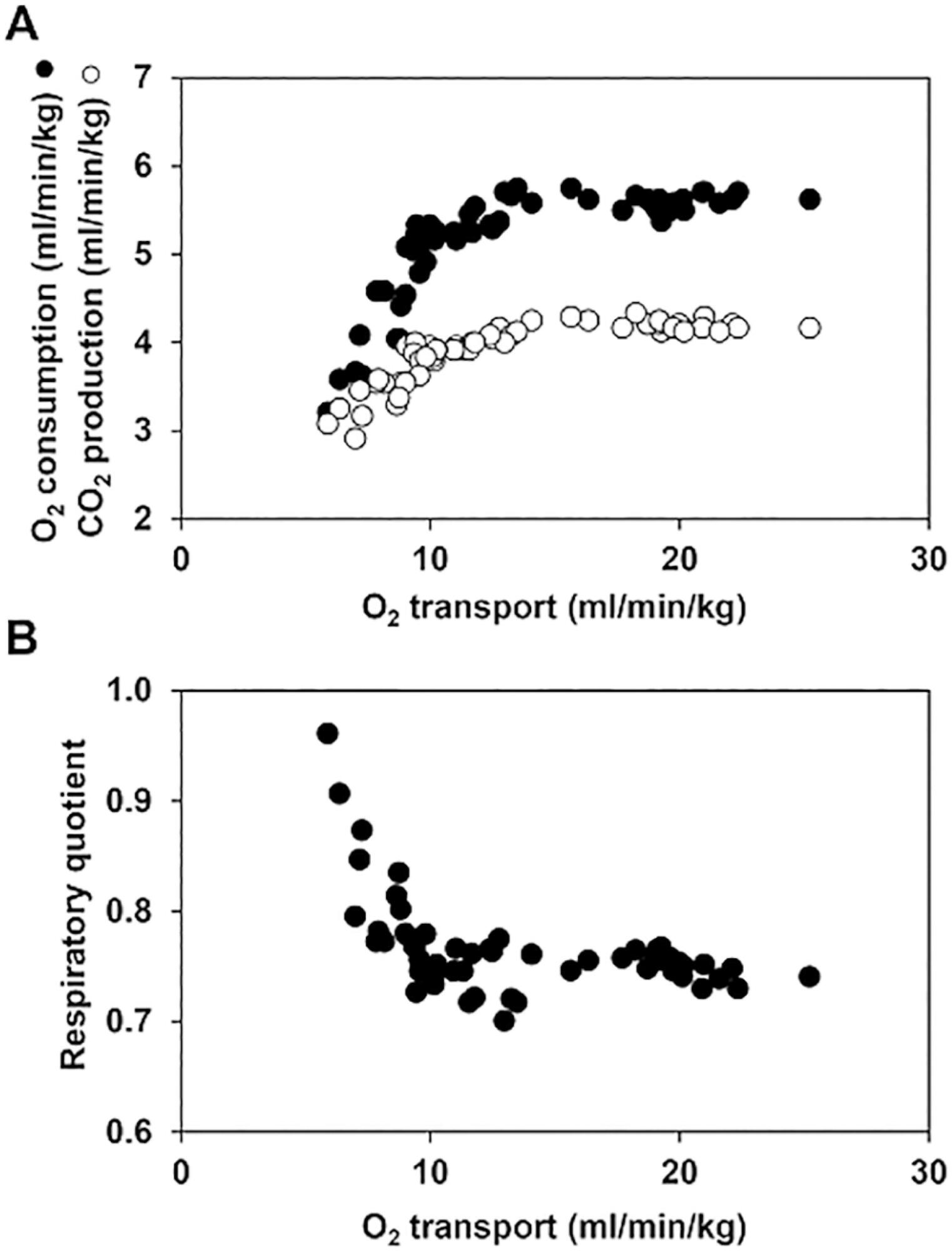
The central venous minus arterial carbon dioxide pressure to arterial minus central venous oxygen content ratio (Pcv-aCO2/Ca-cvO2) has been proposed as a surrogate for respiratory quotient and an indicator of tissue oxygenation. Some small observational studies have found that a Pcv-aCO2/Ca-cvO2 > 1.4 was associated with hyperlactatemia, oxygen supply dependency, and increased mortality. Moreover, Pcv-aCO2/Ca-cvO2 has been incorporated into algorithms for tissue oxygenation evaluation and resuscitation. However, the evidence for these recommendations is quite limited and of low quality. The goal of this narrative review was to analyze the methodological bases, the pathophysiologic foundations, and the experimental and clinical evidence supporting the use of Pcv-aCO2/Ca-cvO2 as a surrogate for respiratory quotient. Physiologically, the increase in respiratory quotient secondary to critical reductions in oxygen transport is a life-threatening and dramatic event. Nevertheless, this event is easily noticeable and probably does not require further monitoring. Since the beginning of anaerobic metabolism is indicated by the sudden increase in respiratory quotient and the normal range of respiratory quotient is wide, the use of a defined cutoff of 1.4 for Pcv-aCO2/Ca-cvO2 is meaningless. Experimental studies have shown that Pcv-aCO2/Ca-cvO2 is more dependent on factors that modify the dissociation of carbon dioxide from hemoglobin than on respiratory quotient and that respiratory quotient and Pcv-aCO2/Ca-cvO2 may have distinct behaviors. Studies performed in critically ill patients have shown controversial results regarding the ability of Pcv-aCO2/Ca-cvO2 to predict outcome, hyperlactatemia, microvascular abnormalities, and oxygen supply dependency. A randomized controlled trial also showed that Pcv-aCO2/Ca-cvO2 is useless as a goal of resuscitation. Pcv-aCO2/Ca-cvO2 should be carefully interpreted in critically ill patients.
Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(4):571-581
DOI 10.5935/0103-507X.20190070
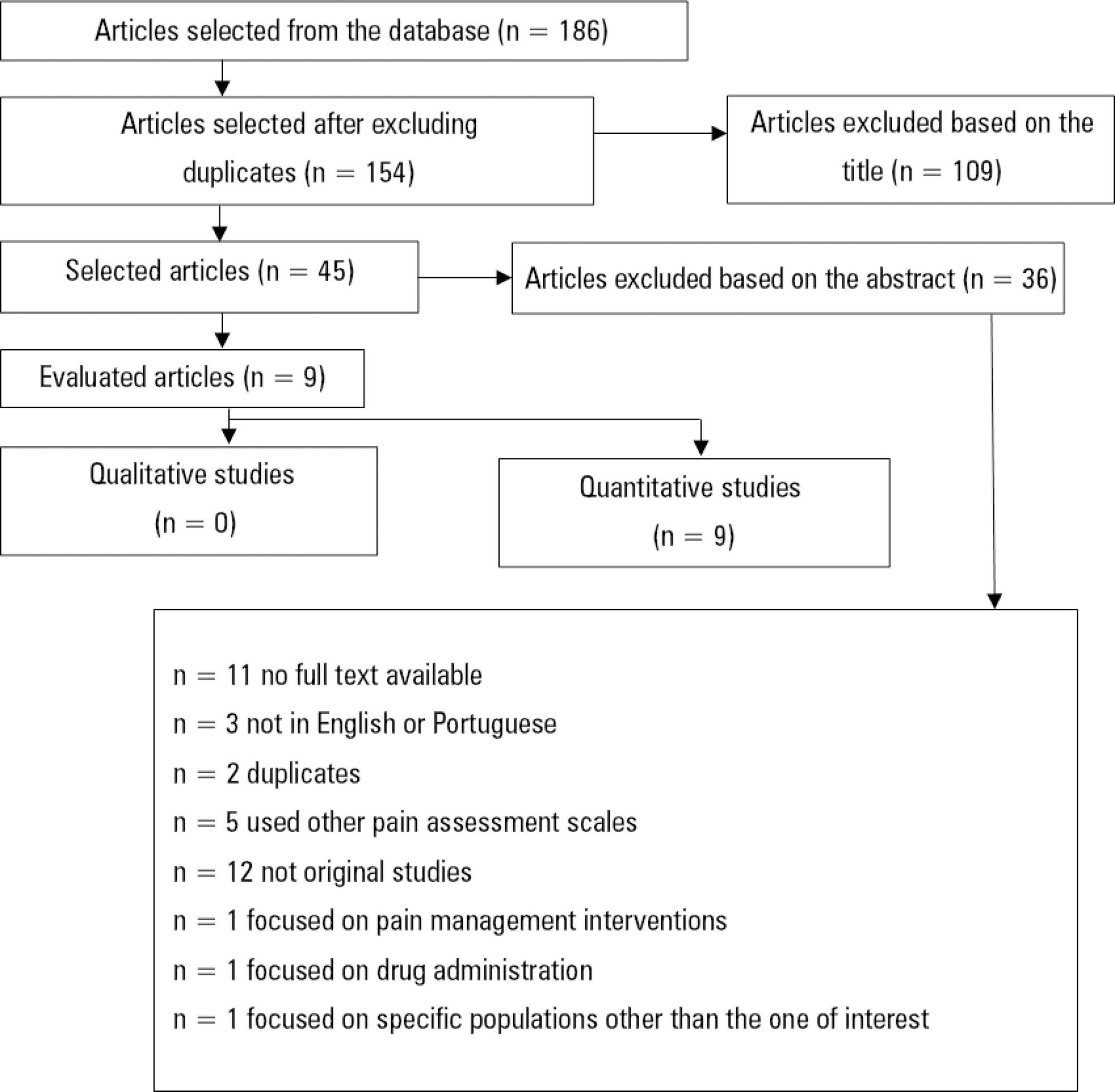
Descrever a adequação de duas escalas comportamentais, a Behavioral Pain Scale e a Critical Care Pain Observation Tool, para a avaliação da dor em pacientes intubados orotraquealmente, internados em unidades de terapia intensiva.
Utilizando a metodologia recomendada pelo Centro Cochrane, foi realizada revisão sistemática da literatura, na base de dados eletrônica EBSCO host (CINAHL Complete, MEDLINE®Complete, Nursing & Allied Health Collection: Comprehensive, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, Library, Information Science & Technology Abstracts, MedicLatina). Foram realizadas duas pesquisas com os seguintes termos em inglês no campo de pesquisa: "behavioral pain scale" AND "critical care pain observation tool" AND "behavioral pain scale" OR "critical care pain observation tool". Dois revisores independentes realizaram a avaliação crítica, a extração e a síntese dos dados.
Foram incluídos 15 estudos que evidenciaram que a Behavioral Pain Scale e a Critical Care Pain Observation Tool eram duas escalas válidas e confiáveis para a avaliação da dor em pacientes intubados orotraquealmente e internados em unidade de terapia intensiva. As escalas apresentaram propriedades psicométricas semelhantes, bem como boa confiabilidade.
Ambas as escalas são adequadas para a avaliação da dor em pacientes intubados orotraquealmente, internados em unidade de terapia intensiva, contudo, apresentam limitações em populações específicas como doentes vítimas de trauma, queimados e do foro neurocirurgico. É sugerida a realização de mais estudos sobre o tema e em populações específicas.
Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(4):511-520
DOI 10.5935/0103-507X.20190088
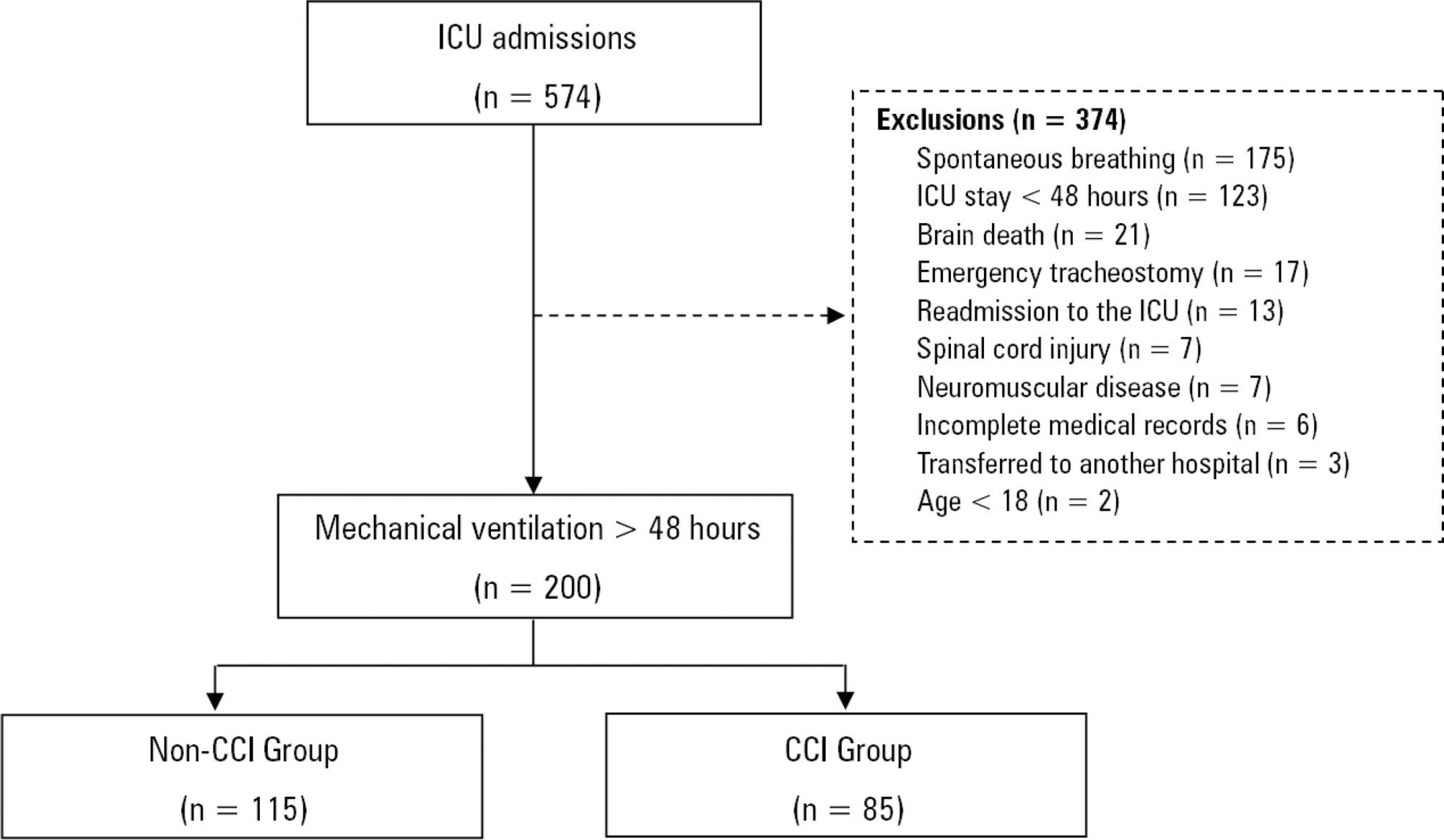
To characterize patients with chronic critical illness and identify predictors of development of chronic critical illness.
Prospective data was collected for 1 year in the intensive care unit of a general hospital in Southern Brazil. Three logistic regression models were constructed to identify factors associated with chronic critical illness.
Among the 574 subjects admitted to the intensive care unit, 200 were submitted to mechanical ventilation. Of these patients, 85 (43.5%) developed chronic critical illness, composing 14.8% of all the patients admitted to the intensive care unit. The regression model that evaluated the association of chronic critical illness with conditions present prior to intensive care unit admission identified chronic renal failure in patients undergoing hemodialysis (OR 3.57; p = 0.04) and a neurological diagnosis at hospital admission (OR 2.25; p = 0.008) as independent factors. In the model that evaluated the association of chronic critical illness with situations that occurred during intensive care unit stay, muscle weakness (OR 2.86; p = 0.01) and pressure ulcers (OR 9.54; p < 0.001) had the strongest associations. In the global multivariate analysis (that assessed previous factors and situations that occurred in the intensive care unit), hospital admission due to neurological diseases (OR 2.61; p = 0.03) and the development of pressure ulcers (OR 9.08; p < 0.001) had the strongest associations.
The incidence of chronic critical illness in this study was similar to that observed in other studies and had a strong association with the diagnosis of neurological diseases at hospital admission and chronic renal failure in patients undergoing hemodialysis, as well as complications developed during hospitalization, such as pressure ulcers and muscle weakness.