Abstract
Rev Bras Ter Intensiva. 2012;24(3):278-283
DOI 10.1590/S0103-507X2012000300012
OBJECTIVE: This study analyzed acute respiratory failure caused by acute pulmonary edema, as well as chronic obstructive pulmonary disease exacerbation, that was treated with non-invasive mechanical ventilation to identify the factors that are associated with the success or failure non-invasive mechanical ventilation in urgent and emergency service. METHODS: This study was a prospective, descriptive and analytical study. We included patients of both genders aged >18 years who used non-invasive mechanical ventilation due to acute respiratory failure that was secondary to acute pulmonary edema or chronic obstructive pulmonary disease exacerbation. Patients with acute respiratory failure that was secondary to pathologies other than acute pulmonary edema and chronic obstructive pulmonary disease or who presented with contraindications for the technique were excluded. Expiratory pressures between 5 and 8 cmH2O and inspiratory pressures between 10 and 12 cmH2O were used. Supplemental oxygen maintained peripheral oxygen saturation at >90%. The primary outcome was endotracheal intubation. RESULTS: A total of 152 patients were included. The median non-invasive mechanical ventilation time was 6 hours (range 1 - 32 hours) for chronic obstructive pulmonary disease patients (n=60) and 5 hours (range 2 - 32 hours) for acute pulmonary edema patients (n=92). Most (75.7%) patients progressed successfully. However, reduced APACHE II scores and lower peripheral oxygen saturation were observed. These results were statistically significant in patients who progressed to intubation (p<0.001). BiPAP (Bi-level Positive Airway Pressure portable ventilator), as continuous positive airway pressure use increased the probability of endotracheal intubation 2.3 times (p=0.032). Patients with acute pulmonary edema and elevated GCS scores also increased the probability of success. CONCLUSION: Respiratory frequency >25 rpm, higher APACHE II scores, BiPAP use and chronic obstructive pulmonary disease diagnosis were associated with endotracheal intubation. Higher GCS and SpO2 values were associated with NIV success. Non-invasive mechanical ventilation can be used in emergency services in acute respiratory failure cases caused by acute pulmonary edema and chronic obstructive pulmonary disease exacerbation, but patients with variables related to a higher percentage of endotracheal intubation should be specially monitored.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):157-161
DOI 10.1590/S0103-507X2012000200010
OBJECTIVE: Because patients hospitalized in intensive care units are at risk for poor nutrition, and nutritional therapy is not always started at an appropriate time, the present study aimed to correlate nutritional status, early nutrition, and hyperglycemia with patient mortality in an intensive care unit. METHODS: This archival cohort study used the secondary database of 453 patients who stayed at least 48 hours in an intensive care unit and were assessed for 8 days of hospitalization. Patient nutritional status was defined according to the body mass index. Early nutrition was defined as an feeding energy within the first 48 hours of hospitalization, regardless of the administration route. Blood glucose levels were monitored using a glucometer. RESULTS: A majority of patients were male (54.2%), and approximately half of patients were overweight (48.4%). At the end of the first 48 hours, 69.4% of patients had received nutrition, and only 13.5% of patients still exhibited hyperglycemia. The patients who received early nutritional therapy exhibited lower a mortality risk (p = 0.002), regardless of the presence of other factors associated with mortality. CONCLUSIONS: The significant correlation between early nutritional therapy and survival emphasizes the importance of nutrition in severely ill patients. The low frequency of hyperglycemia found in this study might indicate that the prescription of nutritional therapy and the application of an insulin protocol are appropriate at institutional intensive care units.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):162-166
DOI 10.1590/S0103-507X2012000200011
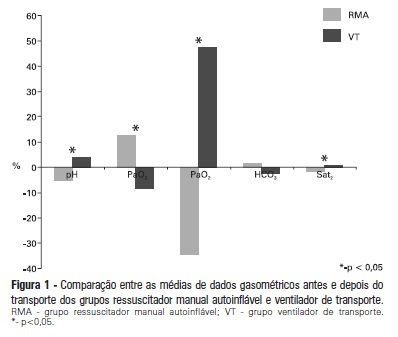
OBJECTIVE: To evaluate the effects on blood gases by two methods of ventilation (with transport ventilation or self-inflating manual resuscitator) during intra-hospital transport of patients after cardiac surgery. METHODS: Observational, longitudinal, prospective, randomized study. Two samples of arterial blood were collected at the end of the surgery and another at the end of patient transport. RESULTS: We included 23 patients: 13 in the Group with transport ventilation and 10 in the Group with self-inflating manual resuscitator. Baseline characteristics were similar between both groups, except for higher acute severity of illness in the Group with transport ventilation. We observed significant differences in comparisons of percentage variations of gasometric data: pH (transport ventilation + 4% x MR -5%, p=0.007), PaCO2 (-8% x +13%, p=0.006), PaO2 (+47% x -34%, p=0.01) and SatO2 (+0.6% x -1.7%, p=0.001). CONCLUSION: The use of mechanical ventilation results in fewer repercussions for blood gas analysis in the intra-hospital transport of cardiac surgery patients.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):167-172
DOI 10.1590/S0103-507X2012000200012
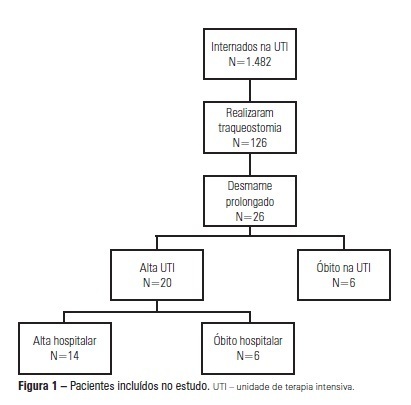
OBJECTIVE: We aimed to assess the use of noninvasive ventilation devices in patients with prolonged weaning following tracheotomy. METHODS: We performed a retrospective observational study using data collected from the clinical records of tracheotomized patients diagnosed with prolonged weaning. The participants were hospitalized in the adult intensive care unit of Moinhos de Vento Hospital, Porto Alegre (RS) between December 2007 and December 2008. RESULTS: In the data collection period, 1,482 patients were admitted to the intensive care unit. In total, 126 patients underwent tracheotomies, and 26 of these patients met the inclusion criteria for participating in the study. The average age of the patients in our sample was 73 ± 12 years. In our sample, 57.7% of the participants were female, and 80.8% were admitted as a result of acute hypoxemic respiratory failure. After the tracheotomy, the patients remained under mechanical ventilation for an average of 29.8 days. After the initiation of the experimental protocol, the tracheotomized patients remained under ventilation for an average of 53.5 days on a portable noninvasive device connected to the tracheotomy. There were three possible outcomes for the patients. They were discharged, were weaned from the noninvasive ventilation, or died in the intensive care unit or hospital ward. In total, 76.9% (20/26) of the patients were discharged from the intensive care unit, and 53.8% (14/26) of the patients were discharged from the hospital. CONCLUSION: The use of noninvasive portable ventilators connected to the tracheotomy may represent an alternative for discontinuing ventilationand discharging tracheotomized patients with prolonged ventilatory weaning from intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):143-150
DOI 10.1590/S0103-507X2012000200008
OBJECTIVE: To determine the prevalence of infections in Brazilian intensive care units and the associated mortality by analyzing the data obtained in the Extended Prevalence of Infection in Intensive Care (EPIC II) study. METHODS: EPIC II was a multicenter, international, cross-sectional prospective study of infection prevalence. It described the demographic, physiological, bacteriological, and therapeutic characteristics, outcome up to the 60th day, prevalence of infection, and mortality of all the patients admitted to the participating ICUs between zero hour and midnight on May 8, 2007. A total of 14,414 patients were included in the original study. Of these 14,414 patients, 1,235 were Brazilian and were hospitalized in 90 Brazilian ICUs. They represent the focus of this study. RESULTS: Among these 1,235 Brazilian patients, 61,6% had an infection on the day of the trial, and the lungs were the main site of infection (71.2%). Half of the patients had positive cultures, predominantly gram-negative bacilli (72%). On the day of the study, the median SOFA score was 5 (3-8) and the median SAPS II score was 36 (26-47). The infected patients had SOFA scores significantly higher than those of the non-infected patients 6 (4-9) and 3 (2-6), respectively). The overall ICU mortality rate was 28.4%: 37.6% in the infected patients, and 13.2% in the non-infected patients (p<0.001). Similarly, the in-hospital mortality rate was 34.2%, with a higher rate in the infected than in the non-infected patients (44.2% vs. 17.7%) (p<0.001). In the multivariate analysis, the main factors associated with infection incidence were emergency surgery (OR 2.89, 95%CI [1.72-4.86], p<0.001), mechanical ventilation (OR 2.06, 95% CI [1.5-2.82], p<0.001), and the SAPS II score (OR 1.04, 95% CI [1.03-1.06], p<0.001). The main factors related to mortality were ICC functional class III/ IV (OR 3.0, 95% CI [1.51-5.98], p<0.01), diabetes mellitus (OR 0.48, 95% CI [0.25-0.95], p<0.03), cirrhosis (OR 4.62, 95% CI [1.47-14,5], p<0.01), male gender (OR 0.68, 95% CI [0.46-1.0], p<0.05), mechanical ventilation (OR 1.87, 95% CI [1.19-2.95], p<0.01), hemodialysis (OR 1.98, 95% CI [1.05-3.75], p<0.03), and the SAPS II score (OR 1.08, 95% CI [1.06-1.10], p<0.001). CONCLUSION: The present study revealed a higher prevalence of infections in Brazilian ICUs than has been previously reported. There was a clear association between infection and mortality.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):173-178
DOI 10.1590/S0103-507X2012000200013
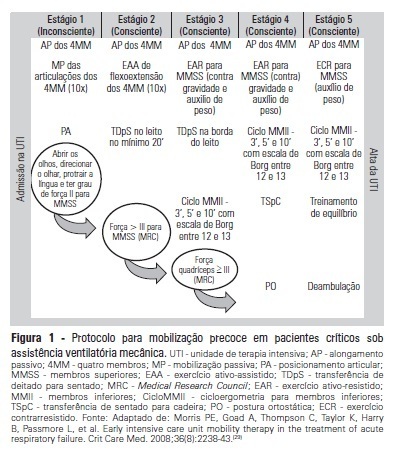
OBJECTIVE:To evaluate the effects of an early mobilization protocol on respiratory and peripheral muscles in critically ill patients. METHODS: A randomized controlled clinical trial was conducted with 59 male and female patients on mechanical ventilation. The patients were divided into a conventional physical therapy group (control group, n=14) that received the sector's standard physical therapy program and an early mobilization group (n=14) that received a systematic early mobilization protocol. Peripheral muscle strength was assessed with the Medical Research Council score, and respiratory muscle strength (determined by the maximal inspiratory and expiratory pressures) was measured using a vacuum manometer with a unidirectional valve. Systematic early mobilization was performed on five levels. RESULTS: Significant increases were observed for values for maximal inspiratory pressure and the Medical Research Council score in the early mobilization group. However, no statistically significant improvement was observed for maximal expiratory pressure or MV duration (days), length of stay in the intensive care unit (days), and length of hospital stay (days). CONCLUSION: The early mobilization group showed gains in inspiratory and peripheral muscle strength.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):151-156
DOI 10.1590/S0103-507X2012000200009
OBJECTIVE:To characterize drug prescriptions in a university hospital adult intensive care unit. METHODS: Single-center, observational, descriptive, cross-sectional study conducted at an adult general intensive care unit. The study population included all of the unit's inpatients from January to March 2011. The following characteristics for all prescriptions recorded during this period were examined: drug name (generic, brand name or abbreviation), dosage strength, pharmaceutical form, dose, route of administration, patient name, patient registration in the institution, clinic and hospital bed as well as the name, board license number, signature of the prescriber and date of the prescription. It was quantified the percentage of prescribed drugs included in the National List of Essential Drugs, the World Health Organization Model List of Essential Medicines and the University Hospital Center Pharmacotherapy Guide. The prescribed drugs were classified based on the Anatomical Therapeutic Chemical classification system (levels 1 and 2). RESULTS: Eight hundred forty-four prescriptions were reviewed from 72 patients (mean age: 59.04 ± 21.80), 54.92% of whom were female. The mean number of prescriptions per patient was 11.72 ± 11.68. The total number of drugs prescribed was 12,052 and 9,571 (79.41%) of the drugs were prescribed using the generic name. The most frequent absent information in the drug description was the pharmaceutical form of the drug (8,829/73.26%). The dosage strength was indicated in 7,231 (60%) of the prescriptions, and the prescriber and patient information were indicated in over 96% of the prescriptions. The prescribed drugs were classified in 13 therapeutic groups and 55 subgroups. Systemic antibacterials represented one of the most frequently prescribed subgroups. CONCLUSION: Most of the reviewed information was present in the prescriptions. However, the dosage strength and pharmaceutical form were absent in many prescriptions. The characterization of prescriptions at different hospital units is essential for the development of strategies that reduce drug utilization problems.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):179-183
DOI 10.1590/S0103-507X2012000200014
OBJECTIVE:The aim of the present study was to evaluate the prevalence and factors associated with bronchopulmonary dysplasia at a neonatal intensive care unit. METHODS: The study was a cross-sectional study that used secondary data from premature infants who were born with less than 32 weeks of gestational age and were admitted to a neonatal intensive care unit. Chi-square, Mann-Whitney and multivariate tests were used. Significance was set at p<0.05. RESULTS: A total of 88 premature infants were included in the study. Bronchopulmonary dysplasia occurred in 27.3% of the infants and was related to having a gestational age below 28 weeks (OR: 4.80; 95% CI: 1.50-15.34; p=0.008) and a patent ductus arteriosus (OR: 3.44; 95% CI: 1.10-10.76; p=0.034). The group with bronchopulmonary dysplasia used mechanical ventilation for a longer duration, with a median of 24.5 days (p<0.0001). At discharge, the corrected and chronological ages were higher in the group with bronchopulmonary dysplasia (p<0.0001), with respective medians of 38.4 weeks and 70.5 days. CONCLUSIONS: In this study, the prevalence of bronchopulmonary dysplasia was high; the high prevalence was related to extreme prematurity, patent ductus arteriosus, a longer period under mechanical ventilation and prolonged hospitalization. The increased survival of infants with low gestational age makes this disorder a public health issue.