Abstract
Crit Care Sci. 2024;36:e20240203en
DOI 10.62675/2965-2774.20240203-en
To assess whether the respiratory oxygenation index (ROX index) measured after the start of high-flow nasal cannula oxygen therapy can help identify the need for intubation in patients with acute respiratory failure due to coronavirus disease 2019.
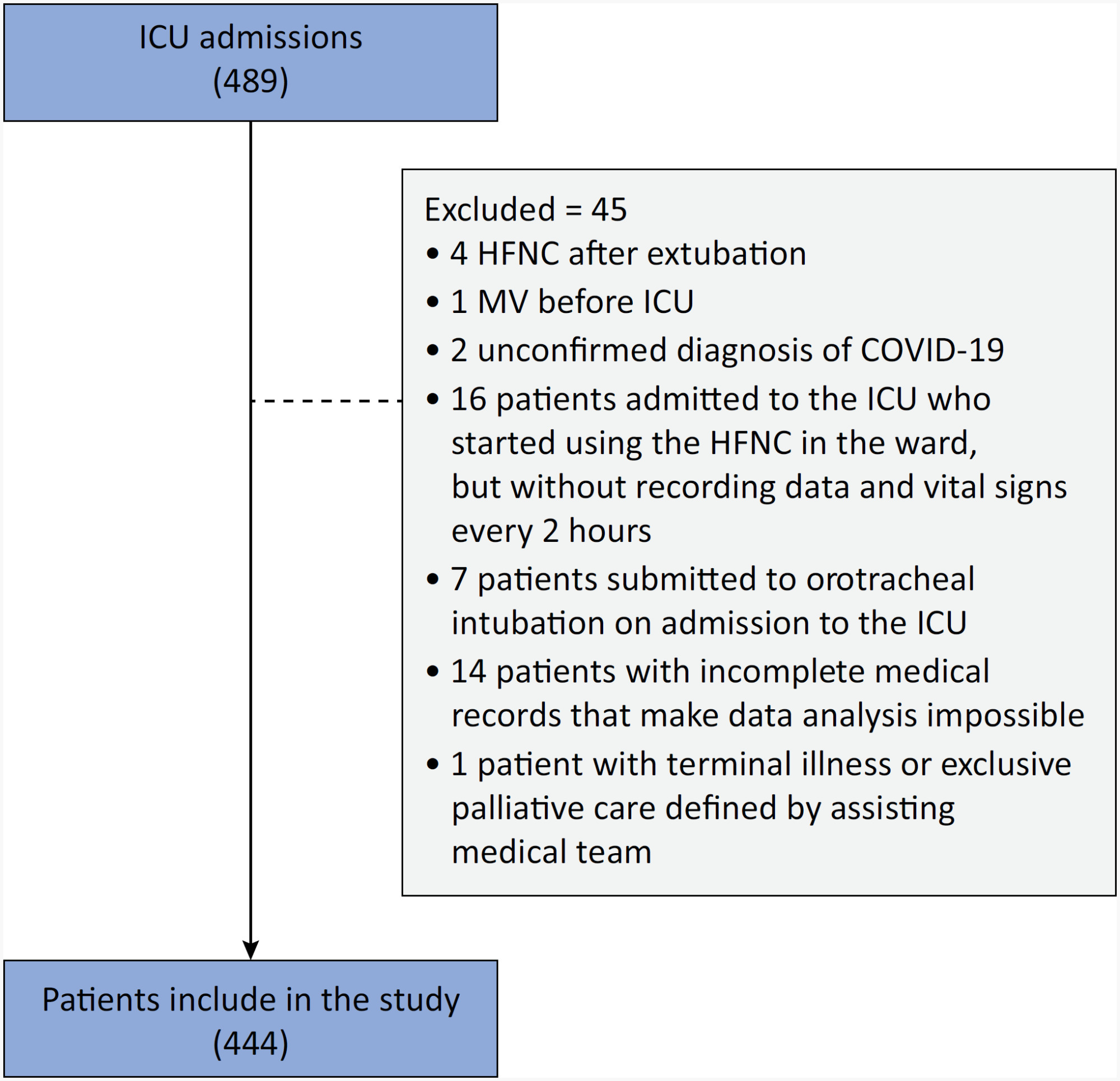
This retrospective, observational, multicenter study was conducted at the intensive care units of six Brazilian hospitals from March to December 2020. The primary outcome was the need for intubation up to 7 days after starting the high-flow nasal cannula.
A total of 444 patients were included in the study, and 261 (58.7%) were subjected to intubation. An analysis of the area under the receiver operating characteristic curve (AUROC) showed that the ability to discriminate between successful and failed high-flow nasal cannula oxygen therapy within 7 days was greater for the ROX index measured at 24 hours (AUROC 0.80; 95%CI 0.76 - 0.84). The median interval between high-flow nasal cannula initiation and intubation was 24 hours (24 - 72), and the most accurate predictor of intubation obtained before 24 hours was the ROX index measured at 12 hours (AUROC 0.75; 95%CI 0.70 - 0.79). Kaplan-Meier curves revealed a greater probability of intubation within 7 days in patients with a ROX index ≤ 5.54 at 12 hours (hazard ratio 3.07; 95%CI 2.24 - 4.20) and ≤ 5.96 at 24 hours (hazard ratio 5.15; 95%CI 3.65 - 7.27).
The ROX index can aid in the early identification of patients with acute respiratory failure due to COVID-19 who will progress to the failure of high-flow nasal cannula supportive therapy and the need for intubation.
Abstract
Crit Care Sci. 2024;36:e20240158en
DOI 10.62675/2965-2774.20240158-en
To evaluate the association of biomarkers with successful ventilatory weaning in COVID-19 patients.
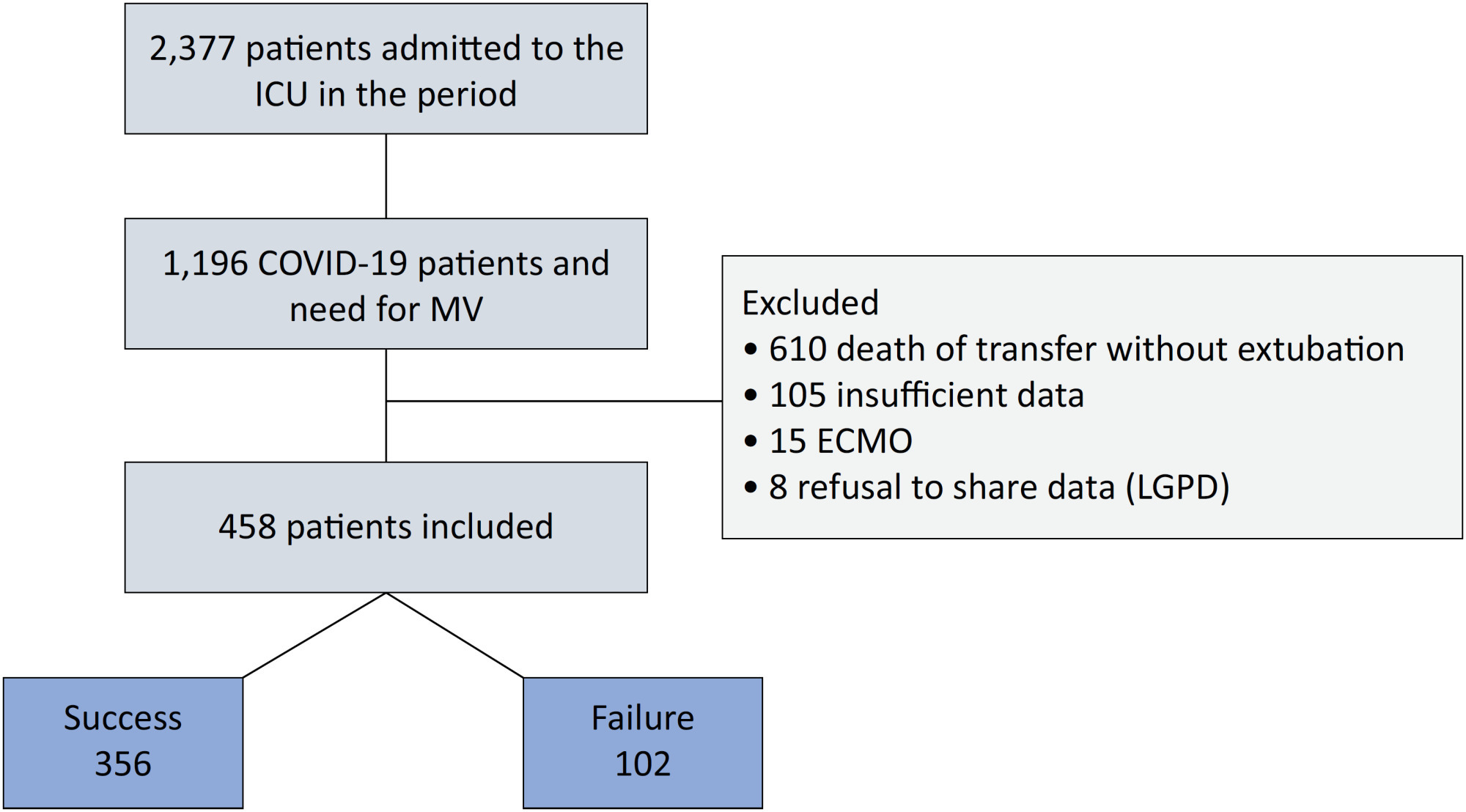
An observational, retrospective, and single-center study was conducted between March 2020 and April 2021. C-reactive protein, total lymphocytes, and the neutrophil/lymphocyte ratio were evaluated during attrition and extubation, and the variation in these biomarker values was measured. The primary outcome was successful extubation. ROC curves were drawn to find the best cutoff points for the biomarkers based on sensitivity and specificity. Statistical analysis was performed using logistic regression.
Of the 2,377 patients admitted to the intensive care unit, 458 were included in the analysis, 356 in the Successful Weaning Group and 102 in the Failure Group. The cutoff points found from the ROC curves were −62.4% for C-reactive protein, +45.7% for total lymphocytes, and −32.9% for neutrophil/lymphocyte ratio. These points were significantly associated with greater extubation success. In the multivariate analysis, only C-reactive protein variation remained statistically significant (OR 2.6; 95%CI 1.51 – 4.5; p < 0.001).
In this study, a decrease in C-reactive protein levels was associated with successful extubation in COVID-19 patients. Total lymphocytes and the neutrophil/lymphocyte ratio did not maintain the association after multivariate analysis. However, a decrease in C-reactive protein levels should not be used as a sole variable to identify COVID-19 patients suitable for weaning; as in our study, the area under the ROC curve demonstrated poor accuracy in discriminating extubation outcomes, with low sensitivity and specificity.
Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
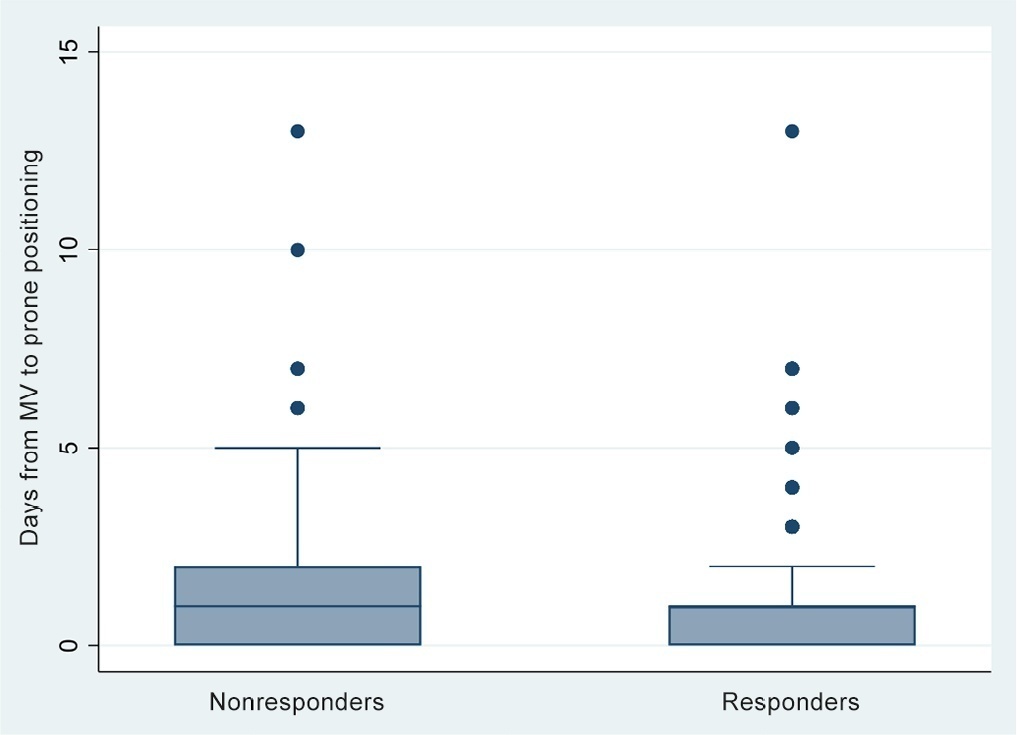
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Abstract
Rev Bras Ter Intensiva. 2022;34(1):131-140
DOI 10.5935/0103-507X.20220007-en
To evaluate the incidence of risk factors for postintubation hypotension in critically ill patients with COVID-19.
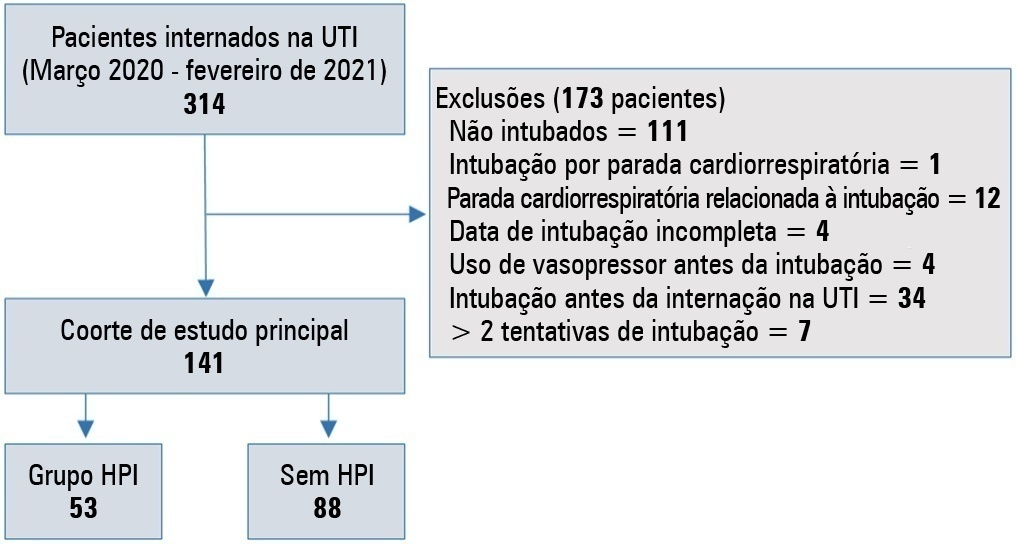
We conducted a retrospective study of 141 patients with COVID-19 who were intubated in the intensive care unit. Postintubation hypotension was defined as the need for any vasopressor dose at any time within the 60 minutes following intubation. Patients with intubation-related cardiac arrest and hypotension before intubation were excluded from the study.
Of the 141 included patients, 53 patients (37.5%) had postintubation hypotension, and 43.6% of the patients (n = 17) were female. The median age of the postintubation hypotension group was 75.0 (interquartile range: 67.0 - 84.0). In the multivariate analysis, shock index ≥ 0.90 (OR = 7.76; 95%CI 3.14 - 19.21; p < 0.001), albumin levels < 2.92g/dL (OR = 3.65; 95%CI 1.49 - 8.96; p = 0.005), and procalcitonin levels (OR = 1.07, 95%CI 1.01 - 1.15; p = 0.045) were independent risk factors for postintubation hypotension. Hospital mortality was similar in patients with postintubation hypotension and patients without postintubation hypotension (92.5% versus 85.2%; p = 0.29).
The incidence of postintubation hypotension was 37.5% in critically ill COVID-19 patients. A shock index ≥ 0.90 and albumin levels < 2.92g/dL were independently associated with postintubation hypotension. Furthermore, a shock index ≥ 0.90 may be a practical tool to predict the increased risk of postintubation hypotension in bedside scenarios before endotracheal intubation. In this study, postintubation hypotension was not associated with increased hospital mortality in COVID-19 patients.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):433-438
DOI 10.5935/0103-507X.20200073
To describe the use of neuromuscular blockade as well as other practices among Brazilian physicians in adult intensive care units.
An online national survey was designed and administered to Brazilian intensivists. Questions were selected using the Delphi method and assessed physicians’ demographic data, intensive care unit characteristics, practices regarding airway management, use of neuromuscular blockade and sedation during endotracheal intubation in the intensive care unit. As a secondary outcome, we applied a multivariate analysis to evaluate factors associated with the use of neuromuscular blockade.
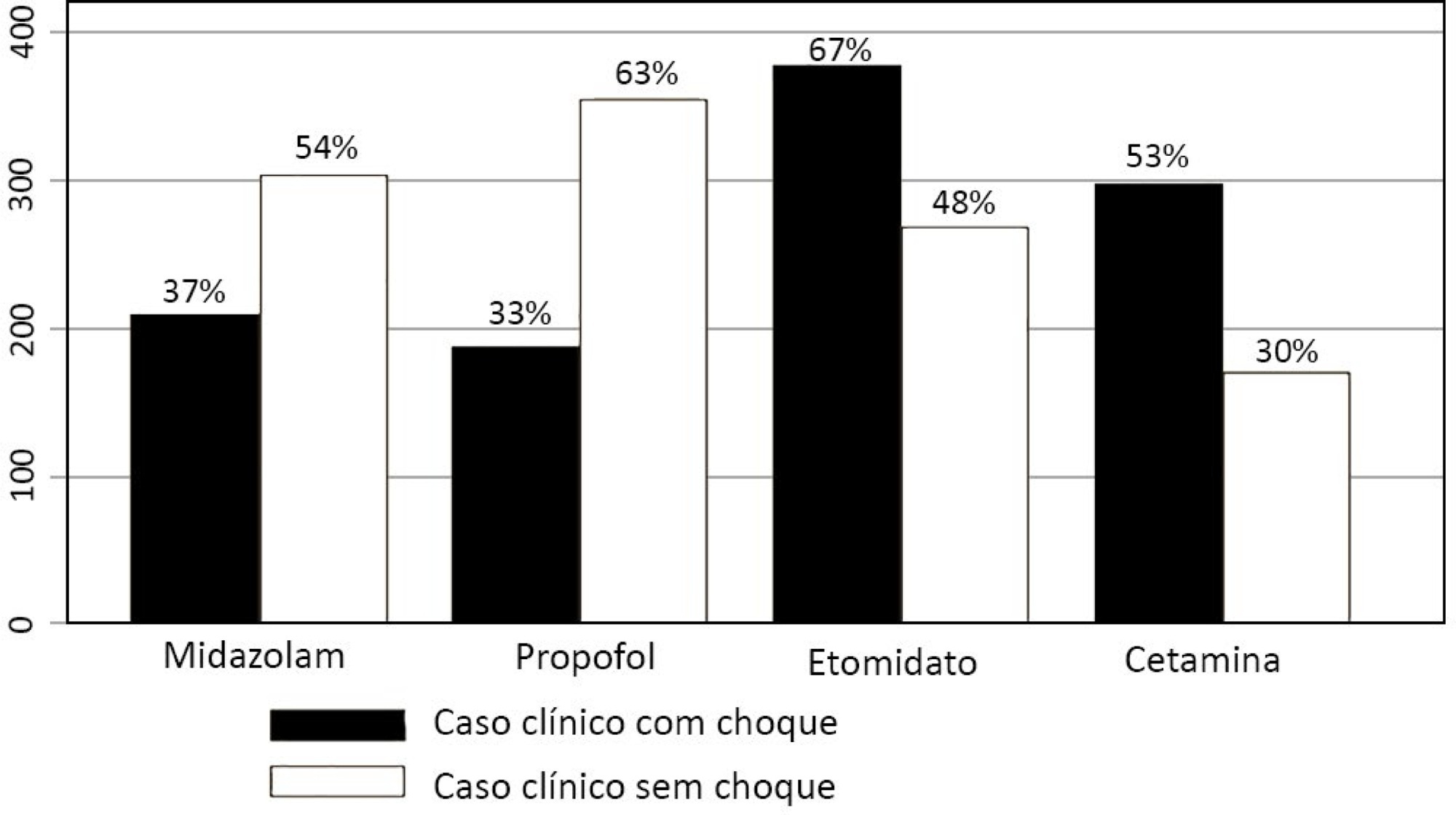
Five hundred sixty-five intensivists from all Brazilian regions responded to the questionnaire. The majority of respondents were male (65%), with a mean age of 38 ( 8.4 years, and 58.5% had a board certification in critical care. Only 40.7% of the intensivists reported the use of neuromuscular blockade during all or in more than 75% of endotracheal intubations. In the multivariate analysis, the number of intubations performed monthly and physician specialization in anesthesiology were directly associated with frequent use of neuromuscular blockade. Etomidate and ketamine were more commonly used in the clinical situation of hypotension and shock, while propofol and midazolam were more commonly prescribed in the situation of clinical stability.
The reported use of neuromuscular blockade was low among intensivists, and sedative drugs were chosen in accordance with patient hemodynamic stability. These results may help the design of future studies regarding airway management in Brazil.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):79-85
DOI 10.5935/0103-507X.20190012
We aimed to determine the incidence, risk factors, and outcomes of unplanned extubation among adult patients.
We conducted a prospective cohort study of adult intubated patients admitted to the charity wards of a government tertiary teaching hospital in the Philippines. Patients managed in both intensive care and nonintensive care settings were included. Patients were followed-up until discharge or until seven days postextubation.
The outcomes of the 191 included patients were planned extubation (35%), unplanned extubation (19%), death (39%), and discharge against advice (7%). Competing risk regression showed that male sex (Crude OR: 2.25, 95%CI: 1.10 - 4.63) and age (Crude OR 0.976, 95%CI: 0.957 - 0.996) were significant baseline factors. The night shift (Crude OR: 24.6, 95%CI: 2.87 - 211) was also consistently associated with more unplanned extubations. Among postextubation outcomes, reintubation (unplanned extubation: 61.1% versus planned extubation: 25.4%), acute respiratory failure (unplanned extubation: 38.9% versus planned extubation: 17.5%), and cardiovascular events (unplanned extubation: 8.33% versus planned extubation: 1.49%) occurred significantly more often among the unplanned extubation patients. Admission in an intensive care unit was not associated with a lower risk of unplanned extubation (Crude OR 1.15, 95%CI: 0.594 - 2.21).
Many intubated patients had unplanned extubation. Patients admitted in nonintensive care unit settings did not have significantly higher odds of unplanned extubation.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):180-187
DOI 10.5935/0103-507X.20170028
To analyze patients after cardiac surgery that needed endotracheal reintubation and identify factors associated with death and its relation with the severity scores.
Retrospective analysis of information of 1,640 patients in the postoperative period of cardiac surgery between 2007 and 2015.
The reintubation rate was 7.26%. Of those who were reintubated, 36 (30.3%) underwent coronary artery bypass surgery, 27 (22.7%) underwent valve replacement, 25 (21.0%) underwent correction of an aneurysm, and 8 (6.7%) underwent a heart transplant. Among those with comorbidities, 54 (51.9%) were hypertensive, 22 (21.2%) were diabetic, and 10 (9.6%) had lung diseases. Among those who had complications, 61 (52.6%) had pneumonia, 50 (42.4%) developed renal failure, and 49 (51.0%) had a moderate form of the transient disturbance of gas exchange. Noninvasive ventilation was performed in 53 (44.5%) patients. The death rate was 40.3%, and mortality was higher in the group that did not receive noninvasive ventilation before reintubation (53.5%). Within the reintubated patients who died, the SOFA and APACHE II values were 7.9 ± 3.0 and 16.9 ± 4.5, respectively. Most of the reintubated patients (47.5%) belonged to the high-risk group, EuroSCORE (> 6 points).
The reintubation rate was high, and it was related to worse SOFA, APACHE II and EuroSCORE scores. Mortality was higher in the group that did not receive noninvasive ventilation before reintubation.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):49-55
DOI 10.1590/S0103-507X2011000100009
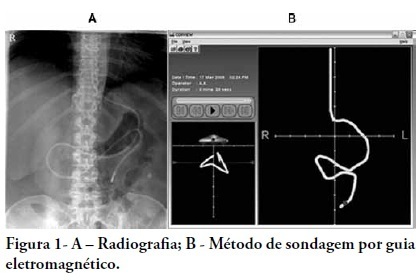
OBJECTIVE: Appropriate nutritional support is important to the outcomes of critically ill patients. However, a significant portion of these patients experience intestinal motility problems. Administration of enteral nutrition by means of tubes placed in the post-pyloric position has been suggested to improve the nutrition tolerance. The aim of this study was to compare the rate of successful post-pyloric placement using a real-time electromagnetic positioning device to the success rate using the conventional placement method. METHODS: This was a prospective, randomized and controlled study, conducted in a tertiary hospital over a period of three months. The patients were randomized to one of two groups: electromagnetically guided system group, whose patients underwent real-time monitoring of post-pyloric tube placement; or the control group, whose patients underwent tube placment using to the conventional blinded technique. The rates of successful post-pyloric placement and the procedure times were assessed and compared between the groups. RESULTS: Thirty-seven patients were enrolled, 18 in the electromagnetic group and 19 in the control group. The final tube position was evaluated using radiography. The electromagnetic guided group showed better success rates and shorter procedure times when compared to the control group. Additionally, in the electromagnetic guided group, higher pH values were found in the fluids aspirated from the probe, suggesting successful postpyloric placement. CONCLUSION: The electromagnetically guided method provided better placement accuracy than did the conventional technique.