Abstract
Rev Bras Ter Intensiva. 2018;30(2):153-159
DOI 10.5935/0103-507X.20180030
To investigate prognostic factors among critically ill patients with community-acquired bacterial meningitis and acute kidney injury.
A retrospective study including patients admitted to a tertiary infectious disease hospital in Fortaleza, Brazil diagnosed with community-acquired bacterial meningitis complicated with acute kidney injury. Factors associated with death, mechanical ventilation and use of vasopressors were investigated.
Forty-one patients were included, with a mean age of 41.6 ± 15.5 years; 56% were males. Mean time between intensive care unit admission and acute kidney injury diagnosis was 5.8 ± 10.6 days. Overall mortality was 53.7%. According to KDIGO criteria, 10 patients were classified as stage 1 (24.4%), 18 as stage 2 (43.9%) and 13 as stage 3 (31.7%). KDIGO 3 significantly increased mortality (OR = 6.67; 95%CI = 1.23 - 36.23; p = 0.028). Thrombocytopenia was not associated with higher mortality, but it was a risk factor for KDIGO 3 (OR = 5.67; 95%CI = 1.25 - 25.61; p = 0.024) and for mechanical ventilation (OR = 6.25; 95%CI = 1.33 - 29.37; p = 0.02). Patients who needed mechanical ventilation by 48 hours from acute kidney injury diagnosis had higher urea (44.6 versus 74mg/dL, p = 0.039) and sodium (138.6 versus 144.1mEq/L; p = 0.036).
Mortality among critically ill patients with community-acquired bacterial meningitis and acute kidney injury is high. Acute kidney injury severity was associated with even higher mortality. Thrombocytopenia was associated with severer acute kidney injury. Higher urea was an earlier predictor of severer acute kidney injury than was creatinine.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):373-381
DOI 10.5935/0103-507X.20170051
Novel biomarkers can be suitable for early acute kidney injury diagnosis and the prediction of the need for dialysis. It remains unclear whether such biomarkers may also play a role in the prediction of recovery after established acute kidney injury or in aiding the decision of when to stop renal support therapy. PubMed, Web of Science and Google Scholar were searched for studies that reported on the epidemiology of renal recovery after acute kidney injury, the risk factors of recovery versus non-recovery after acute kidney injury, and potential biomarkers of acute kidney injury recovery. The reference lists of these articles and relevant review articles were also reviewed. Final references were selected for inclusion in the review based on their relevance. New biomarkers exhibited a potential role in the early diagnosis of acute kidney injury recovery. Urine HGF, IGFBP-7, TIMP-2 and NGAL may improve our ability to predict the odds and timing of recovery and eventually renal support withdrawal. Acute kidney injury recovery requires more study, and its definition needs to be standardized to allow for better and more powerful research on biomarkers because some of them show potential for the prediction of acute kidney injury recovery.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):70-77
DOI 10.5935/0103-507X.20160015
Identify prognostic factors related to mortality and non-recovery of renal function.
A prospective single-center study was conducted at the intensive care medicine department of a university hospital between 2012 and 2015. Patients with acute kidney injury receiving continuous renal replacement therapy were included in the study. Clinical and analytical parameters were collected, and the reasons for initiation and discontinuation of renal replacement therapy were examined.
A total of 41 patients were included in the study, of whom 43.9% had sepsis. The median Simplified Acute Physiology Score II (SAPSII) was 56 and the mortality was 53.7%, with a predicted mortality of 59.8%. The etiology of acute kidney injury was often multifactorial (56.1%). Survivors had lower cumulative fluid balance (median = 3,600mL, interquartile range [IQR] = 1,175 - 8,025) than non-survivors (median = 12,000mL, IQR = 6,625 - 17,875; p = 0.004). Patients who recovered renal function (median = 51.0, IQR = 45.8 - 56.2) had lower SAPS II than those who do not recover renal function (median = 73, IQR = 54 - 85; p = 0.005) as well as lower fluid balance (median = 3,850, IQR = 1,425 - 8,025 versus median = 11,500, IQR = 6,625 - 16,275; p = 0.004).
SAPS II at admission and cumulative fluid balance during renal support therapy were risk factors for mortality and non-recovery of renal function among critically ill patients with acute kidney injury needing renal replacement therapy.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):384-391
DOI 10.5935/0103-507X.20140059
This study aimed to describe and compare the characteristics and clinical outcomes of patients with septic and non-septic acute kidney injury.
This study evaluated an open cohort of 117 critically ill patients with acute kidney injury who were consecutively admitted to an intensive care unit, excluding patients with a history of advanced-stage chronic kidney disease, kidney transplantation, hospitalization or death in a period shorter than 24 hours. The presence of sepsis and in-hospital death were the exposure and primary variables in this study, respectively. A confounding analysis was performed using logistic regression.
No significant differences were found between the mean ages of the groups with septic and non-septic acute kidney injury [65.30±21.27 years versus 66.35±12.82 years, respectively; p=0.75]. In the septic and non-septic acute kidney injury groups, a predominance of females (57.4% versus 52.4%, respectively; p=0.49) and Afro-descendants (81.5% versus 76.2%, respectively; p=0.49) was observed. Compared with the non-septic patients, the patients with sepsis had a higher mean Acute Physiology and Chronic Health Evaluation II score [21.73±7.26 versus 15.75±5.98; p<0.001)] and a higher mean water balance (p=0.001). Arterial hypertension (p=0.01) and heart failure (p<0.001) were more common in the non-septic patients. Septic acute kidney injury was associated with a greater number of patients who required dialysis (p=0.001) and a greater number of deaths (p<0.001); however, renal function recovery was more common in this group (p=0.01). Sepsis (OR: 3.88; 95%CI: 1.51-10.00) and an Acute Physiology and Chronic Health Evaluation II score >18.5 (OR: 9.77; 95%CI: 3.73-25.58) were associated with death in the multivariate analysis.
Sepsis was an independent predictor of death. Significant differences were found between the characteristics and clinical outcomes of patients with septic versus non-septic acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):347-354
DOI 10.5935/0103-507X.20140053
To assess the diagnostic and prognostic efficacy of urine neutrophil gelatinase-associated lipocalin in patients admitted to an intensive care unit.
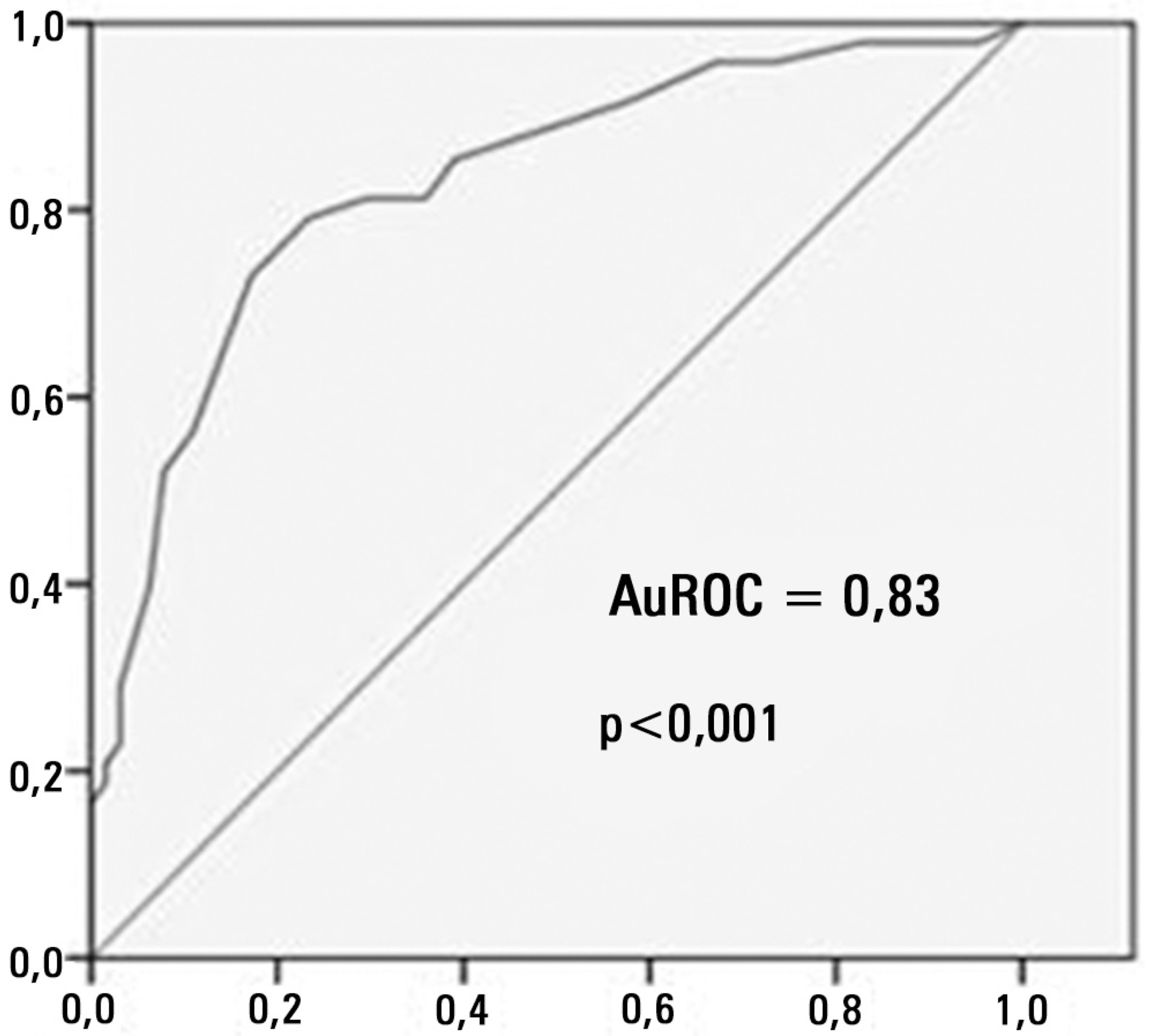
Longitudinal, prospective cohort study conducted in a cardiology intensive care unit. The participants were divided into groups with and without acute kidney injury and were followed from admission to the intensive care unit until hospital discharge or death. Serum creatinine, urine output and urine neutrophil gelatinase-associated lipocalin were measured 24 and 48 hours after admission.
A total of 83 patients admitted to the intensive care unit for clinical reasons were assessed, most being male (57.8%). The participants were divided into groups without acute kidney injury (N=18), with acute kidney injury (N=28) and with severe acute kidney injury (N=37). Chronic diseases, mechanical ventilation and renal replacement therapy were more common in the groups with acute kidney injury and severe acute kidney injury, and those groups exhibited longer intensive care unit stay and hospital stay and higher mortality. Serum creatinine did not change significantly in the group with acute kidney injury within the first 24 hours of admission to the intensive care unit, although, urine neutrophil gelatinase-associated lipocalin was high in the groups with acute kidney injury and severe acute kidney injury (p<0.001). Increased urine neutrophil gelatinase-associated lipocalin was associated with death.
An increase in urine neutrophil gelatinase-associated lipocalin precedes variations in serum creatinine in patients with acute kidney injury and may be associated with death.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):143-147
DOI 10.5935/0103-507X.20140021
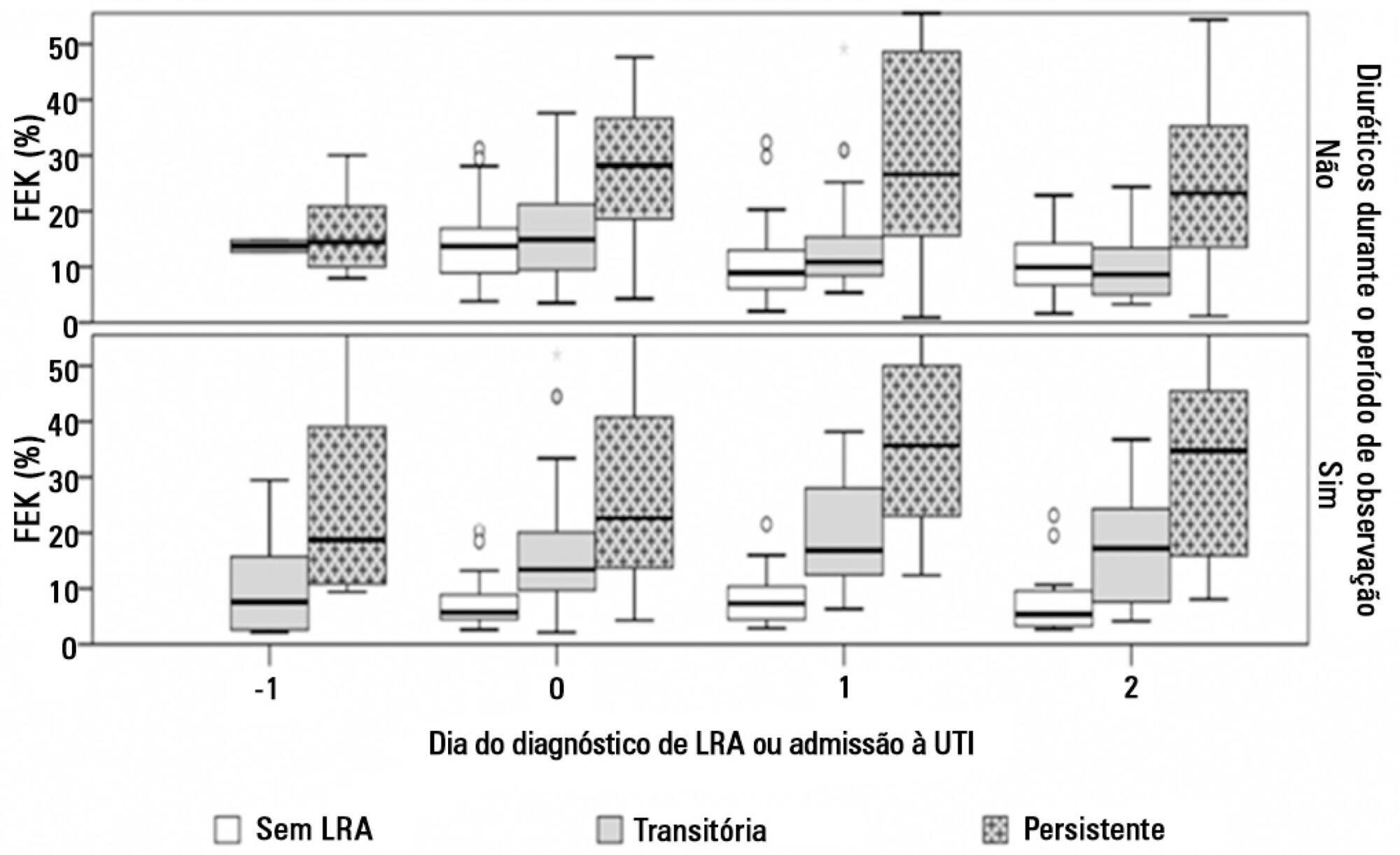
To evaluate the behavior of fractional excretion of potassium in the course of acute kidney injury in critically ill patients.
As part of a larger study in which we have evaluated blood and urinary parameters in the course of acute kidney injury, 168 patients were included. Blood and urine samples were collected daily until the removal of the urinary catheter or the initiation of renal replacement therapy. We describe the evolution of fractional excretion of potassium based on whether acute kidney injury was diagnosed, its duration (transient or persistent) and its severity (creatinine-based Acute Kidney Injury Network - AKIN stage). The diagnostic performance of fractional excretion of potassium in predicting the duration of acute kidney injury and the need for renal replacement therapy on the day of acute kidney injury diagnosis was also evaluated.
Fractional excretion of potassium was significantly higher in persistent acute kidney injury compared to transient acute kidney injury on the day of acute kidney injury diagnosis (24.8 vs. 13.8%, p<0.001). Both groups had the median fractional excretion of potassium increasing in the two days preceding the acute kidney injury diagnosis. Patients without acute kidney injury had stable low fractional excretion of potassium values. The fractional excretion of potassium was fairly accurate in predicting persistent acute kidney injury (area under the curve: 0.712; 95% confidence interval: 0.614-0.811; p<0.001) on the day of acute kidney injury diagnosis. The area under the curve was 0.663 (95% confidence interval: 0.523-0.803; p=0.03) for renal replacement therapy. The fractional excretion of potassium increased with maximum AKIN stage reached, in both transient and persistent acute kidney injury.
Sequential fractional excretion of potassium assessment appears to be useful in critically ill patients at risk for acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):130-136
DOI 10.5935/0103-507X.20130024
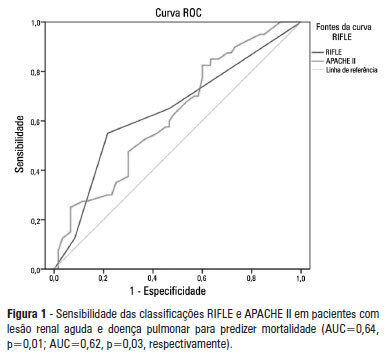
OBJECTIVE: To examine the factors associated with acute kidney injury and outcome in patients with lung disease. METHODS: A prospective study was conducted with 100 consecutive patients admitted to a respiratory intensive care unit in Fortaleza (CE), Brazil. The risk factors for acute kidney injury and mortality were investigated in a group of patients with lung diseases. RESULTS: The mean age of the study population was 57 years, and 50% were male. The incidence of acute kidney injury was higher in patients with PaO2/FiO2<200 mmHg (54% versus 23.7%; p=0.02). Death was observed in 40 cases and the rate of mortality of the acute kidney injury group was higher (62.8% versus 27.6%; p=0.01). The independent factor that was found to be associated with acute kidney injury was PaO2/FiO2<200 mmHg (p=0.01), and the independent risk factors for death were PEEP at admission (OR: 3.6; 95%CI: 1.3-9.6; p=0.009) and need for hemodialysis (OR: 7.9; 95%CI: 2.2-28.3; p=0.001). CONCLUSION: There was a higher mortality rate in the acute kidney injury group. Increased mortality was associated with mechanical ventilation, high PEEP, urea and need for dialysis. Further studies must be performed to better establish the relationship between kidney and lung injury and its impact on patient outcome.