Abstract
Rev Bras Ter Intensiva. 2019;31(4):511-520
DOI 10.5935/0103-507X.20190088
To characterize patients with chronic critical illness and identify predictors of development of chronic critical illness.
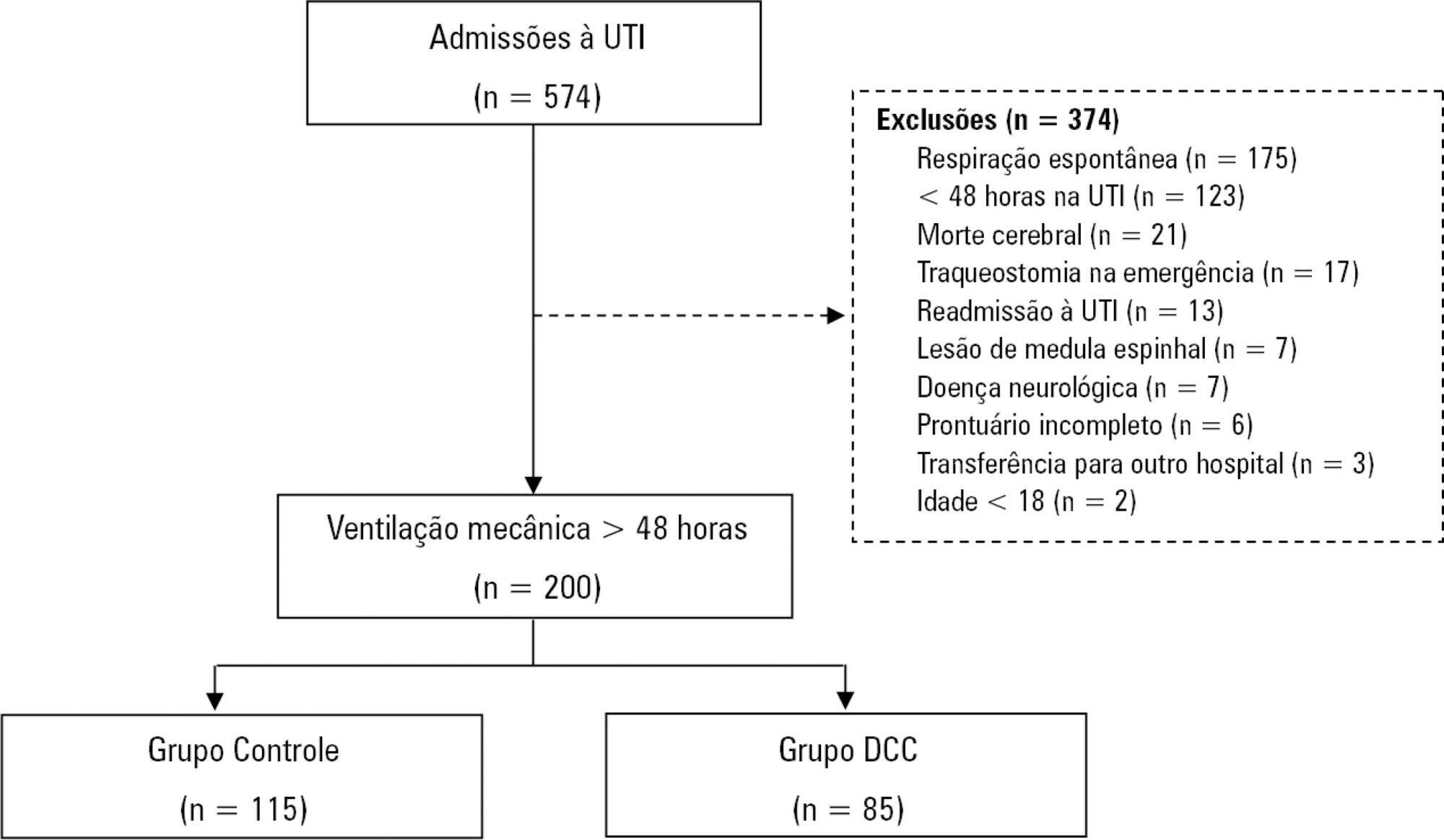
Prospective data was collected for 1 year in the intensive care unit of a general hospital in Southern Brazil. Three logistic regression models were constructed to identify factors associated with chronic critical illness.
Among the 574 subjects admitted to the intensive care unit, 200 were submitted to mechanical ventilation. Of these patients, 85 (43.5%) developed chronic critical illness, composing 14.8% of all the patients admitted to the intensive care unit. The regression model that evaluated the association of chronic critical illness with conditions present prior to intensive care unit admission identified chronic renal failure in patients undergoing hemodialysis (OR 3.57; p = 0.04) and a neurological diagnosis at hospital admission (OR 2.25; p = 0.008) as independent factors. In the model that evaluated the association of chronic critical illness with situations that occurred during intensive care unit stay, muscle weakness (OR 2.86; p = 0.01) and pressure ulcers (OR 9.54; p < 0.001) had the strongest associations. In the global multivariate analysis (that assessed previous factors and situations that occurred in the intensive care unit), hospital admission due to neurological diseases (OR 2.61; p = 0.03) and the development of pressure ulcers (OR 9.08; p < 0.001) had the strongest associations.
The incidence of chronic critical illness in this study was similar to that observed in other studies and had a strong association with the diagnosis of neurological diseases at hospital admission and chronic renal failure in patients undergoing hemodialysis, as well as complications developed during hospitalization, such as pressure ulcers and muscle weakness.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):521-528
DOI 10.5935/0103-507X.20190065
To compare the measurement properties (internal consistency, intra and interrater reliability, construct validity, and ceiling and floor effects) of the Functional Status Score for the ICU (FSS-ICU) and the Functional Independence Measure (FIM-motor domain).
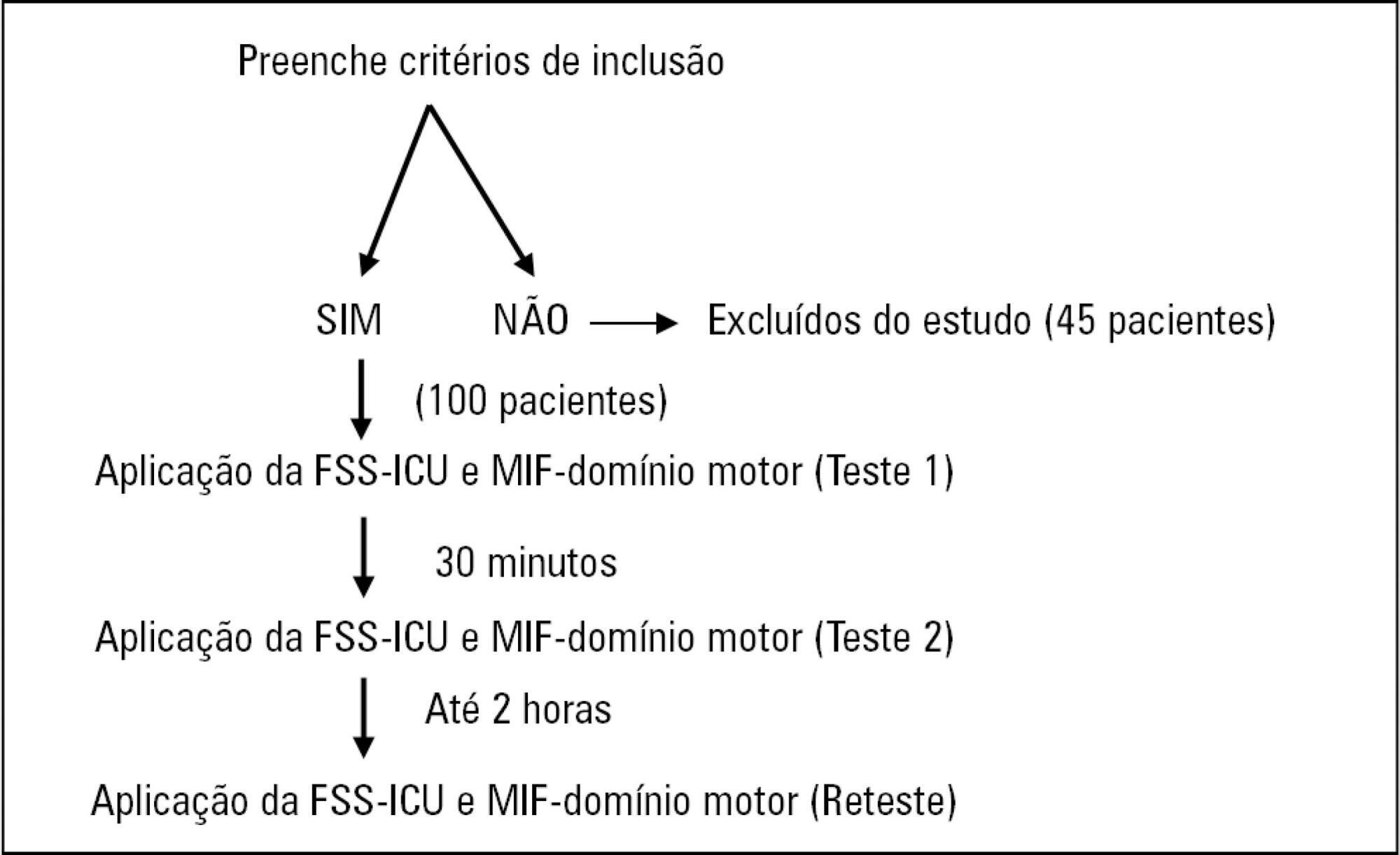
In this study of measurement properties, the FSS-ICU and FIM were applied to 100 patients (72.1 ± 15.9 years; 53% male; Sequential Organ Failure Assessment = 11.0 ± 3.5 points, Simplified Acute Physiology Score 3 = 50.2 ± 16.8 points) in an intensive care unit at baseline and after 2 hours by physiotherapist 1 (test and retest) and 30 minutes after baseline by physiotherapist 2. The measurement properties evaluated were internal consistency (Cronbach's alpha), intra- and interrater reliability (intraclass correlation coefficient), agreement (standard error of measurement) and minimum detectable change at a 90% confidence level, ceiling and floor effects (frequency of maximum and minimum scores) and construct validity (Pearson's correlation).
The FSS-ICU and FIM presented adequate internal consistency (Cronbach's alpha, FSS-ICU = 0.95 and FIM = 0.86), intra-and interrater reliability for overall FSS-ICU and FIM score (ICC > 0.75), agreement (minimum detectable change at a 90% confidence level: FSS-ICU and FIM = 1.0 point; standard error of measurement: FSS-ICU = 2% and FIM = 1%) and construct validity (r = 0.94; p < 0.001). However, the FSS-ICU and FIM presented ceiling effects (maximum score for 16% of patients for the FSS-ICU and 18% for the FIM).
The FSS-ICU and FIM present adequate measurement properties to assess functionality in critically ill patients, although they present ceiling effects.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):529-535
DOI 10.5935/0103-507X.20190066
To measure and compare the functionality of patients after discharge from the intensive care unit and at the time of hospital discharge.
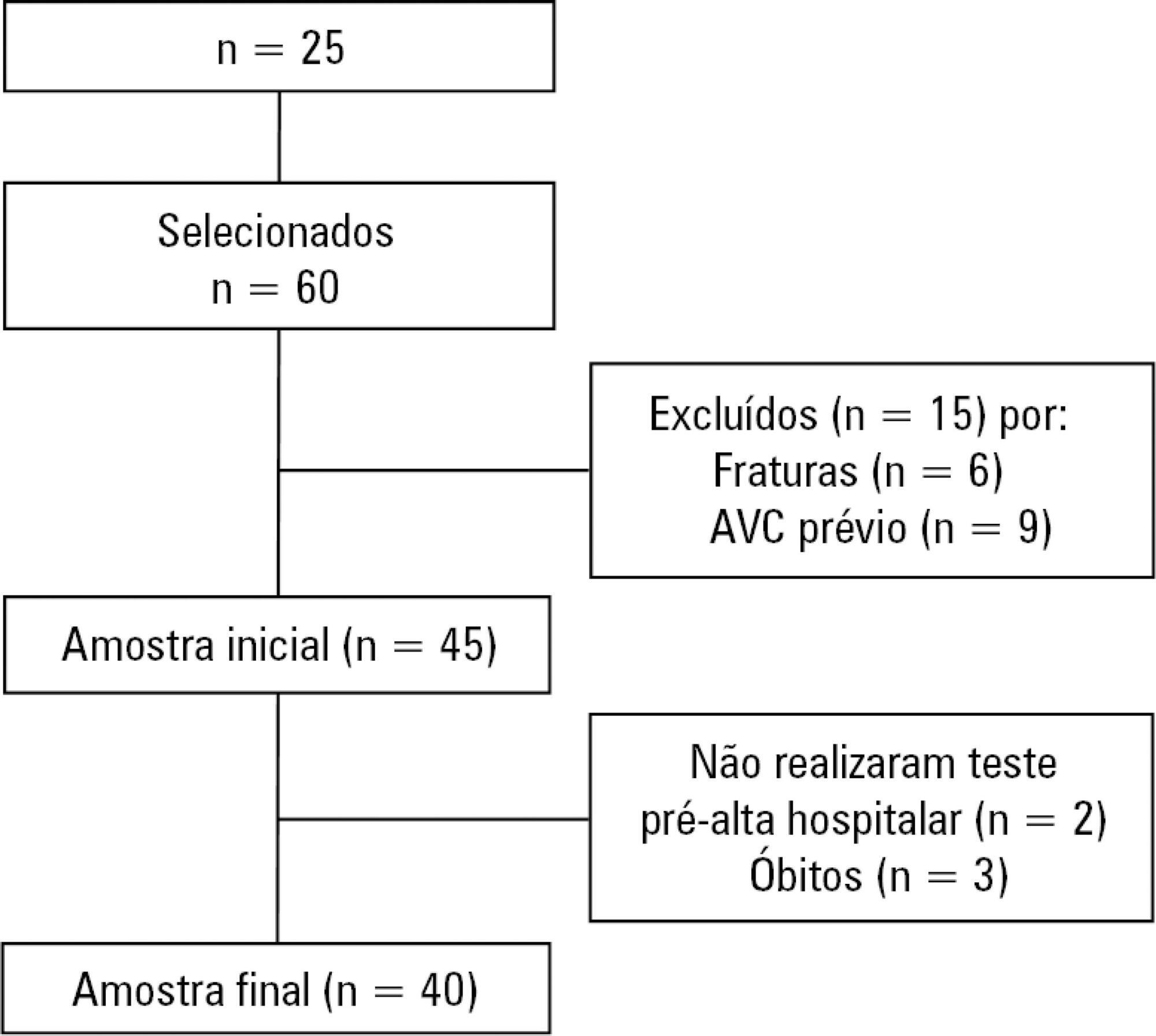
Quantitative study of a prospective cohort performed between August of 2016 and December of 2017 at a university hospital. A 10-meter walk test was performed at 2 timepoints: after discharge from the intensive care unit and prior to hospital discharge. The data were analyzed using Student's t-test and Pearson or Spearman correlation. Statistical Package for Social Science (SPSS) version 21.0 was used for the analysis, and p ≤ 0.05 was adopted as the level of significance.
Forty patients, with a mean age of 57.1 ± 12.2 years and with a predominance of males (60%), were evaluated. For the post-intensive care unit test, a mean speed of 0.48m/s was observed, and for the pre-hospital discharge test, there was an increase to 0.71m/s, evidencing functional evolution during the hospital stay (p < 0.001).
There was significant improvement in walking speed at the time of hospital discharge when compared to the walking speed at the time of intensive care unit discharge.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):282-288
DOI 10.5935/0103-507X.20190053
To describe the epidemiological profile of victims of cardiac arrest assisted using a nontransporting emergency medical service vehicle and to determine whether these patients met the criteria for the use of extracorporeal membrane oxygenation.
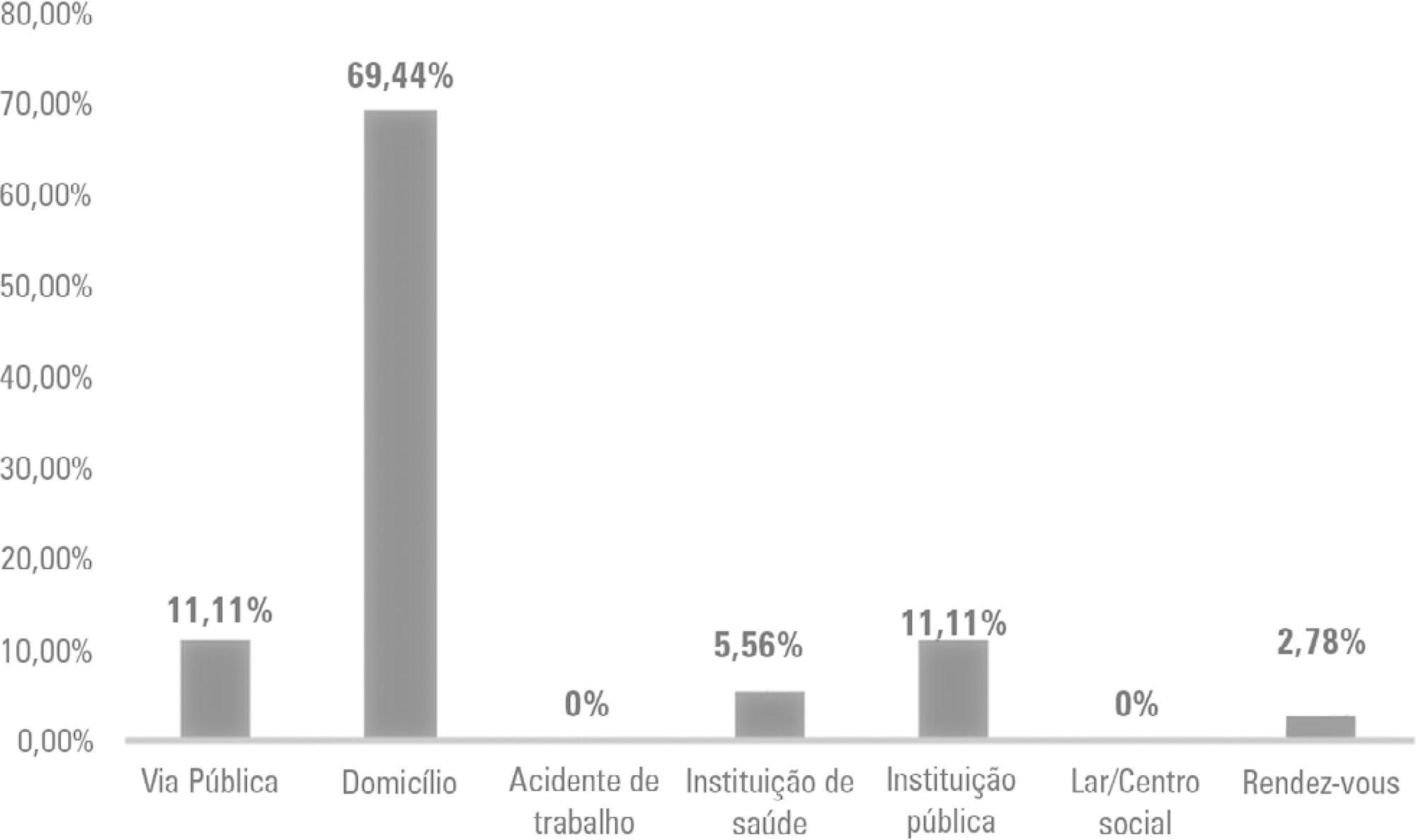
This study employed a retrospective, cohort, descriptive, and exploratory design. Data were collected in January 2018 in northern Portugal by consulting the records of nontransporting emergency medical service vehicles that provided assistance between 2012 and 2016. An observation grid was prepared that was supported by the instrument used for collecting data from the national registry of out-ofhospital cardiac arrests.
After applying the inclusion criteria, the sample consisted of 36 victims. Extracorporeal membrane oxygenation could have been applied to 24 victims during the period analyzed, which might have increased the odds for transplantation, survival, or both, for either the victim or other individuals.
Nontransporting emergency medical service vehicles have the potential for inclusion in the extracorporeal membrane oxygenation network of the study area.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):289-295
DOI 10.5935/0103-507X.20190052
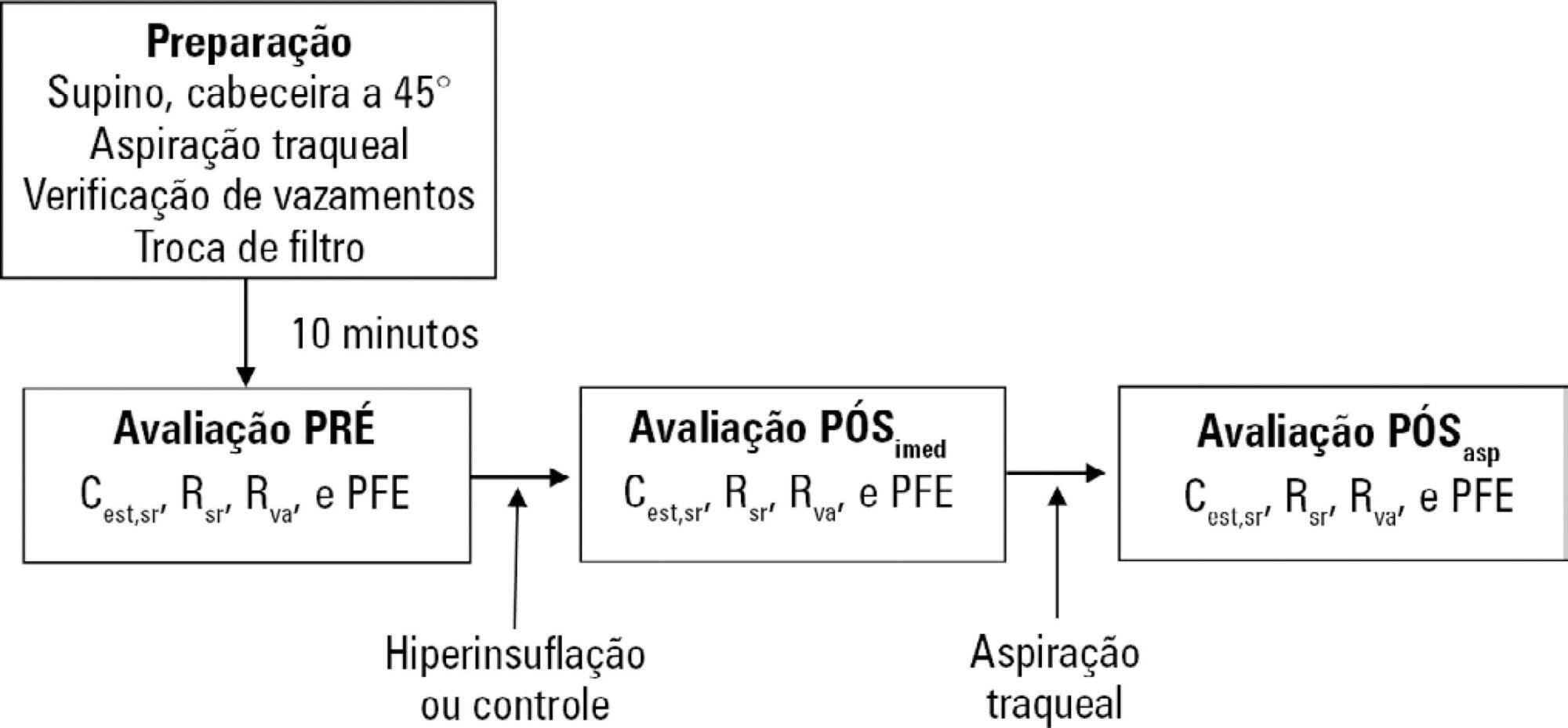
To evaluate the effects of ventilator hyperinflation on respiratory mechanics.
A randomized crossover clinical trial was conducted with 38 mechanically ventilated patients with pulmonary infection. The order of the hyperinflation and control (without changes in the parameters) conditions was randomized. Hyperinflation was performed for 5 minutes in pressure-controlled ventilation mode, with progressive increases of 5cmH2O until a maximum pressure of 35cmH2O was reached, maintaining positive end expiratory pressure. After 35cmH2O was reached, the inspiratory time and respiratory rate were adjusted so that the inspiratory and expiratory flows reached baseline levels. Measurements of static compliance, total resistance and airway resistance, and peak expiratory flow were evaluated before the technique, immediately after the technique and after aspiration. Two-way analysis of variance for repeated measures was used with Tukey's post hoc test, and p < 0.05 was considered significant.
Ventilator hyperinflation increased static compliance, which remained at the same level after aspiration (46.2 ± 14.8 versus 52.0 ± 14.9 versus 52.3 ± 16.0mL/cmH2O; p < 0.001). There was a transient increase in airway resistance (6.6 ± 3.6 versus 8.0 ± 5.5 versus 6.6 ± 3.5cmH2O/Ls-1; p < 0.001) and a transient reduction in peak expiratory flow (32.0 ± 16.0 versus 29.8 ± 14.8 versus 32.1 ± 15.3Lpm; p <0.05) immediately after the technique; these values returned to pretechnique levels after tracheal aspiration. There were no changes in the control condition, nor were hemodynamic alterations observed.
Ventilator hyperinflation promoted increased compliance associated with a transient increase in airway resistance and peak expiratory flow, with reduction after aspiration.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):296-302
DOI 10.5935/0103-507X.20190054
Evaluate the physiological and autonomic nervous system responses of premature newborns to body position and noise in the neonatal intensive care unit.
A quasi-experimental study. The autonomic nervous system of newborns was evaluated based on heart rate variability when the newborns were exposed to environmental noise and placed in different positions: supine without support, supine with manual restraint and prone.
Fifty premature newborns were evaluated (gestational age: 32.6 ± 2.3 weeks; weight: 1816 ± 493g; and Brazelton sleep/awake level: 3 to 4). A positive correlation was found between environmental noise and sympathetic activity (R = 0.27, p = 0.04). The mean environmental noise was 53 ± 14dB. The heart rate was higher in the supine position than in the manual restraint and prone positions (148.7 ± 21.6, 141.9 ± 16 and 144 ± 13, respectively) (p = 0.001). Sympathetic activity, represented by a low frequency index, was higher in the supine position (p < 0.05) than in the other positions, and parasympathetic activity (high frequency, root mean square of the sum of differences between normal adjacent mean R-R interval and percentage of adjacent iRR that differed by more than 50ms) was higher in the prone position (p < 0.05) than in the other positions. The complexity of the autonomic adjustments (approximate entropy and sample entropy) was lower in the supine position than in the other positions.
The prone position and manual restraint position increased both parasympathetic activity and the complexity of autonomic adjustments in comparison to the supine position, even in the presence of higher environmental noise than the recommended level, which tends to increase sympathetic activity.

Abstract
Rev Bras Ter Intensiva. 2019;31(3):303-311
DOI 10.5935/0103-507X.20190055
To evaluate the medical knowledge regarding the application of the diagnostic criteria for brain death and to correlate it with training parameters for this diagnosis according to Federal Council of Medicine resolution 2,173 of 2017.
We interviewed 174 physicians with experience with comatose patients. A structured questionnaire adapted from previous studies was used. The associations of the variables were tested using the chi-square test for independence. A multivariate logistic model was fitted for associations with p values ≤ 0.20.
Among the interviewees, 40% had been working for more than 1 year in intensive care, and 23% had initiated ten or more brain death protocols complying with the new resolution. Forty-five percent of the interviewees reported having difficulty following the criteria, 94% acknowledged the need for complementary tests for diagnosis, and 8% of them reported the existence of incorrect tests. The difficulty with these criteria decreased with an increase in the number of years of medical training (OR = 0.487; p = 0.045; 95%CI 0.241 - 0.983) and with a higher number of initiated brain death protocols (OR = 0.223; p = 0.0001; 95%CI 0.117 - 0.424).
Difficulties in the application of brain death criteria were identified by a significant portion of the sample. However, among other factors, more years of training and a greater number of initiated brain death protocols were associated with greater ease in the application of brain death criteria according to the guidelines provided in Resolution 2,173 of the Federal Council of Medicine.