Abstract
Rev Bras Ter Intensiva. 2019;31(1):79-85
DOI 10.5935/0103-507X.20190012
We aimed to determine the incidence, risk factors, and outcomes of unplanned extubation among adult patients.
We conducted a prospective cohort study of adult intubated patients admitted to the charity wards of a government tertiary teaching hospital in the Philippines. Patients managed in both intensive care and nonintensive care settings were included. Patients were followed-up until discharge or until seven days postextubation.
The outcomes of the 191 included patients were planned extubation (35%), unplanned extubation (19%), death (39%), and discharge against advice (7%). Competing risk regression showed that male sex (Crude OR: 2.25, 95%CI: 1.10 - 4.63) and age (Crude OR 0.976, 95%CI: 0.957 - 0.996) were significant baseline factors. The night shift (Crude OR: 24.6, 95%CI: 2.87 - 211) was also consistently associated with more unplanned extubations. Among postextubation outcomes, reintubation (unplanned extubation: 61.1% versus planned extubation: 25.4%), acute respiratory failure (unplanned extubation: 38.9% versus planned extubation: 17.5%), and cardiovascular events (unplanned extubation: 8.33% versus planned extubation: 1.49%) occurred significantly more often among the unplanned extubation patients. Admission in an intensive care unit was not associated with a lower risk of unplanned extubation (Crude OR 1.15, 95%CI: 0.594 - 2.21).
Many intubated patients had unplanned extubation. Patients admitted in nonintensive care unit settings did not have significantly higher odds of unplanned extubation.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):47-56
DOI 10.5935/0103-507X.20190011
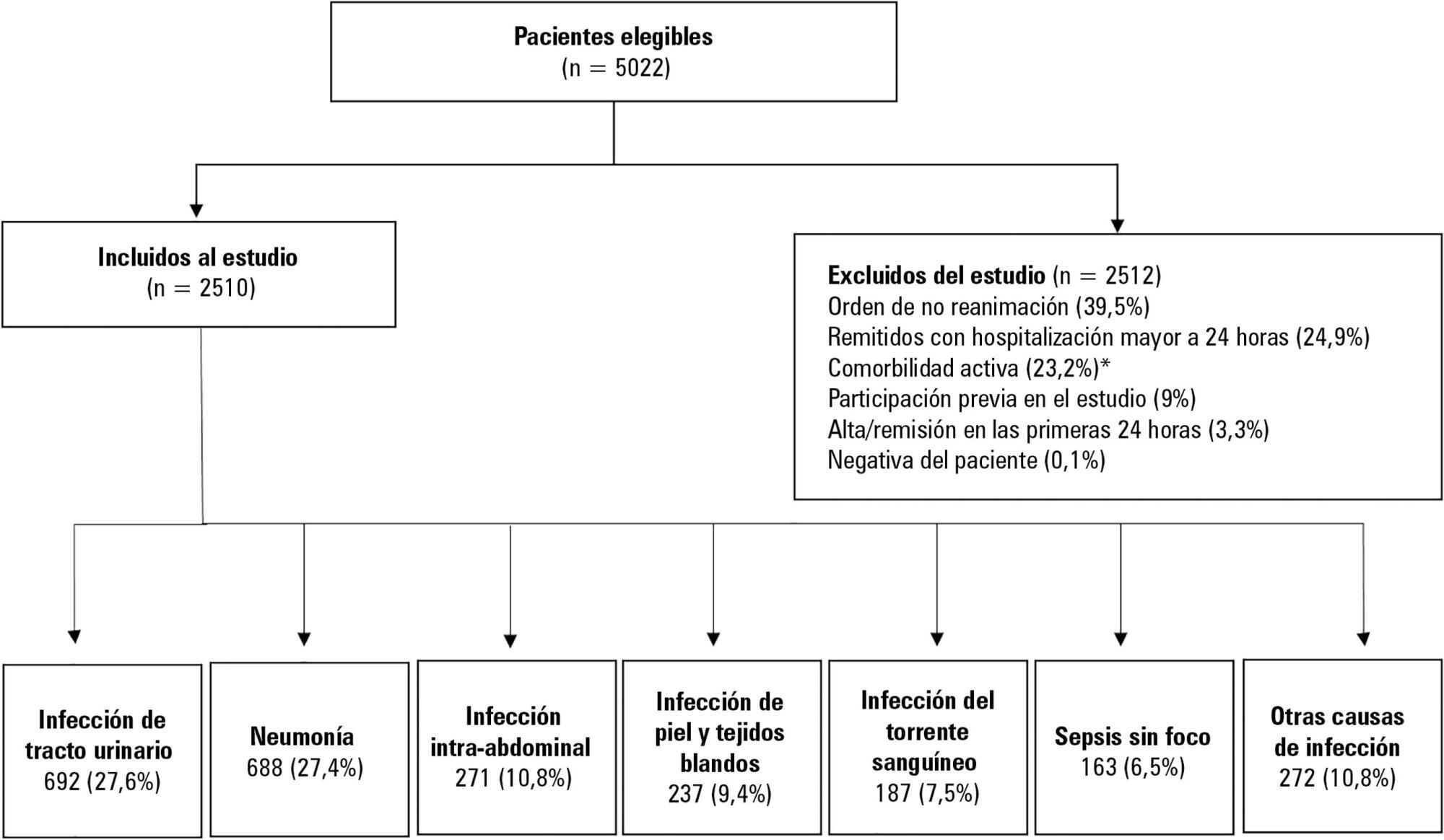
To determine the association between the primary site of infection and in-hospital mortality as the main outcome, or the need for admission to the intensive care unit as a secondary outcome, in patients with sepsis admitted to the emergency department.
This was a secondary analysis of a multicenter prospective cohort. Patients included in the study were older than 18 years with a diagnosis of severe sepsis or septic shock who were admitted to the emergency departments of three tertiary care hospitals. Of the 5022 eligible participants, 2510 were included. Multiple logistic regression analysis was performed for mortality.
The most common site of infection was the urinary tract, present in 27.8% of the cases, followed by pneumonia (27.5%) and intra-abdominal focus (10.8%). In 5.4% of the cases, no definite site of infection was identified on admission. Logistic regression revealed a significant association between the following sites of infection and in-hospital mortality when using the urinary infection group as a reference: pneumonia (OR 3.4; 95%CI, 2.2 - 5.2; p < 0.001), skin and soft tissues (OR 2.6; 95%CI, 1.4 - 5.0; p = 0.003), bloodstream (OR 2.0; 95%CI, 1.1 - 3.6; p = 0.018), without specific focus (OR 2.0; 95%CI, 1.1 - 3.8; p = 0.028), and intra-abdominal focus (OR 1.9; 95%CI, 1.1 - 3.3; p = 0.024).
There is a significant association between the different sites of infection and in-hospital mortality or the need for admission to an intensive care unit in patients with sepsis or septic shock. Urinary tract infection shows the lowest risk, which should be considered in prognostic models of these conditions.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):57-62
DOI 10.5935/0103-507X.20190016
To assess the Perme mobility scale score as a predictor of functional status and complications in the postoperative period in patients undergoing liver transplantation.
The sample consisted of 30 patients who underwent liver transplantation. The patients were evaluated at two time points to determine their perception of pain, degree of dyspnea, peripheral muscle strength, and functional status according to the Perme scale. The collected data were analyzed by descriptive and inferential statistics. To compare the means between the evaluations, Student's t test for paired samples was applied. In case of asymmetry, the Wilcoxon test was used. In the evaluation of the association between the quantitative variables, the Pearson or Spearman correlation tests were applied.
A total of 30 individuals who underwent liver transplantation were included. The patients were predominantly male, and the mean age was 58.4 ± 9.9 years. The most prevalent underlying pathology was cirrhosis C virus (23.3%). Significant associations of the time on mechanical ventilation with the Perme scale score at discharge from the intensive care unit (r = -0.374; p = 0.042) and the number of physical therapy treatments (r = -0.578; p = 0.001) were recorded. When comparing the results of the initial evaluation and the evaluation at hospital discharge, there was a significant improvement in functional status (p < 0.001).
Functional mobility, peripheral muscle strength, pain perception, and dyspnea are significantly improved at hospital discharge compared with those at inpatient unit admission.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):71-78
DOI 10.5935/0103-507X.20190013
To compare the clinical characteristics and outcomes of patients with community-acquired and hospital-acquired sepsis.
This is a retrospective cohort study that included all patients with a diagnosis of sepsis detected between January 2010 and December 2015 at a private hospital in southern Brazil. Outcomes (mortality, intensive care unit and hospital lengths of stay) were measured by analyzing electronic records.
There were 543 hospitalized patients with a diagnosis of sepsis, with a frequency of 90.5 (85 to 105) cases/year. Of these, 319 (58%) cases were classified as hospital-acquired sepsis. This group exhibited more severe disease and had a larger number of organ dysfunctions, with higher hospital [8 (8 - 10) versus 23 (20 - 27) days; p < 0.001] and intensive care unit [5 (4 - 7) versus 8.5 (7 - 10); p < 0.001] lengths of stay and higher in-hospital mortality (30.7% versus 15.6%; p < 0.001) than those with community-acquired sepsis. After adjusting for age, APACHE II scores, and hemodynamic and respiratory dysfunction, hospital-acquired sepsis remained associated with increased mortality (OR 1.96; 95%CI 1.15 - 3.32, p = 0.013).
The present results contribute to the definition of the epidemiological profile of sepsis in the sample studied, in which hospital-acquired sepsis was more severe and was associated with higher mortality.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):64-70
DOI 10.5935/0103-507X.20180012
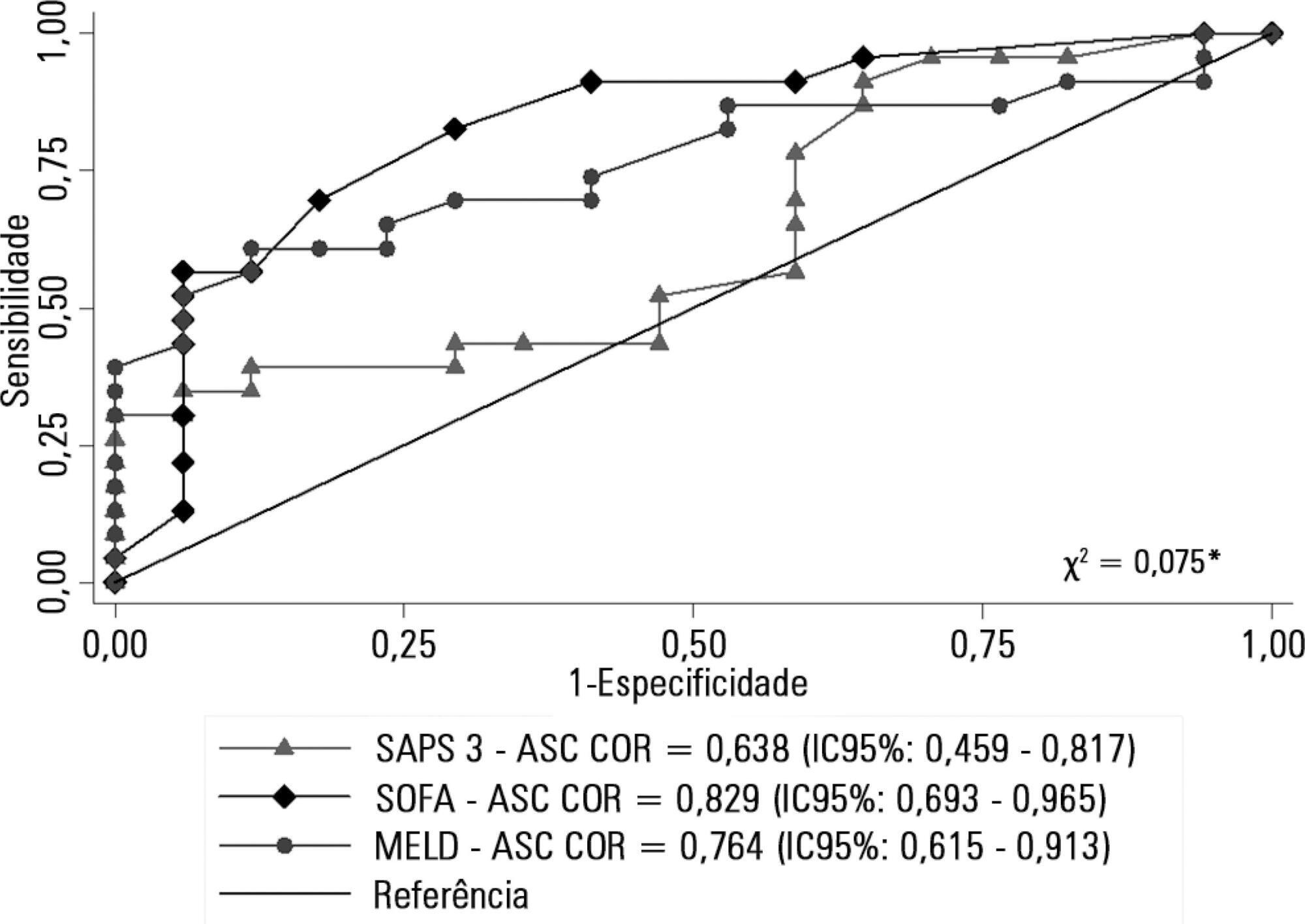
To describe a cohort of patients with acute liver failure and to analyze the demographic and clinical factors associated with mortality.
Retrospective cohort study in which all patients admitted for acute liver failure from July 28, 2012, to August 31, 2017, were included. Clinical and demographic data were collected using the Epimed System. The SAPS 3, SOFA, and MELD scores were measured. The odds ratios and 95% confidence intervals were estimated. Receiver operating characteristics curves were obtained for the prognostic scores, along with the Kaplan-Meier survival curve for the score best predicting mortality.
The majority of the 40 patients were female (77.5%), and the most frequent etiology was hepatitis B (n = 13). Only 35% of the patients underwent liver transplantation. The in-hospital mortality rate was 57.5% (95%CI: 41.5 - 73.5). Among the scores investigated, only SOFA remained associated with risk of death (OR = 1.37; 95%CI 1.11 - 1.69; p < 0.001). After SOFA stratification into < 12 and ≥ 12 points, survival was higher in patients with SOFA <12 (log-rank p < 0.001).
SOFA score in the first 24 hours was the best predictor of fatal outcome.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):71-79
DOI 10.5935/0103-507X.20180013
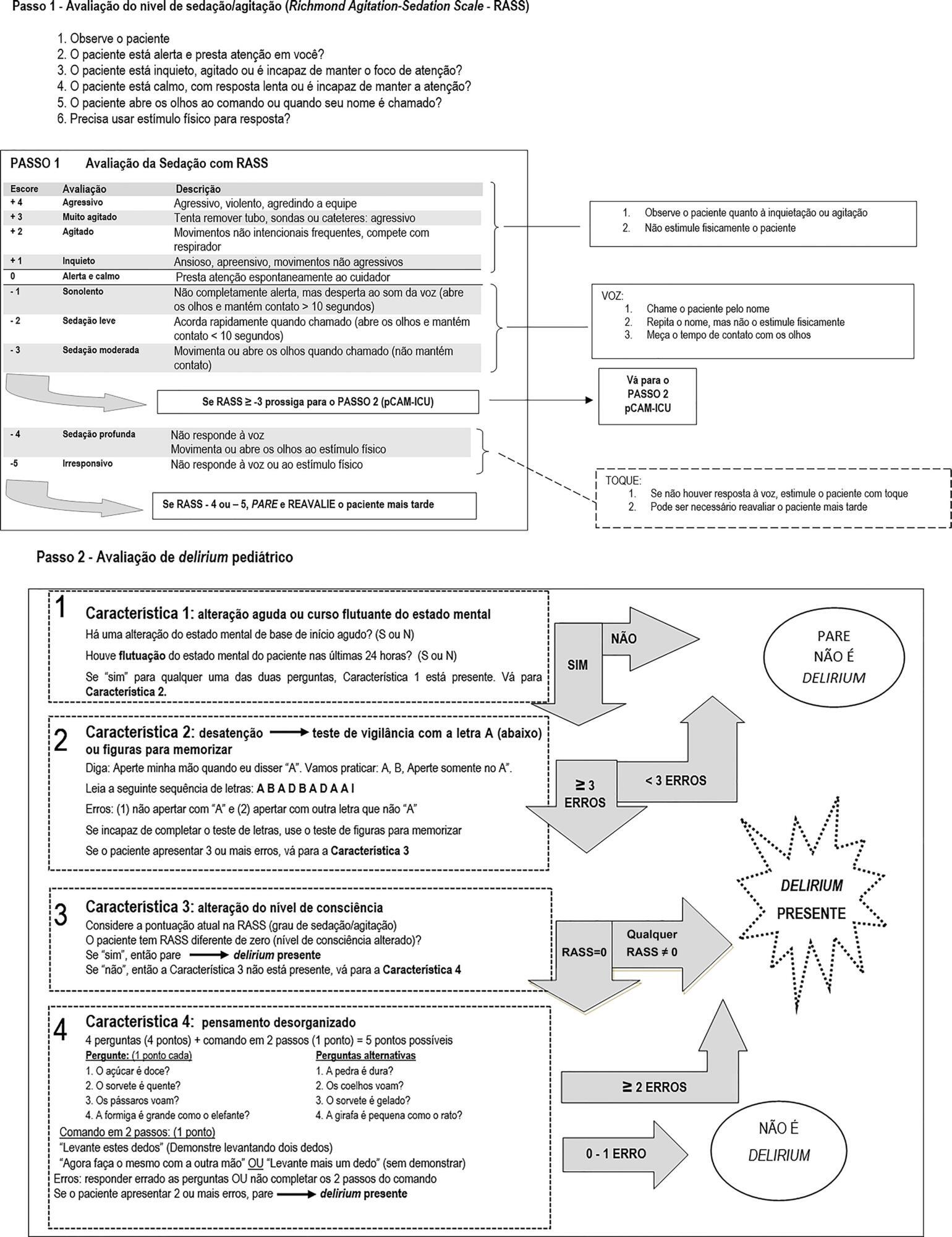
To undertake the translation and cross-cultural adaption into Brazilian Portuguese of the Pediatric Confusion Assessment Method for the Intensive Care Unit for the detection of delirium in pediatric intensive care units, including the algorithm and instructions.
A universalist approach for the translation and cross-cultural adaptation of health measurement instruments was used. A group of pediatric critical care specialists assessed conceptual and item equivalences. Semantic equivalence was evaluated by means of a translation from English to Portuguese by two independent translators; reconciliation into a single version; back-translation by a native English speaker; and consensus among six experts with respect to language and content understanding by means of Likert scale responses and the Content Validity Index. Finally, operational equivalence was assessed by applying a pre-test to 30 patients.
The back-translation was approved by the original authors. The medians of the expert consensus responses varied between good and excellent, except for the feature "acute onset" of the instructions. Items with a low Content Validity Index for the features "acute onset" and "disorganized thinking" were adapted. In the pre-test, the expression "signal with your head" was modified into "nod your head" for better understanding. No further adjustments were necessary, resulting in the final version for Brazilian Portuguese.
The Brazilian version of the Pediatric Confusion Assessment Method for the Intensive Care Unit was generated in agreement with the international recommendations and can be used in Brazil for the diagnosis of delirium in critically ill children 5 years of age or above and with no developmental cognitive disabilities.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):28-34
DOI 10.5935/0103-507X.20180008
To investigate the longterm psychological outcome in survivors of critical illness after intensive care unit discharge.
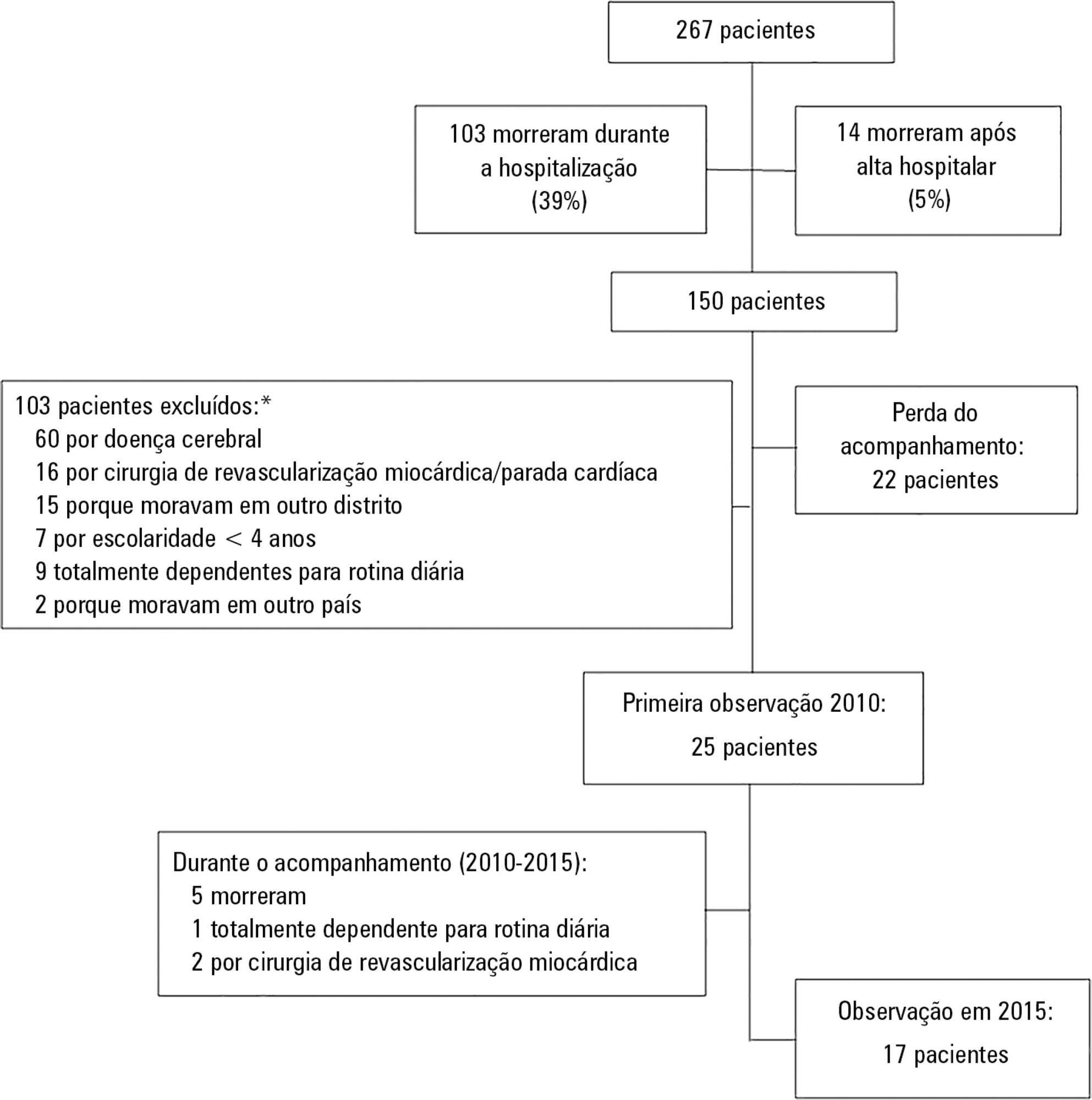
A prospective cohort of survivors admitted to a mixed intensive care unit between January and September 2010 was evaluated six months and five years after hospital discharge. The Dementia Rating Scale-2, the Hospital Anxiety and Depression Scale, the Posttraumatic stress syndrome 14-questions inventory, the Euro Quality of Life 5 Dimensions (EQ-5-D), and the Visual Analogue Scale (EQ VAS) were assessed at both follow-up periods.
Of 267 patients, 25 patients were evaluated at 6 months after discharge (62 ± 16 years); 12 (48%) presented cognitive impairment, 6 (24%) anxiety, 4 (16%) depression, and 4 (16%) post-traumatic stress disorder. Among those re-evaluated five years after discharge (n = 17; 65 ± 15 years), the frequency of cognitive impairment dropped from 8 (47%) to 3 (18%) (p = 0.063), due to improvement in these patients over time, and other patients did not acquire any dysfunction after discharge. At five years after discharge, only two patients (12%) reported anxiety, and none had depression or post-traumatic stress disorder. No differences were found between the six-month and five-year follow-ups regarding EQ-5-D and EQ VAS.
Survivors do not show a progressive decline in cognitive function or quality of life within five years after intensive care unit discharge. Psychopathological symptoms tend to decrease with time.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):42-49
DOI 10.5935/0103-507X.20180009
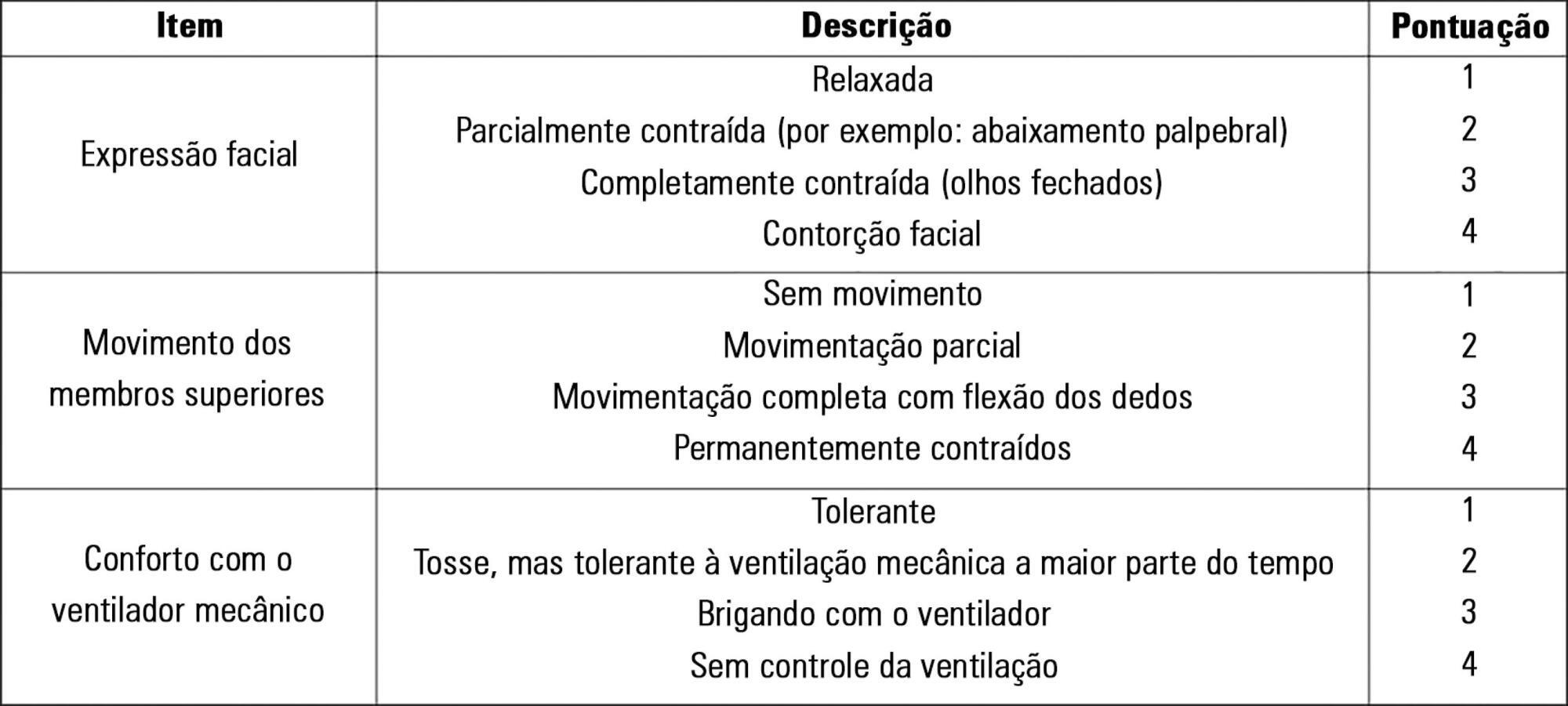
To evaluate the validity and reliability of the Brazilian version of the Behavioral Pain Scale (BPS-Br) in victims of traumatic brain injury.
Observational prospective study with paired and repeated measures conducted at two intensive care units (clinical and surgical) of a large general hospital. The convenience sample consisted of adult victims of moderate or severe penetrating or blunt craniocerebral trauma who were sedated and mechanically ventilated. A total of 432 paired observations were performed by independent evaluators simultaneously, prior to eye cleaning, during eye cleaning, during tracheal aspiration and after tracheal aspiration. Sociodemographic, clinical, trauma-related, sedoanalgesia and physiological parameter data (heart rate, systolic and diastolic blood pressure) were collected. The discriminant validity was tested using the Friedman and Wilcoxon paired tests. The intraclass correlation coefficient and Cohen's Kappa coefficient were used to evaluate the reliability. The Spearman correlation test was used to test the association between clinical variables and BPS-Br scores during tracheal aspiration.
There was a significant increase in the physiological parameters during tracheal aspiration, but without correlation with the BPS-Br scores. Pain was significantly more intense during tracheal aspiration (p < 0.005). Satisfactory interobserver agreement was found, with an intraclass correlation coefficient of 0.95 (0.90 - 0.98) and Kappa coefficient of 0.70.
Brazilian version of the Behavioral Pain Scale scores increased during tracheal aspiration. The Brazilian version of the scale was valid and reliable for pain assessment of traumatic brain injury victims undergoing tracheal aspiration.