Abstract
Rev Bras Ter Intensiva. 2013;25(4):290-296
DOI 10.5935/0103-507X.20130050
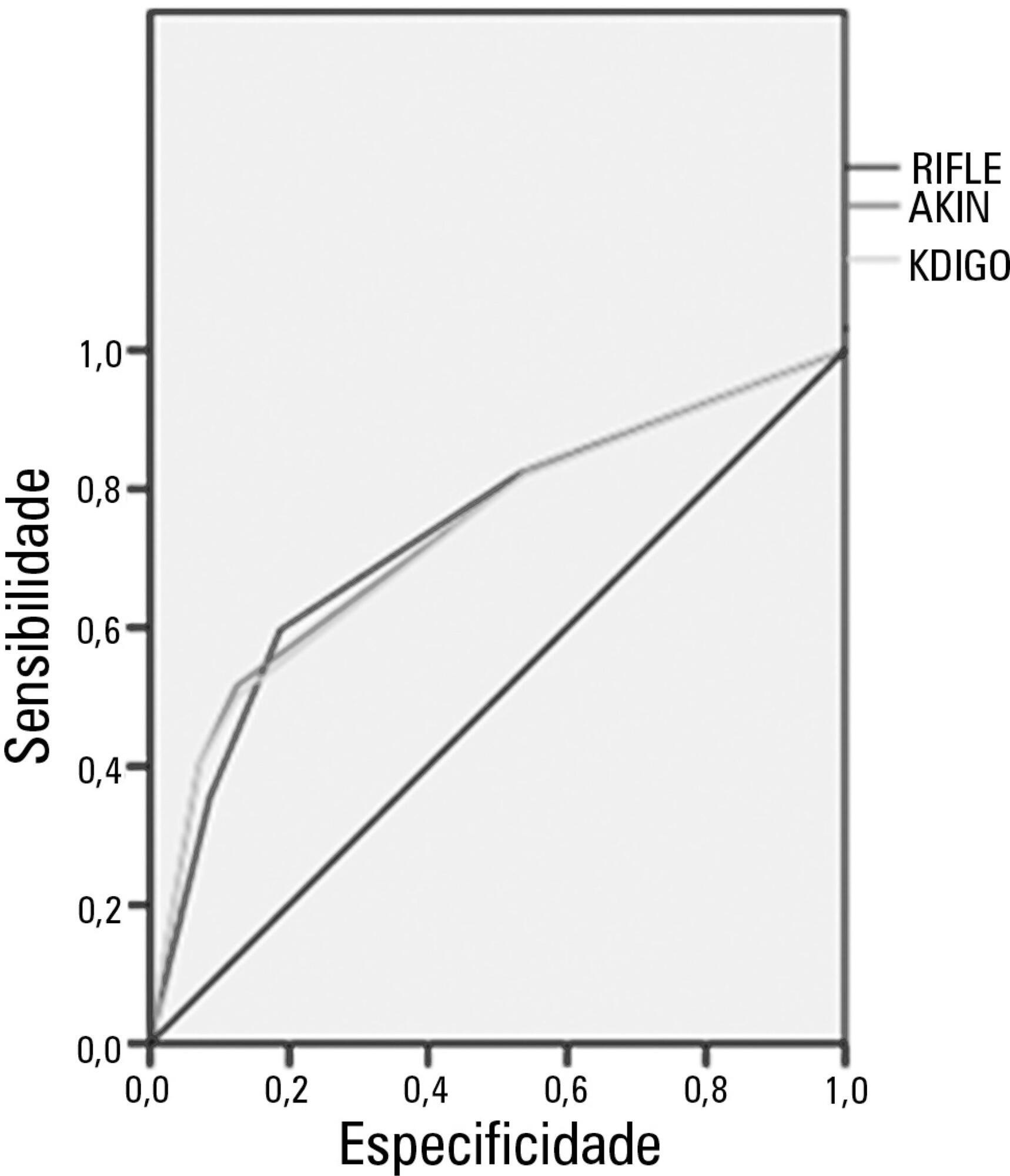
Acute kidney injury is a common complication in critically ill patients, and the RIFLE, AKIN and KDIGO criteria are used to classify these patients. The present study's aim was to compare these criteria as predictors of mortality in critically ill patients.
Prospective cohort study using medical records as the source of data. All patients admitted to the intensive care unit were included. The exclusion criteria were hospitalization for less than 24 hours and death. Patients were followed until discharge or death. Student's t test, chi-squared analysis, a multivariate logistic regression and ROC curves were used for the data analysis.
The mean patient age was 64 years old, and the majority of patients were women of African descent. According to RIFLE, the mortality rates were 17.74%, 22.58%, 24.19% and 35.48% for patients without acute kidney injury (AKI) in stages of Risk, Injury and Failure, respectively. For AKIN, the mortality rates were 17.74%, 29.03%, 12.90% and 40.32% for patients without AKI and at stage I, stage II and stage III, respectively. For KDIGO 2012, the mortality rates were 17.74%, 29.03%, 11.29% and 41.94% for patients without AKI and at stage I, stage II and stage III, respectively. All three classification systems showed similar ROC curves for mortality.
The RIFLE, AKIN and KDIGO criteria were good tools for predicting mortality in critically ill patients with no significant difference between them.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):297-305
DOI 10.5935/0103-507X.20130051
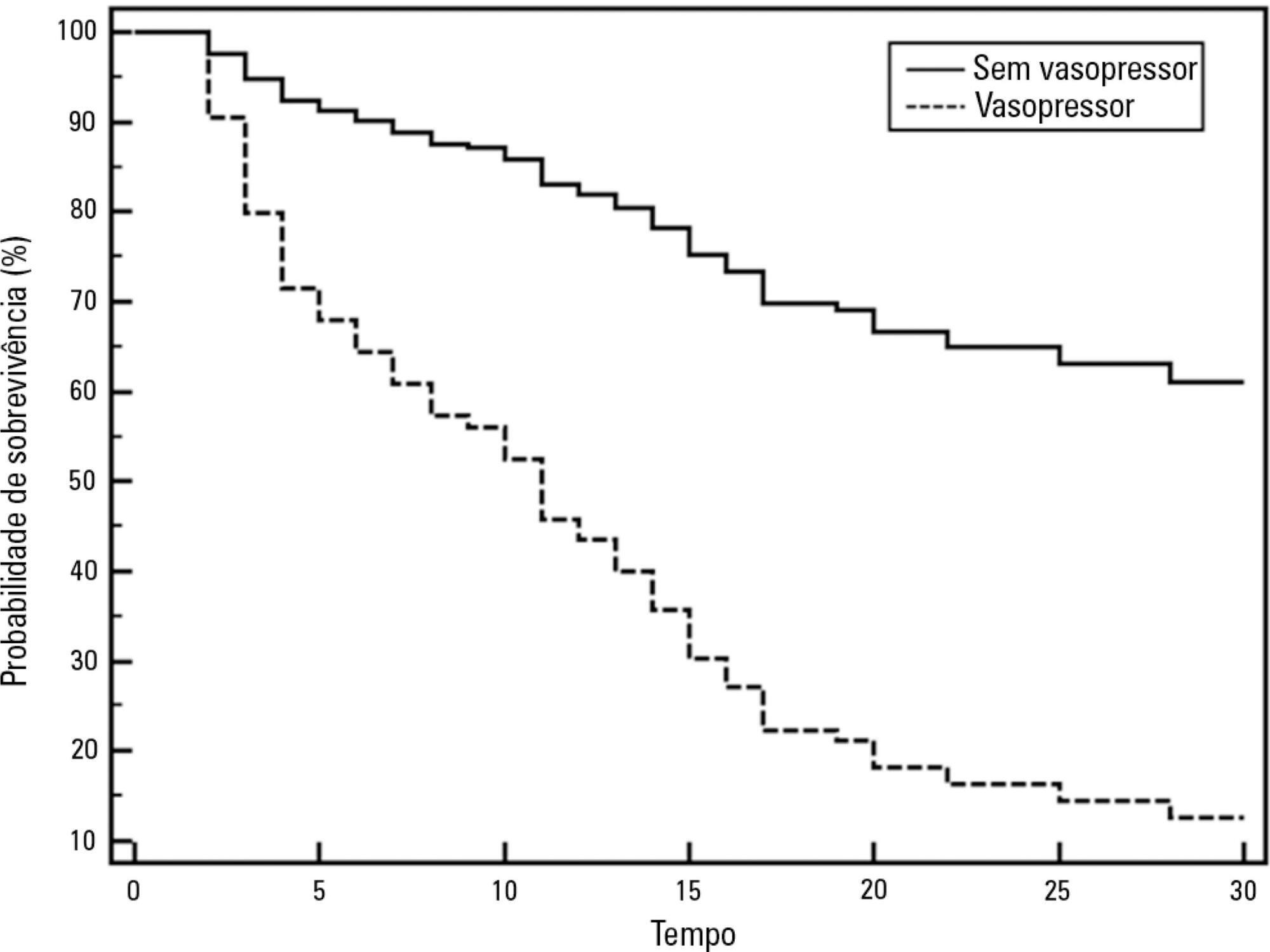
To describe a single center experience involving the administration of colistin to treat nosocomial infections caused by multidrug-resistant Gram-negative bacteria and identify factors associated with acute kidney injury and mortality.
This retrospective longitudinal study evaluates critically ill patients with infections caused by multidrug-resistant Gram-negative bacteria. All adult patients who required treatment with intravenous colistin (colistimethate sodium) from January to December 2008 were considered eligible for the study. Data include demographics, diagnosis, duration of treatment, presence of acute kidney injury and 30-day mortality.
Colistin was used to treat an infection in 109 (13.8%) of the 789 patients admitted to the intensive care unit. The 30-day mortality observed in these patients was 71.6%. Twenty-nine patients (26.6%) presented kidney injury prior to colistin treatment, and six of these patients were able to recover kidney function even during colistin treatment. Twenty-one patients (19.2%) developed acute kidney injury while taking colistin, and 11 of these patients required dialysis. The variable independently associated with the presence of acute kidney injury was the Sequential Organ Failure Assessment at the beginning of colistin treatment (OR 1.46; 95%CI 1.20-1.79; p<0.001). The factors age (OR 1.03; 95%CI 1.00-1.05; p=0.02) and vasopressor use (OR 12.48; 95%CI 4.49-34.70; p<0.001) were associated with death in the logistic-regression model.
Organ dysfunction at the beginning of colistin treatment was associated with acute kidney injury. In a small group of patients, we were able to observe an improvement of kidney function during colistin treatment. Age and vasopressor use were associated with death.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):236-245
DOI 10.1590/S0103-507X2012000300006
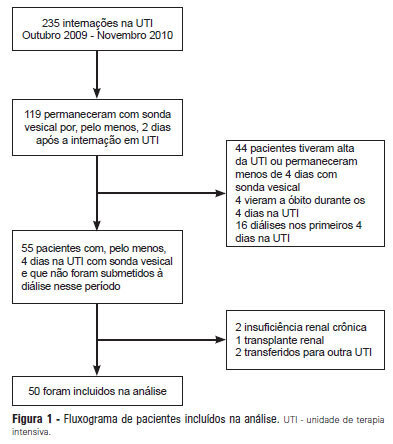
OBJECTIVE: Intensive care unit survivors and non-survivors have distinct acid-base profiles. The kidney's regulation of urinary electrolytes and the urinary strong ion difference plays a major role in acid-base homeostasis. The aim of this study was to evaluate the potential utility of daily spot urinary electrolyte measurement in acid-base and renal function monitoring. METHODS: We prospectively recorded daily plasma acid-base parameters and traditional markers of renal function in parallel with spot urinary electrolyte measurements in patients with urinary catheters admitted to our intensive care unit. Patients who remained in the intensive care unit for at least 4 days with a urinary catheter were included in the study. RESULTS: Of the 50 patients included in the study, 22% died during their intensive care unit stay. The incidence of acute kidney injury was significantly higher in non-survivors during the 4-day observation period (64% vs. 18% in survivors). Urinary chloride and sodium were lower and urinary strong ion difference was higher on day 1 in patients who developed acute kidney injury among both survivors and non-survivors. Both groups had similar urine output, although non-survivors had persistently higher urinary strong ion difference on all days. Survivors had a progressive improvement in metabolic acid-base profile due to increases in the plasma strong ion difference and decreases in weak acids. These changes were concomitant with decreases in urinary strong ion difference. In non-survivors, acid-base parameters did not significantly change during follow-up. CONCLUSIONS: Daily assessment of spot urinary electrolytes and strong ion difference are useful components of acid-base and renal function evaluations in critically ill patients, having distinct profiles between intensive care unit survivors and non-survivors.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):321-326
DOI 10.1590/S0103-507X2011000300010
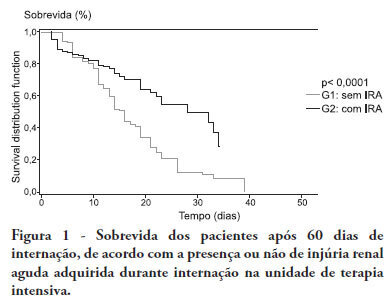
OBJECTIVE:To compare the clinical features and outcomes of patients with and without acute kidney injury in an intensive care unit of a tertiary university hospital and to identify acute kidney injury and mortality risk factors. METHODS: This was a prospective observational study of a cohort including 564 patients followed during their stay in the intensive care unit of Hospital das Clinicas da Faculdade de Medicina de Botucatu (Botucatu, São Paulo, Brazil) between May 2008 and May 2010. Patients were allocated to two different groups: with (G1) and without (G2) acute kidney injury. RESULTS: The incidence of acute kidney injury was 25.5%. The groups were different with respect to the reason for admission to the intensive care unit (sepsis, G1: 41.6% versus G2: 24.1%; P < 0.0001; neurosurgery, postoperative G1: 13.8% versus G2: 38.1%; P < 0.0001); age (G1: 56.8 ± 15.9 vs. G2: 49.8 ± 17.8 years; P < 0.0001); Acute Physiological Chronic Health Evaluation (APACHE) II score (G1: 21.9 ± 6.9 versus G2: 14.1 ± 4.6; P < 0.0001); use of mechanical ventilation (G1: 89.2% vs. G2: 69.1%; P < 0.0001) and use of vasoactive drugs (G1: 78.3% vs. G2: 56.1%; P < 0.0001). Higher rates of diabetes mellitus, congestive heart failure, chronic renal disease and use of non-steroidal anti-inflammatory drugs were more frequent in acute kidney injury patients (28.2% vs. 19.7%, P = 0.03; 23.6 vs. 11.6%, P = 0.0002; 21.5% vs. 11.5%, P < 0.0001 and 23.5% vs. 71.%, P < 0.0001, for G1 versus G2, respectively). Length of hospital stay and mortality were also higher for acute kidney injury patients (G1: 6.6 ± 2.7 days versus G2: 12.9 ±5.6 days, P < 0.0001 and G1: 62.5% versus G2: 16.4%, P < 0.0001). Multivariate analysis identified the following as risk factors for acute kidney injury: age above 55 years, APACHE II score above 16, baseline creatinine above 1.2 and use of non-steroidal anti-inflammatory drugs (odds ratio (OR) = 1.36, 95% confidence interval (95%CI): 1.22 - 1.85; OR = 1.2, 95%CI: 1.11 - 1.33; OR = 5.2, 95%CI: 2.3 - 11.6 and OR = 2.15, 95%CI: 1.1 - 4.2, respectively). Acute kidney injury was independently associated with longer hospital stay and increased mortality (OR = 1.18, 95%CI: 1.05 - 1.26 and OR = 1.24, 95%CI: 1.09 - 1.99, respectively). Analysis of the survival curve 30 days after admission showed 83.3% mortality for acute kidney injury patients and 45.2% for non-acute kidney injury patients (P < 0.0001). CONCLUSION: The incidence of acute kidney injury was high in this intensive care unit; the independent risk factors associated with acute kidney injury were age > 55 years, APACHE II > 16, baseline serum creatinine > 1.2 and use of non-steroidal anti-inflammatory drugs. Acute kidney injury is an independent risk factor for longer intensive care unit stay and mortality.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):115-123
DOI 10.1590/S0103-507X2008000200001
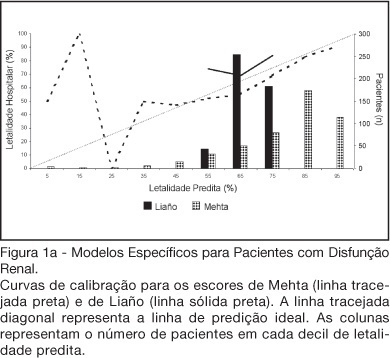
BACKGROUND AND OBJECTIVES: There is no consensus about prognostic scores for use in patients with acute kidney injury (AKI). The aim of this study was to evaluate the performance of six prognostic scores in predicting hospital mortality in patients with AKI and need for renal replacement therapy (RRT). METHODS: Prospective cohort of patients admitted to the intensive care units (ICU) of three tertiary care hospitals that required RRT for AKI over a 32-month period. Patients with end-stage renal disease and those with ICU stay < 24h were excluded. Data from the first 24h of ICU admission were used to calculate SAPS II and APACHE II scores, and data from the first 24h of RRT were used in the calculation of LOD, ODIN, Liaño and Mehta scores. Discrimination was evaluated using the area under ROC curve (AUROC) and calibration using the Hosmer-Lemeshow goodness-of-fit test. The hospital mortality was the end-point of interest. RESULTS: 467 patients were evaluated. Hospital mortality rate was 75%. Mean SAPS II and APACHE II scores were 48.5 ±11.2 and 27.4 ± 6.3 points, and median LOD score was 7 (5-8) points. Except for Mehta score (p = 0.001), calibration was appropriate in all models. However, discrimination was uniformly unsatisfactory; AUROC ranged from 0.60 for ODIN to 0.72 for SAPS II and Mehta scores. In addition, except for Mehta, all models tended to underestimate hospital mortality. CONCLUSIONS: Organ dysfunction, general and renal-specific severity-of-illness scores were inaccurate in predicting outcome in ICU patients in need for RRT.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):292-296
DOI 10.1590/S0103-507X2007000300004
BACKGROUND AND OBJECTIVES: The Acute Kidney Injury (AKI) is the most serious complication of rhabdomyolysis. In this syndrome, the delivery of heme pigment induces an injury that distinguishes itself by glomerular vasoconstriction and direct cellular toxicity with oxidative component. The renoprotection with antioxidants has demonstrated satisfactory effect. The proanthocyanidins are natural antioxidants found in the grape seed extract. The aim of this study was to evaluate the antioxidant effect of Vitis vinifera (grape seed extract) on the renal function of rats submitted to the injury by rhabdomyolysis. METHODS: Wistar rats, male, adults, weight ranging from 250-300g were used. The AKI was induced by intramuscular administration of glycerol 50%. The animals were distributed in 4 groups: Saline group (6 mL/kg of NaCl 0.9% intraperitoneal once a day), Glycerol group (6 mL/kg) of intramuscular glycerol each femoral region received 3 mL/kg of glycerol, once a day), Vitis vinifera group (3 mg/kg/day v.o by 5 days) and Glycerol + Vitis vinifera by 5 days before glycerol). RESULTS: Renal function (RF-creatinine clearance) and oxidative profile (urinary peroxides-FOX-2 and MDA-TBARS) were evaluted. The Glycerol group treated with Vitis vinifera has shown improvements in RF and reduction levels of lipid peroxidation. CONCLUSION: The results of this study have confirmed the antioxidant protection of Vitis vinifera in AKI induced by glycerol.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)