Abstract
Rev Bras Ter Intensiva. 2019;31(4):511-520
DOI 10.5935/0103-507X.20190088
To characterize patients with chronic critical illness and identify predictors of development of chronic critical illness.
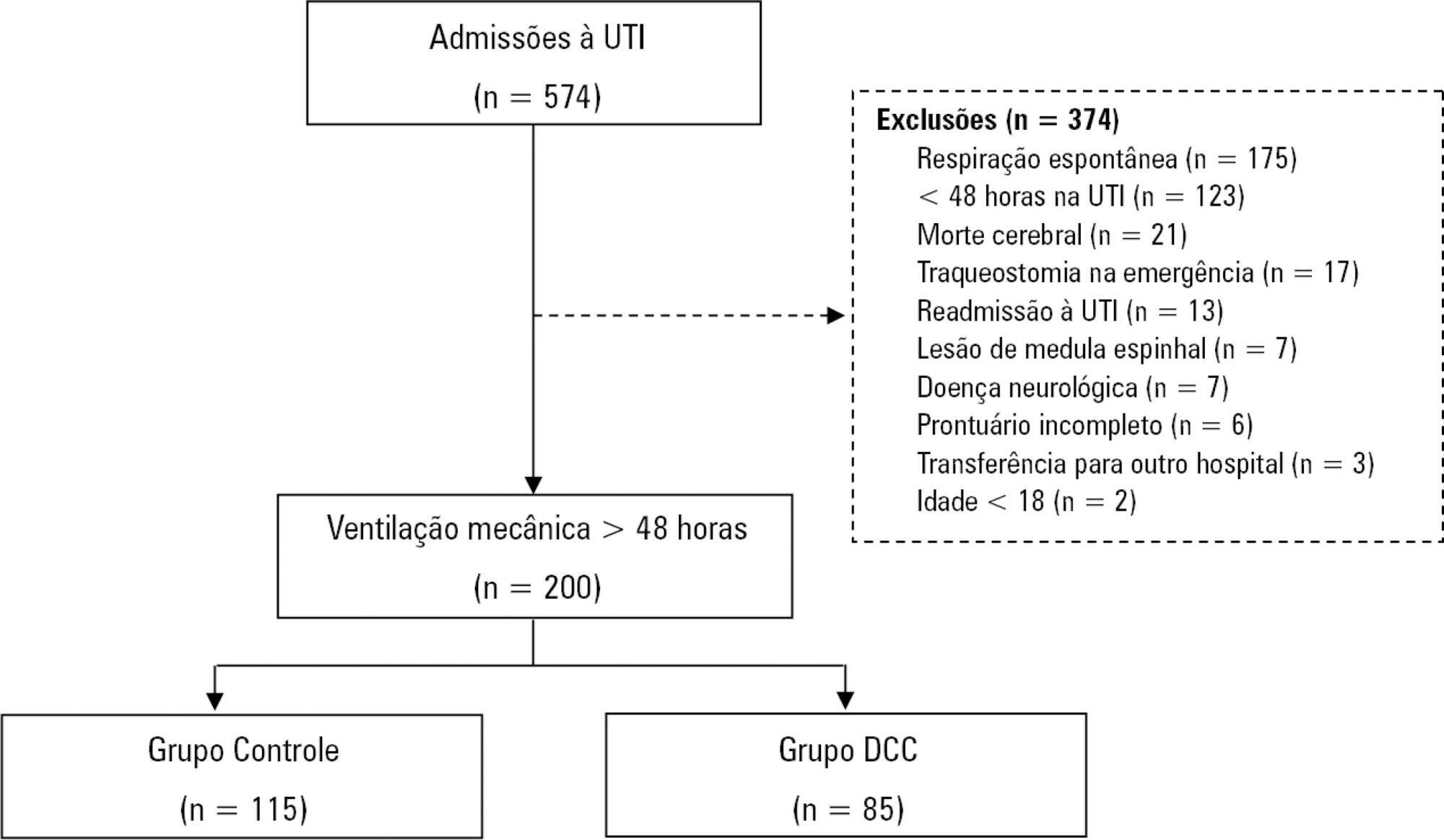
Prospective data was collected for 1 year in the intensive care unit of a general hospital in Southern Brazil. Three logistic regression models were constructed to identify factors associated with chronic critical illness.
Among the 574 subjects admitted to the intensive care unit, 200 were submitted to mechanical ventilation. Of these patients, 85 (43.5%) developed chronic critical illness, composing 14.8% of all the patients admitted to the intensive care unit. The regression model that evaluated the association of chronic critical illness with conditions present prior to intensive care unit admission identified chronic renal failure in patients undergoing hemodialysis (OR 3.57; p = 0.04) and a neurological diagnosis at hospital admission (OR 2.25; p = 0.008) as independent factors. In the model that evaluated the association of chronic critical illness with situations that occurred during intensive care unit stay, muscle weakness (OR 2.86; p = 0.01) and pressure ulcers (OR 9.54; p < 0.001) had the strongest associations. In the global multivariate analysis (that assessed previous factors and situations that occurred in the intensive care unit), hospital admission due to neurological diseases (OR 2.61; p = 0.03) and the development of pressure ulcers (OR 9.08; p < 0.001) had the strongest associations.
The incidence of chronic critical illness in this study was similar to that observed in other studies and had a strong association with the diagnosis of neurological diseases at hospital admission and chronic renal failure in patients undergoing hemodialysis, as well as complications developed during hospitalization, such as pressure ulcers and muscle weakness.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
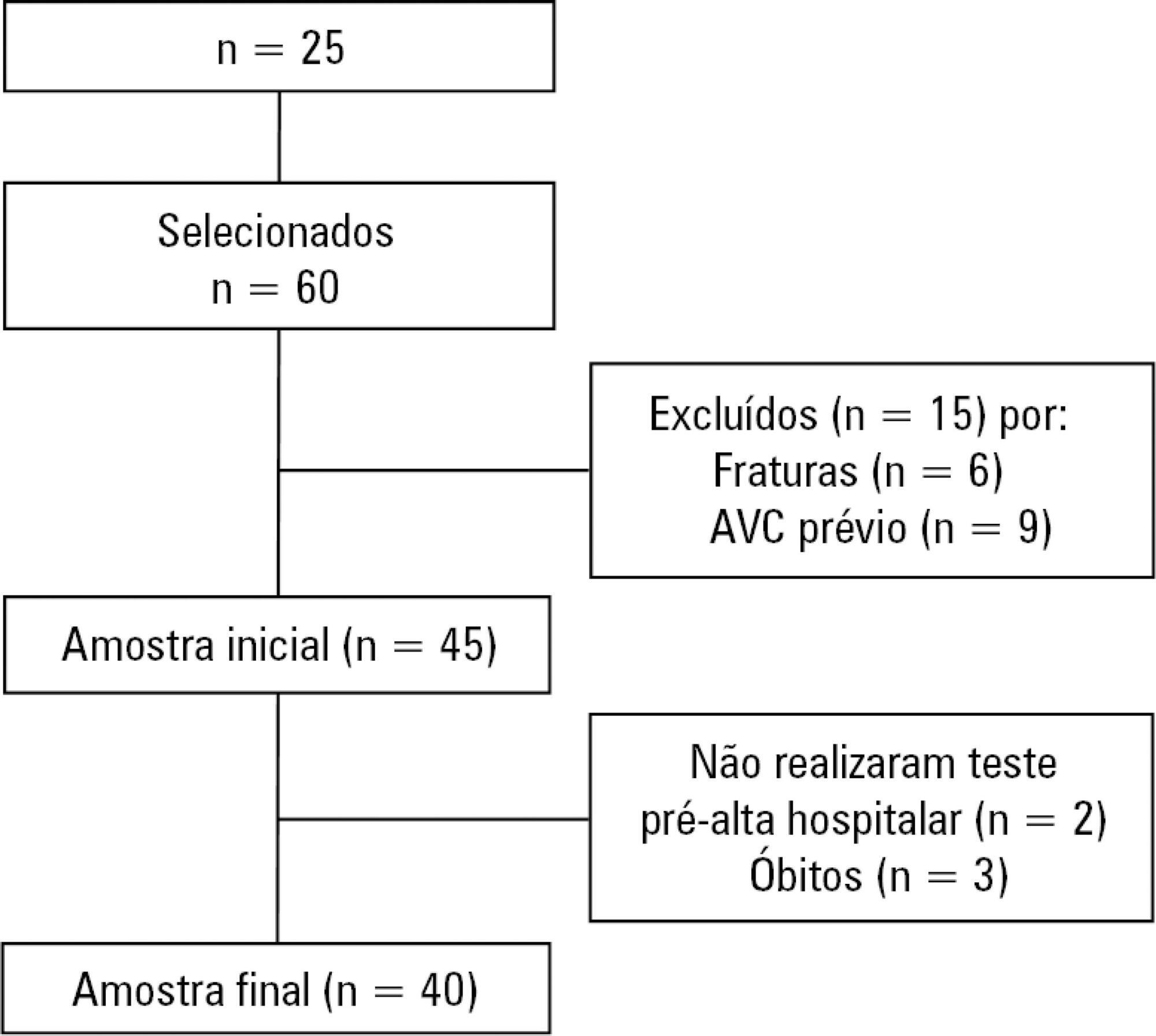
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):326-332
DOI 10.5935/0103-507X.20190041
To evaluate possible associations between nutritional risk and the clinical outcomes of critical patients admitted to an intensive care unit.
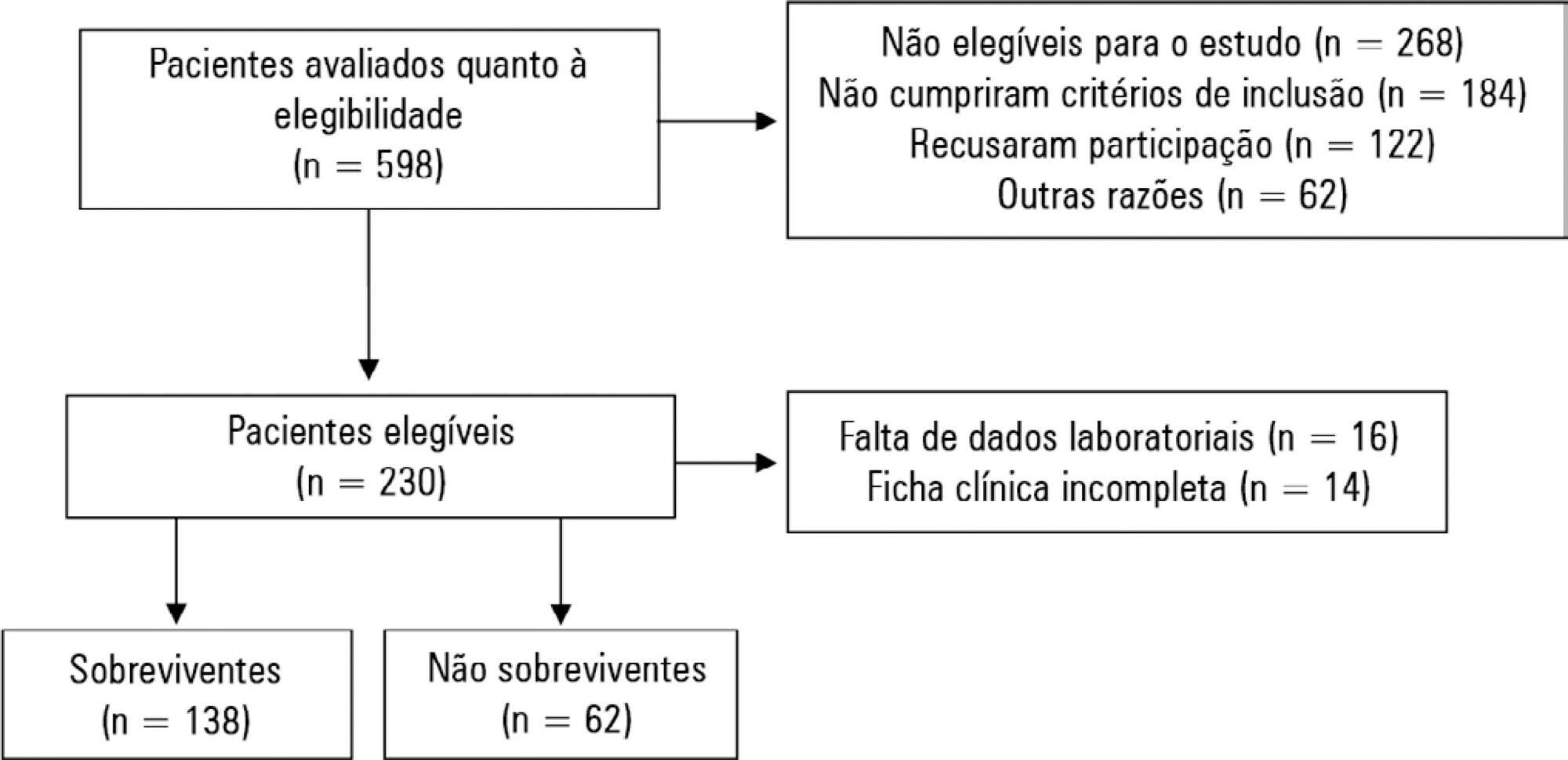
A prospective study was carried out with a cohort comprising 200 patients admitted to a university hospital intensive care unit. Nutritional risk was assessed with the NRS-2002 and NUTRIC scores. Patients with scores ≥ 5 were considered at high nutritional risk. Clinical data and outcome measures were obtained from patients' medical records. Multiple logistic regression analysis was used to calculate odds ratios and their respective 95% confidence intervals (for clinical outcomes).
This sample of critical patients had a mean age of 59.4 ± 16.5 years and 53.5% were female. The proportions at high nutritional risk according to NRS-2002 and NUTRIC were 55% and 36.5%, respectively. Multiple logistic regression models adjusted for gender and type of admission indicated that high nutritional risk assessed by the NRS-2002 was positively associated with use of mechanical ventilation (OR = 2.34; 95%CI 1.31 - 4.19; p = 0.004); presence of infection (OR = 2.21; 95%CI 1.24 - 3.94; p = 0.007), and death (OR = 1.86; 95%CI 1.01 - 3.41; p = 0.045). When evaluated by NUTRIC, nutritional risk was associated with renal replacement therapy (OR = 2.10; 95%CI 1.02 - 4.15; p = 0.040) and death (OR = 3.48; 95%CI 1.88 - 6.44; p < 0.001).
In critically ill patients, high nutritional risk was positively associated with an increased risk of clinical outcomes including hospital death.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):361-367
DOI 10.5935/0103-507X.20190059
To compare the impact of two fast-track strategies regarding the extubation time and removal of invasive mechanical ventilation in adults after cardiac surgery on clinical and hospital outcomes.
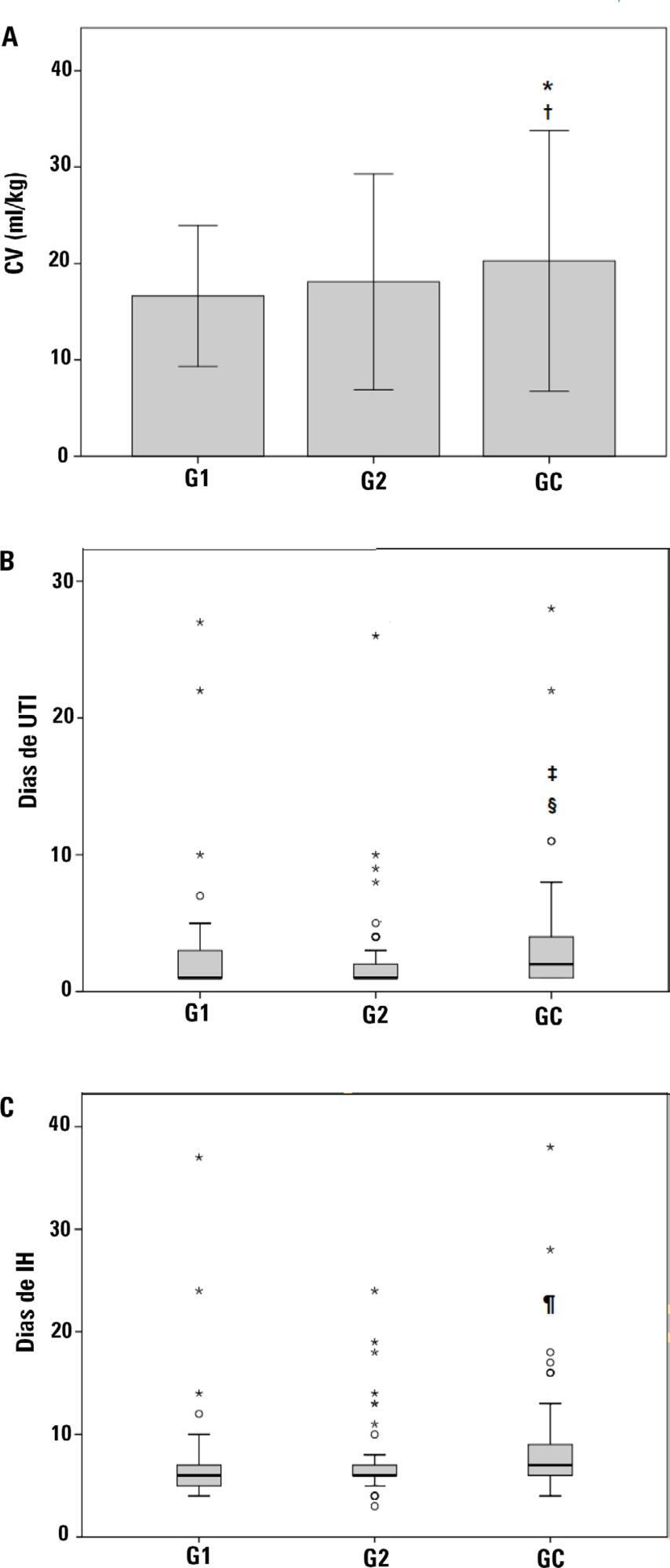
This was a retrospective cohort study with patients undergoing cardiac surgery. Patients were classified according to the extubation time as the Control Group (extubated 6 hours after admission to the intensive care unit, with a maximum mechanical ventilation time of 18 hours), Group 1 (extubated in the operating room after surgery) and Group 2 (extubated within 6 hours after admission to the intensive care unit). The primary outcomes analyzed were vital capacity on the first postoperative day, length of hospital stay, and length of stay in the intensive care unit. The secondary outcomes were reintubation, hospital-acquired pneumonia, sepsis, and death.
For the 223 patients evaluated, the vital capacity was lower in Groups 1 and 2 compared to the Control (p = 0.000 and p = 0.046, respectively). The length of stay in the intensive care unit was significantly lower in Groups 1 and 2 compared to the Control (p = 0.009 and p = 0.000, respectively), whereas the length of hospital stay was lower in Group 1 compared to the Control (p = 0.014). There was an association between extubation in the operating room (Group 1) with reintubation (p = 0.025) and postoperative complications (p = 0.038).
Patients undergoing fast-track management with extubation within 6 hours had shorter stays in the intensive care unit without increasing postoperative complications and death. Patients extubated in the operating room had a shorter hospital stay and a shorter stay in the intensive care unit but showed an increase in the frequency of reintubation and postoperative complications.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):379-385
DOI 10.5935/0103-507X.20190061
To collect data on the use of The Nutrition Risk in Critically Ill (NUTRIC) score.
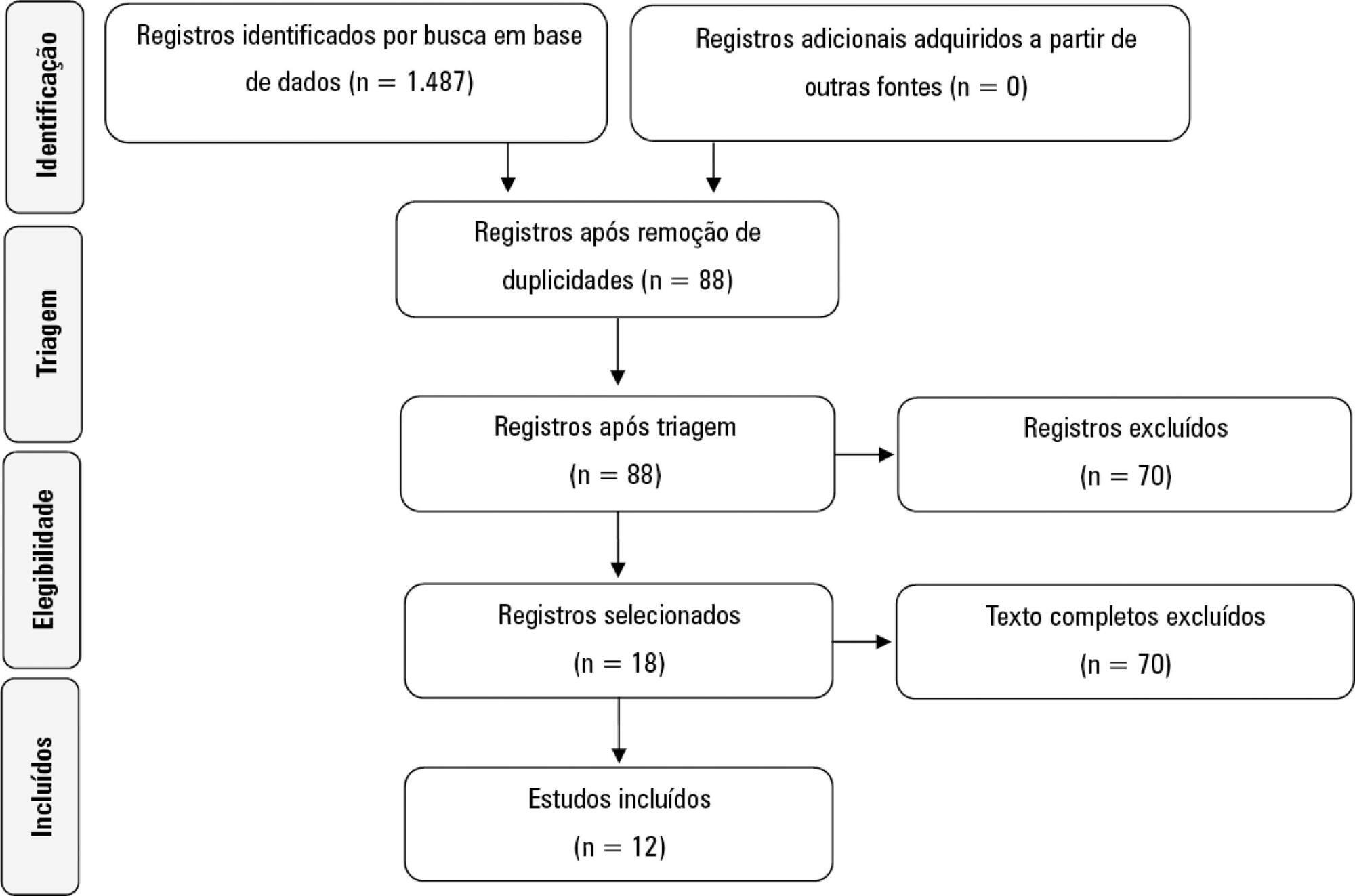
A systematic literature search was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Reviews, abstracts, dissertations, protocols and case reports were excluded from this review; to be included in the review, studies needed to specifically evaluate the NUTRIC score and to have been published in English, Spanish or Portuguese.
We included 12 (0.8%) studies from our search in this review. Ten studies (83.3%) were observational, 1 was a pilot study (8.3%) and 1 was a randomized control trial (8.3%). All of the included studies (100%) chose not to use IL-6 and considered a high nutritional risk cutoff point ≥ 5. There were 11 (91.7%) English language studies versus 1 (8.3%) Spanish language study. Mechanical ventilation and a high NUTRIC score were significantly correlated in four studies. The association between intensive care unit or hospital length of stay and nutritional high risk was significant in three studies. Seven studies found a statistically significant association between the NUTRIC score and mortality.
The NUTRIC score is related to clinical outcomes, such as length of hospital stay, and is appropriate for use in critically ill patients in intensive care units.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):386-392
DOI 10.5935/0103-507X.20190051
The improvement in cardiopulmonary resuscitation quality has reduced the mortality of individuals treated for cardiac arrest. However, survivors have a high risk of severe brain damage in cases of return of spontaneous circulation. Data suggest that cases of cardiac arrest in critically ill patients with non-shockable rhythms have only a 6% chance of returning of spontaneous circulation, and of these, only one-third recover their autonomy. Should we, therefore, opt for a procedure in which the chance of survival is minimal and the risk of hospital death or severe and definitive brain damage is approximately 70%? Is it worth discussing patient resuscitation in cases of cardiac arrest? Would this discussion bring any benefit to the patients and their family members? Advanced discussions on do-not-resuscitate are based on the ethical principle of respect for patient autonomy, as the wishes of family members and physicians often do not match those of patients. In addition to the issue of autonomy, advanced discussions can help the medical and care team anticipate future problems and, thus, better plan patient care. Our opinion is that discussions regarding the resuscitation of critically ill patients should be performed for all patients within the first 24 to 48 hours after admission to the intensive care unit.