Abstract
Rev Bras Ter Intensiva. 2019;31(4):497-503
DOI 10.5935/0103-507X.20190087
To evaluate whether electromyographical findings could predict intensive care unit mortality among mechanically ventilated septic patients under profound sedation.
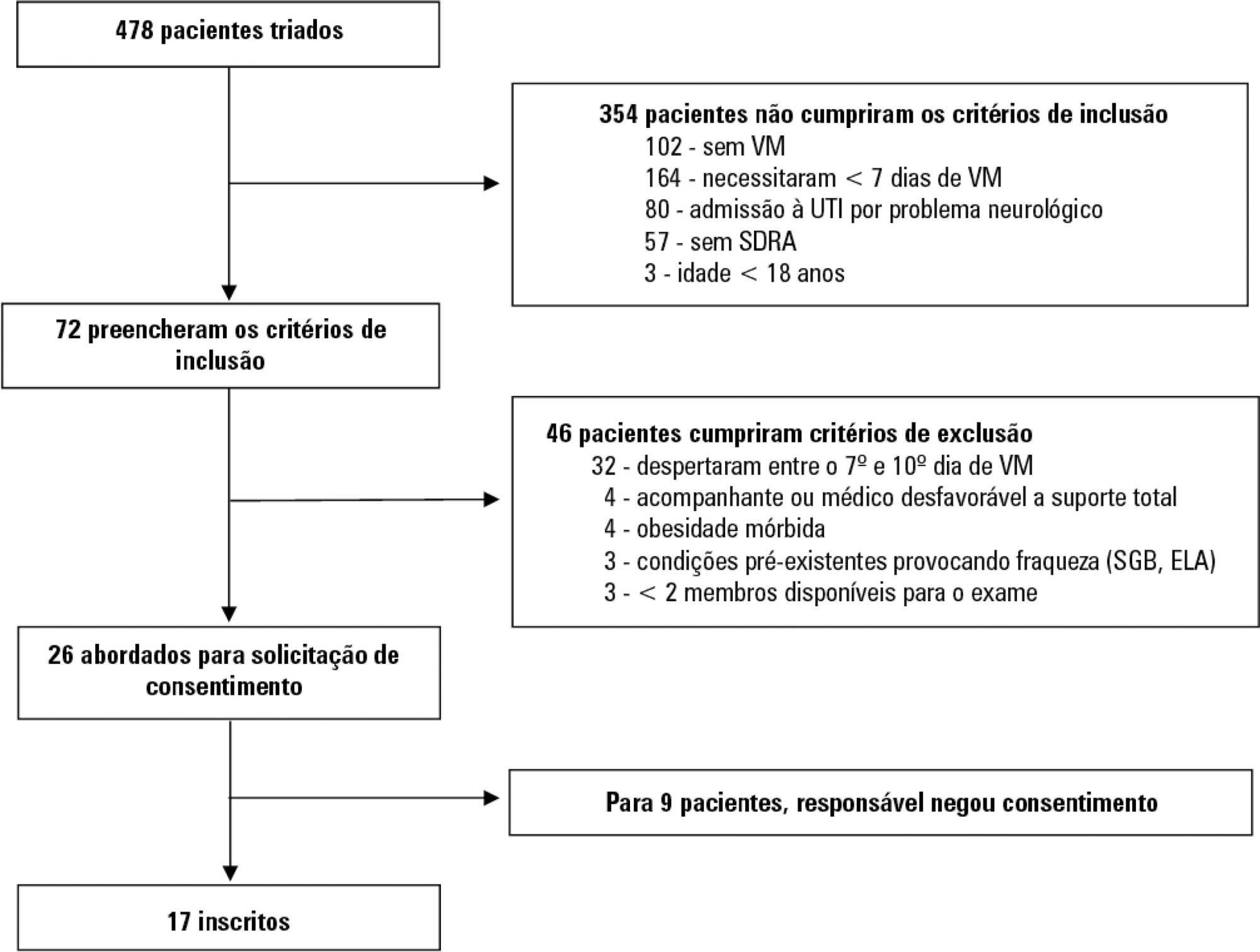
A prospective cohort study that consecutively enrolled moderate-severe acute respiratory distress syndrome (partial pressure of oxygen/fraction of inspired oxygen < 200) patients who were ≥ 18 years of age, dependent on mechanical ventilation for ≥ 7 days, and under profound sedation (Richmond Agitation Sedation Scale ≤ -4) was conducted. Electromyographic studies of the limbs were performed in all patients between the 7th and the 10th day of mechanical ventilation. Sensory nerve action potentials were recorded from the median and sural nerves. The compound muscle action potentials were recorded from the median (abductor pollicis brevis muscle) and common peroneal (extensor digitorum brevis muscle) nerves.
Seventeen patients were enrolled during the seven months of the study. Nine patients (53%) had electromyographic signs of critical illness myopathy or neuropathy. The risk of death during the intensive care unit stay was increased in patients with electromyographical signs of critical illness myopathy or neuropathy in comparison to those without these diagnostics (77.7% versus 12.5%, log-rank p = 0.02).
Electromyographical signs of critical illness myopathy or neuropathy between the 7th and the 10th day of mechanical ventilation may be associated with intensive care unit mortality among moderate-severe acute respiratory distress syndrome patients under profound sedation, in whom clinical strength assessment is not possible.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):504-510
DOI 10.5935/0103-507X.20190067
To evaluate the risk factors for protein-caloric inadequacy in critically ill patients.
Prospective cohort study of patients hospitalized in an adult intensive care unit between February and November 2017. Patients were followed for 7 days. The conditional probability of inadequacy was calculated using the Kaplan-Meier method and the 95% log-rank test. To assess the risk of inadequacy, crude and adjusted hazard ratios (HR) were calculated using Cox regression with a 95% confidence interval.
Of the 130 patients, 63.8% were male, 73.8% were <60 years of age, and 49.2% were diagnosed with trauma. The mean APACHE II score was 24 points, and 70.0% of the patients had a protein-caloric adequacy >80%. In the univariate analysis, the significant variables for inadequacy were use of vasoactive drugs, interruptions of diet and failure to initiate nutrition early. In the final model, patients who presented with vomiting/gastric residue (adjusted HR = 22.5; 95%CI 5.14 - 98.87) and fasting for extubation (adjusted HR = 14.75; 95%CI 3.59 - 60.63) and for examinations and interventions (adjusted HR = 12.46; 95%CI 4.52 - 34.36) had a higher risk of not achieving protein-caloric adequacy.
Achievement of nutritional goals > 80.0% occurred in 70.0% of patients. The risk factors for protein-caloric inadequacy were nutritional interruptions, especially due to vomiting/gastric residue and fasting for extubation, exams and surgical procedures.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):379-385
DOI 10.5935/0103-507X.20190061
To collect data on the use of The Nutrition Risk in Critically Ill (NUTRIC) score.
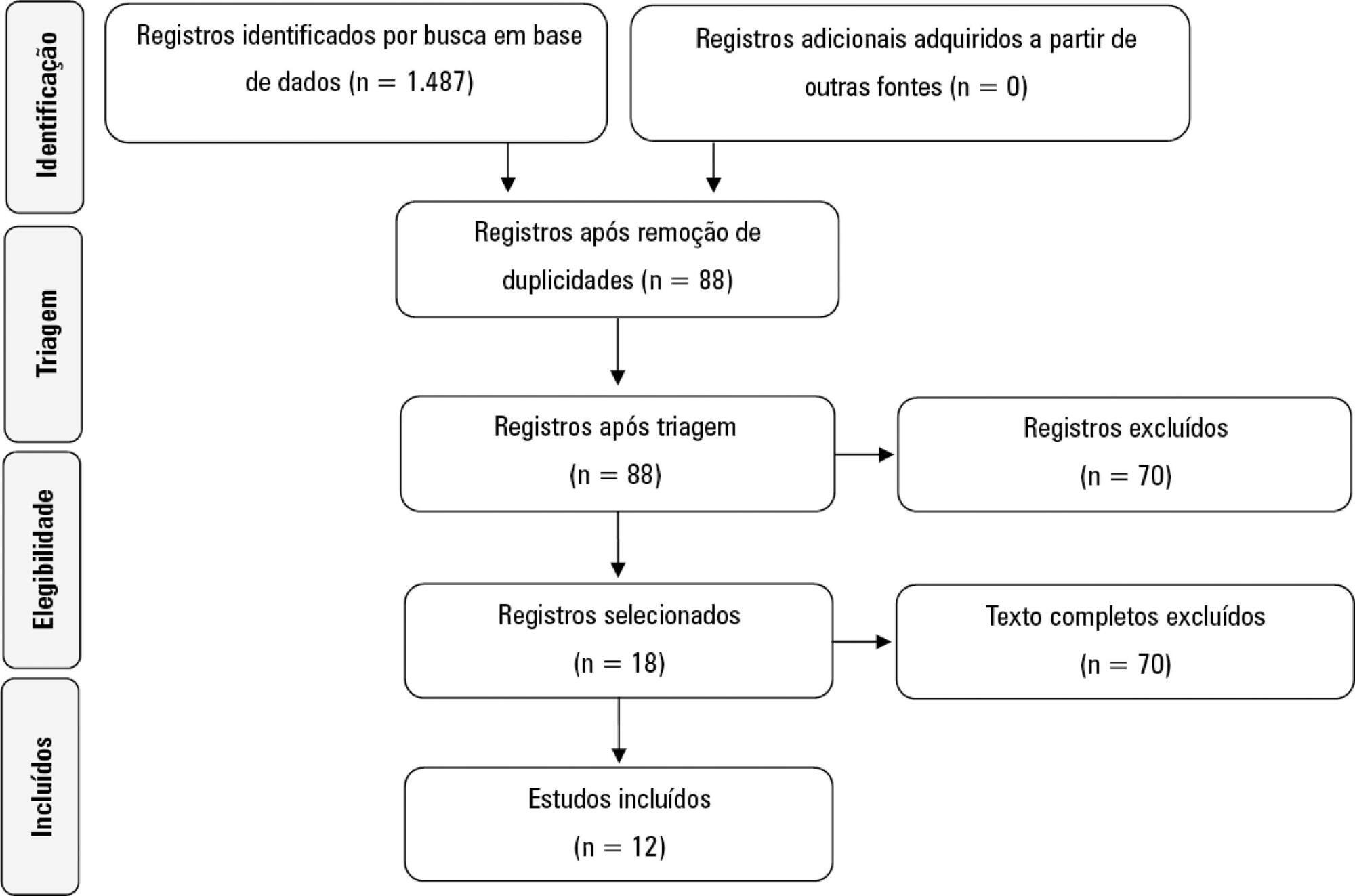
A systematic literature search was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Reviews, abstracts, dissertations, protocols and case reports were excluded from this review; to be included in the review, studies needed to specifically evaluate the NUTRIC score and to have been published in English, Spanish or Portuguese.
We included 12 (0.8%) studies from our search in this review. Ten studies (83.3%) were observational, 1 was a pilot study (8.3%) and 1 was a randomized control trial (8.3%). All of the included studies (100%) chose not to use IL-6 and considered a high nutritional risk cutoff point ≥ 5. There were 11 (91.7%) English language studies versus 1 (8.3%) Spanish language study. Mechanical ventilation and a high NUTRIC score were significantly correlated in four studies. The association between intensive care unit or hospital length of stay and nutritional high risk was significant in three studies. Seven studies found a statistically significant association between the NUTRIC score and mortality.
The NUTRIC score is related to clinical outcomes, such as length of hospital stay, and is appropriate for use in critically ill patients in intensive care units.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):210-216
DOI 10.5935/0103-507X.20190035
To evaluate the association of nutritional status and protein intake with the clinical outcomes of critically ill patients receiving enteral nutrition therapy in an intensive care unit.
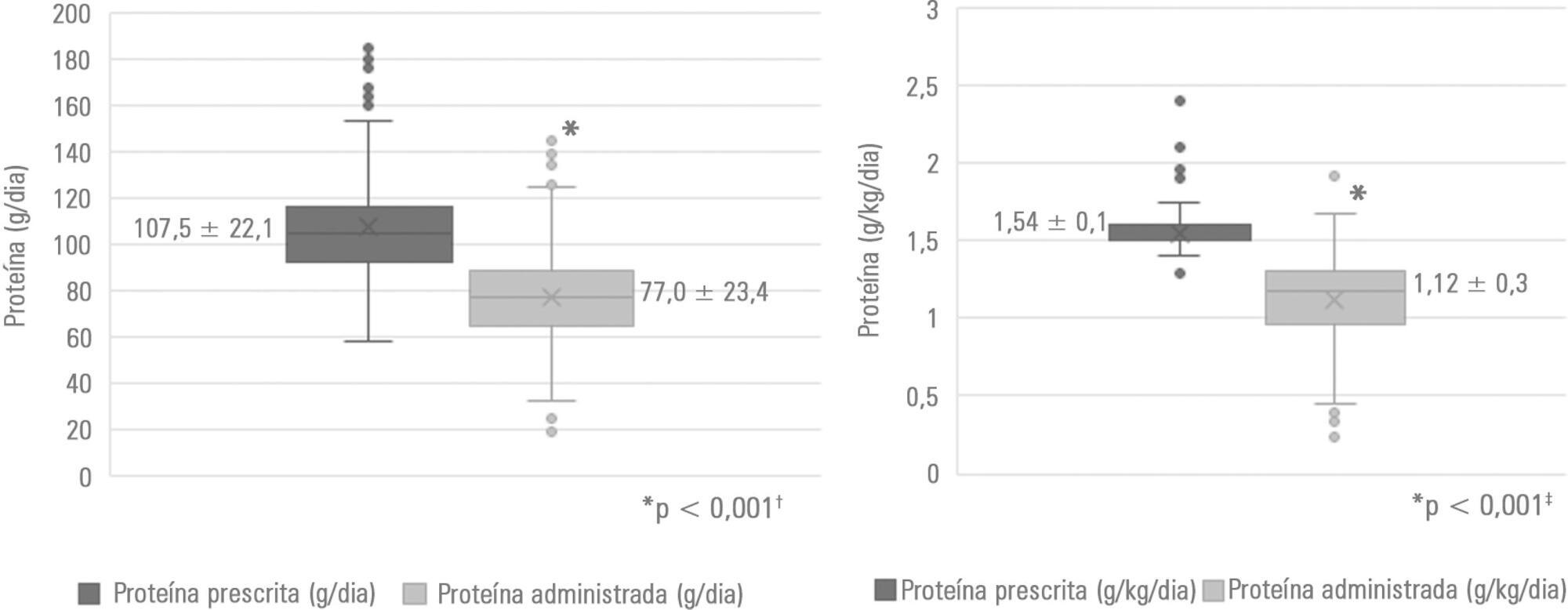
A retrospective observational analytical study was performed by collecting secondary data recorded in medical records of patients ≥ 18 years of age who were admitted to the intensive care unit and who received exclusive enteral nutrition therapy for at least 72 hours in 2017. Nutritional status was assessed by body mass index and arm circumference. For the estimation of protein requirements, the recommendation of the American Society for Parenteral and Enteral Nutrition was considered. Nutritional adequacy was assessed by the daily collection of prescribed and administered enteral formula. In the analyses, parametric and nonparametric tests were used, and significance was set at p <0.05.
Of the 188 patients evaluated, 71.3% were male. The median age of the patients was 48.5 years (31.0 - 63.75). The main clinical diagnosis was trauma (46.3%), and eutrophic was the most frequent nutritional status (54.8% according to body mass index and 46.4% according to arm circumference). Protein adequacy was not attained in 56.4% of patients, and only 46.8% reached the minimum protein recommendation. The occurrence of mortality was associated with nutritional diagnosis, body mass index (p = 0.023), arm circumference (p = 0.041) and protein adequacy (p = 0.012).
Nutritional status and protein intake were significantly associated with the clinical outcomes of critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):147-155
DOI 10.5935/0103-507X.20190024
To analyze the satisfaction, medical situation understanding and symptoms of anxiety and depression in family members of patients admitted to the intensive care unit.
The family members of patients who were hospitalized for ≥ 72 hours were invited to participate in the study, which was performed in a public hospital. Questionnaires were answered to assess the understanding of the diagnosis, treatment and prognosis, and the support received in the intensive care unit. The family needs were also evaluated using a modified version of the Critical Care Family Needs Inventory (CCFNI). The Hospital Anxiety and Depression Scale (HADS) was used to assess the symptoms of anxiety and depression.
A total of 35 family members were interviewed within the patients' first week of stay in the intensive care unit. Most patients (57.1%) were male, aged 54 ± 19 years. Sepsis was the main reason for admission to the intensive care unit (40%); the median of the Simplified Acute Physiology Score (SAPS) 3 was 68 (48 - 77), and 51.4% of the patients died in the intensive care unit. The majority of the family members were female (74.3%) and were sons or daughters of patients (54.3%), with a mean age of 43.2 ± 14 years. Overall, 77.1% of the family members were satisfied with the intensive care unit. A total of 37.1% of the family members did not understand the prognosis. Receiving clear and complete information in the intensive care unit and the doctor being accessible were factors that were significantly correlated with the overall family satisfaction. The prevalence of symptoms of anxiety (60%) and depression (54.3%) in the family members was high.
The emotional distress of family members is high during a patient's hospitalization in the intensive care unit, although satisfaction is also high. Clear and complete information provided by the intensivist and the support received in the intensive care unit are significantly correlated with the satisfaction of family members in a public hospital.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):171-179
DOI 10.5935/0103-507X.20190025
To evaluate differences in outcomes for an optimized calorie and high protein nutrition therapy versus standard nutrition care in critically ill adult patients.
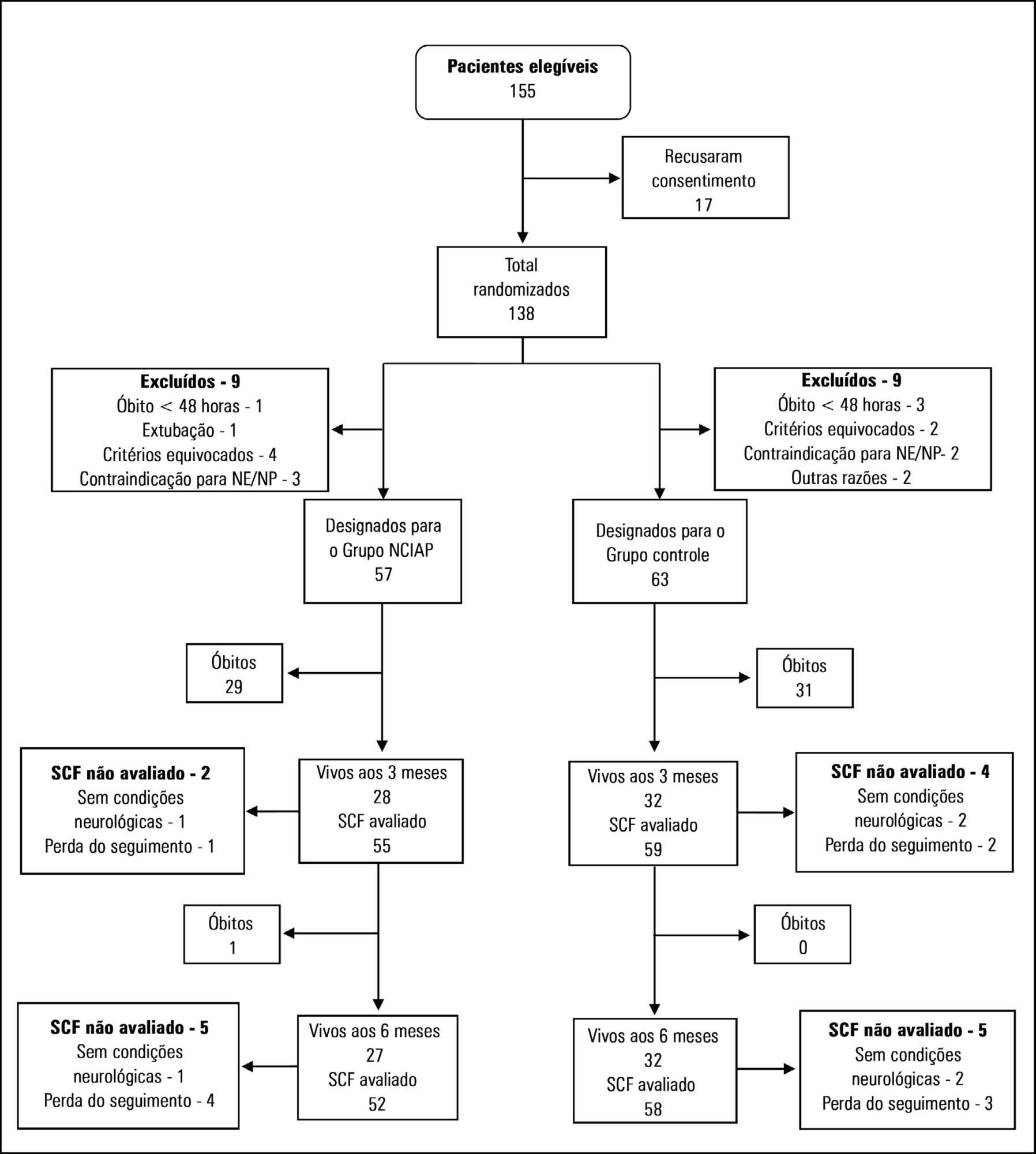
We randomized patients expected to stay in the intensive care unit for at least 3 days. In the optimized calorie and high protein nutrition group, caloric intake was determined by indirect calorimetry, and protein intake was established at 2.0 to 2.2g/kg/day. The control group received 25kcal/kg/day of calories and 1.4 to 1.5g/kg/day protein. The primary outcome was the physical component summary score obtained at 3 and 6 months. Secondary outcomes included handgrip strength at intensive care unit discharge, duration of mechanical ventilation and hospital mortality.
In total, 120 patients were included in the analysis. There was no significant difference between the two groups in calories received. However, the amount of protein received by the optimized calorie and high protein nutrition group was significantly higher compared with the control group. The physical component summary score at 3 and 6 months did not differ between the two groups nor did secondary outcomes. However, after adjusting for covariates, a negative delta protein (protein received minus predetermined protein requirement) was associated with a lower physical component summary score at 3 and 6 months postrandomization.
In this study optimized calorie and high protein strategy did not appear to improve physical quality of life compared with standard nutrition care. However, after adjusting for covariates, a negative delta protein was associated with a lower physical component summary score at 3 and 6 months postrandomization. This association exists independently of the method of calculation of protein target.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):34-38
DOI 10.5935/0103-507X.20190004
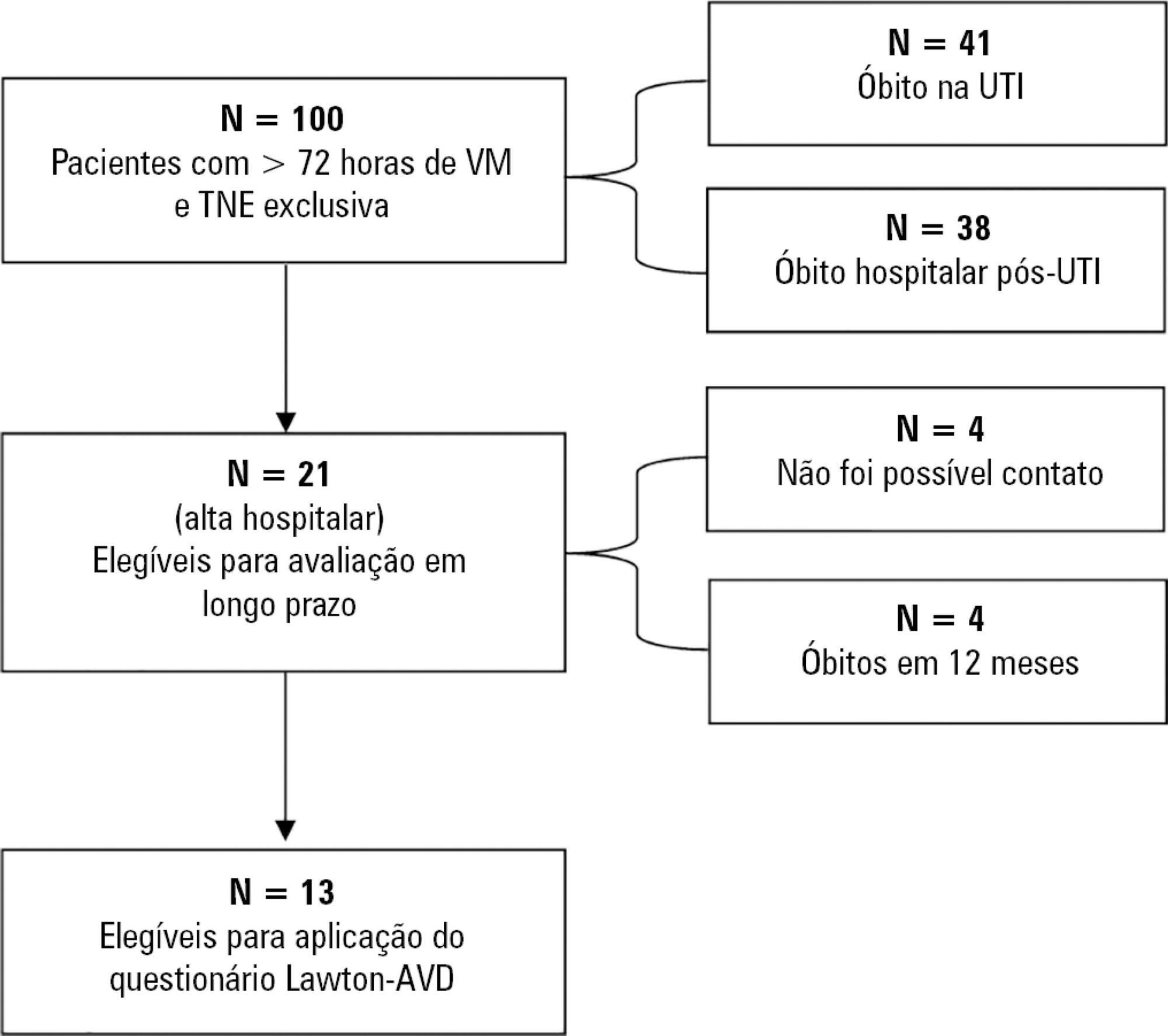
To correlate short-term (duration of mechanical ventilation and length of intensive care unit stay) and long-term (functional capacity) clinical outcomes of patients who reached nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization in the intensive care unit.
This was a prospective observational pilot study conducted in an 18-bed intensive care unit. A total of 100 mechanically ventilated patients receiving exclusive enteral nutritional support and receiving intensive care for more than 72 hours were included. Patients who never received enteral nutrition, those with spinal cord trauma, pregnant women, organ donors and cases of family refusal were excluded. The variables studied were nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization, length of intensive care unit stay, duration of mechanical ventilation and the ability to perform activities of daily living after 12 months, assessed via telephone contact using the Lawton Activities of Daily Living Scale.
The mean duration of mechanical ventilation was 18 ± 9 days, and the mean intensive care unit length of stay was 19 ± 8 days. Only 45% of the patients received more than 70% of the target nutrition in 72 hours. There was no association between nutritional adequacy and short-term (duration of mechanical ventilation, length of stay in the intensive care unit and mortality) or long-term (functional capacity and mortality) clinical outcomes.
Critically ill patients receiving caloric intake ≥ 70% in the first 72 hours of hospitalization did not present better outcomes in the short term or after 1 year.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):317-326
DOI 10.5935/0103-507X.20180052
To characterize the transport of severely ill patients with extracorporeal respiratory or cardiovascular support.
A series of 18 patients in the state of São Paulo, Brazil is described. All patients were consecutively evaluated by a multidisciplinary team at the hospital of origin. The patients were rescued, and extracorporeal membrane oxygenation support was provided on site. The patients were then transported to referral hospitals for extracorporeal membrane oxygenation support. Data were retrieved from a prospectively collected database.
From 2011 to 2017, 18 patients aged 29 (25 - 31) years with a SAPS 3 of 84 (68 - 92) and main primary diagnosis of leptospirosis and influenza A (H1N1) virus were transported to three referral hospitals in São Paulo. A median distance of 39 (15 - 82) km was traveled on each rescue mission during a period of 360 (308 - 431) min. A median of one (0 - 2) nurse, three (2 - 3) physicians, and one (0 - 1) physical therapist was present per rescue. Seventeen rescues were made by ambulance, and one rescue was made by helicopter. The observed complications were interruption in the energy supply to the pump in two cases (11%) and oxygen saturation < 70% in two cases. Thirteen patients (72%) survived and were discharged from the hospital. Among the nonsurvivors, there were two cases of brain death, two cases of multiple organ dysfunction syndrome, and one case of irreversible pulmonary fibrosis.
Transportation with extracorporeal support occurred without serious complications, and the hospital survival rate was high.