Abstract
Rev Bras Ter Intensiva. 2012;24(2):184-187
DOI 10.1590/S0103-507X2012000200015
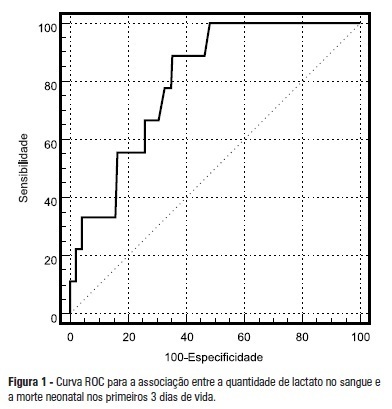
OBJECTIVE: To assess the correlation between plasma lactate concentrations in the first 6 hours of life and early neonatal mortality. METHODS: The patients were divided in 2 groups based on the cutoff point, obtained from a receiver operating characteristic (ROC) curve, of the plasma lactate concentration that best predicted neonatal mortality during the first 3 days of life. The differences between groups and the correlations between the investigated variables and the plasma lactate concentrations measured in the first 6 hours of life were analyzed using the Chi-square, Student's t, or Mann-Whitney tests and logistic regression. RESULTS: The best cutoff point of the plasma lactate concentration as determined by the ROC curve for death during the first 3 days of life was 4.2 mmol/L. The investigated groups differed with regards to the average birth weight, which was lower in the group with serum lactate levels > 4.2 mmol/L, and the match between birth weight and gestational age, where the group with serum lactate levels > 4.2 mmol/L exhibited a higher number of newborns small for their gestational age. Seizures, intracranial hemorrhage, and death during the first 3 days of life occurred more frequently in the group with serum lactate levels > 4.2 mmol/L. CONCLUSION: In the investigated samples, the presence of plasma lactate concentrations > 4.2 mmol/L in the first 6 hours of life correlated with neonatal death during the first 3 days of life, a higher frequency of neurologic morbidity, and newborns that were small for their gestational age.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):72-78
DOI 10.1590/S0103-507X2012000100011
OBJECTIVE: To assess the effects of passive mobilization on acute hemodynamic responses in mechanically ventilated patients. METHODS: This cross-sectional, quantitative, observational study enrolled patients who were admitted to the intensive care unit, sedated and mechanically ventilated. The infusion of sedative and analgesic drugs aimed to maintain a Ramsay scale sedation level of 4 to 6. Passive mobilization consisted of hip and knee flexion-extension movements for five minutes. After 10 minutes of rest, an additional five minutes of flexion-extension passive movements was performed for the shoulders. Hemodynamic assessments (heart rate and systolic, diastolic and mean blood pressure) were performed one minute before the mobilization protocol and one minute after each phase. The double product and myocardial oxygen consumption were calculated using appropriate formulas. RESULTS: A total of 13 patients (69.2% male, with a mean age of 69.1 ± 15.8 years) were admitted from June to December, 2011. Passive mobilization led to statistically significant increases in heart rate, double product and myocardial oxygen consumption. However, mean blood pressure was not significantly altered. CONCLUSIONS: Our results suggest that passive mobilization of mechanically ventilated and sedated patients is safe and provides beneficial effects on acute hemodynamic parameters, particularly heart rate, although mean blood pressure is not significantly altered
Abstract
Rev Bras Ter Intensiva. 2012;24(1):79-85
DOI 10.1590/S0103-507X2012000100012
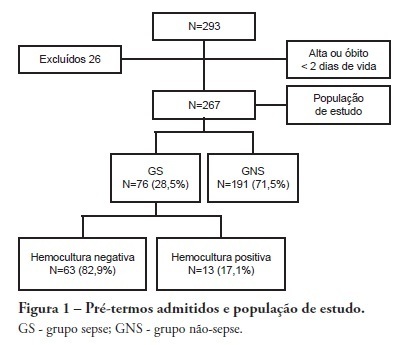
OBJECTIVE: To evaluate the prevalence factors and etiologies associated with late neonatal sepsis in preterm neonates in a neonatal intensive care unit. METHODS: This was a cross-sectional study of secondary data pertaining to preterm neonates admitted to the neonatal intensive care unit between 2008 and 2010 and was gathered from medical charts. The outcome variable, late neonatal sepsis, was characterized using the Brazilian national health surveillance agency criteria. Pearson's Chi-squared test, Fisher's exact test and the linear trend Chi-squared test were used to assess the qualitative variables for linear trends. The statistical significance level was set at p < 0.05. Bivariate and multivariate analyses of the independent and dependent variables were conducted to obtain a measure of the effect and prevalence ratios, considering a p-value of less than 0.20 to indicate statistical significance. RESULTS: This study included 267 preterm neonates. Of the participants, 28.5% were characterized as having late-onset sepsis. Positive blood cultures were recorded for 17.1% of the neonates. Death occurred in 8.2% of the total cases, and of these deaths, 68.2% occurred within the sepsis group. Three deaths were associated with positive blood cultures, all of which grew Gram-negative bacteria. The bivariate analysis demonstrated that as the gestational age and birth weight decreased, the prevalence of late-onset sepsis trended upward. Ten or more days on mechanical ventilation was associated with late-onset neonatal sepsis in 80.8% of cases. Peripherally inserted central catheters left in place for 11 or more days were associated with late-onset neonatal sepsis in 76.2% of cases. The multivariate analysis demonstrated that a peripherally inserted catheter left in place for less than 11 days was associated with late-onset neonatal sepsis. Gram-negative bacteria, including Klebsiella pneumoniae and Escherichia coli, were the most frequent causative agents. CONCLUSIONS: Late sepsis remains a concern because of its prevalence in intensive care units and because it increases the number of invasive procedures that preterm children usually undergo in these units. The authors emphasize the expanding role of Gram-negative bacteria in late-onset neonatal sepsis and the need for more efficient methods to identify confirmed sepsis.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):35-42
DOI 10.1590/S0103-507X2012000100006
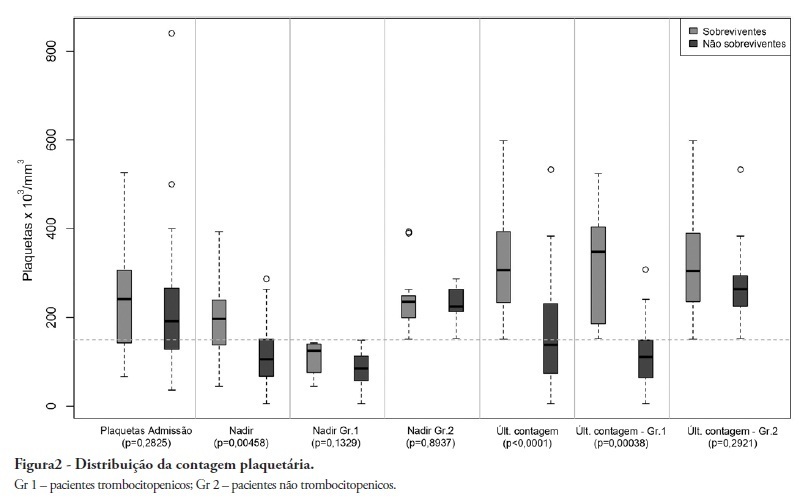
OBJECTIVE: To demonstrate an association between thrombocytopenia and platelet behavior in predicting mortality in septic patients. METHODS: Patients with criteria for sepsis at admission or at any time during hospitalization were selected; patients hospitalized for less than 24 hours were excluded. Thrombocytopenia was defined as a platelet count lower than 150.000/mm³, and recovery was defined as returning to levels above 150.000/mm³ after showing thrombocytopenia. We assessed the admission prognosis variables (APACHE II), platelet counts during the hospitalization and outcomes. RESULTS: Of the 56 patients included, 34 developed thrombocytopenia during sepsis (Group 1) and had a 76.4% mortality rate. The mortality rate among patients not showing thrombocytopenia (Group 2) was 40.9% (RR 1.87; 95% CI 1.12 - 3.12; p = 0.0163). In 44.1% of Group 1 patients, the platelet counts drops by >50% compared with the admission counts; 93.3% of these patients eventually died (RR 1.48; 95% CI 0.93 - 2.36; p = 0.0528). Among the Group 1 patients showing recovered platelet counts, 53.3% survived; 100% of the patients with unrecovered thrombocytopenia died (RR 2.14; 95% CI 1.35 - 3.39; p = 0.0003). Among the patients with APACHE II scores > 22, the thrombocytopenic patients had an 81.8% mortality rate (p = 0.25), while no deaths occurred among the non-thrombocytopenic patients. For the patients with APACHE II scores ≤ 22, the mortality rate of the thrombocytopenic patients was 74% (p = 0.0741), versus 42.8% for the non-thrombocytopenic patients. CONCLUSION: For this sample of septic patients, thrombocytopenia and its progression, defined as a >50% drop or failure to recover platelet count, were shown to be markers of poor prognosis.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):43-51
DOI 10.1590/S0103-507X2012000100007
OBJECTIVE: The objective of this study was to assess the effects of positive end-expiratory pressure on recruitment, cyclic recruitment and derecruitment and strain in patients with acute lung injury and acute respiratory distress syndrome using lung computed tomography. METHODS: This is an open, controlled, non-randomized interventional study of ten patients with acute lung injury and acute respiratory distress syndrome. Using computed tomography, single, basal slices of the lung were obtained during inspiratory and expiratory pauses at a tidal volume of 6 ml/kg and a positive end-expiratory pressure of 5, 10, 15 and 20 cmH2O. The densities of the lung parenchyma were measured in Hounsfield units. The values for positive end-expiratory pressure-induced recruitment, cyclic recruitment and derecruitment and strain were then calculated. RESULTS: Increasing levels of positive end-expiratory pressure were correlated with increased recruitment and global strain (p < 0.01), which was significantly correlated with plateau pressure (r² = 0.97, p < 0.01). In addition, increasing levels of positive end-expiratory pressure systematically increased strain along the sternovertebral axis. CONCLUSION: While strain is an adverse effect of positive end-expiratory pressure, the decision use positive end-expiratory pressure with any patient should be balanced against the potential benefits of recruitment. Due to the small number of patients in this study, the present data should be treated as hypothesis generating and is not intended to limit the clinical application of a high level of positive end-expiratory pressure in patients with severe hypoxemia.

Abstract
Rev Bras Ter Intensiva. 2012;24(1):52-57
DOI 10.1590/S0103-507X2012000100008
OBJECTIVE: To determine the association between the preoperative administration of statins and postoperative delirium in a prospective cohort of patients undergoing cardiac surgery. METHODS: All adult patients who were admitted to the intensive care unit following cardiac surgery between January and June 2011 were included. Delirium was screened during the postoperative period using the Confusion Assessment Method for Intensive Care Unit (CAM-ICU) and Intensive Care Delirium Screening Checklist (ICDSC). RESULTS: A total of 169 patients underwent elective cardiac surgery, and 40.2% of the patients were treated preoperatively with statins. Delirium was identified using the CAM-ICU in 14.9% of patients not taking preoperative statins in comparison with 11.8% of the patients taking statins (p = 0.817). Using the ICDSC, delirium was identified in 18.8% of patients not taking statins in comparison with 10.3% of the patients taking statins (p = 0.191). CONCLUSION: The use of preoperative statins is not correlated with postoperative delirium in patients undergoing cardiac surgery.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):58-63
DOI 10.1590/S0103-507X2012000100009
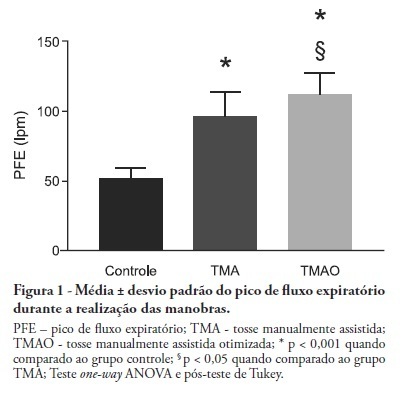
OBJECTIVE: Mechanical ventilation is associated with retained airway secretions. Manually assisted cough contributes to the displacement of bronchial mucus, whereas positive end-expiratory pressure increases collateral ventilation and maintains airway patency. This study aimed to assess the effects of manually assisted cough, either alone or added to increased positive end-expiratory pressure and inspiratory time (optimized manually assisted cough), on the expiratory peak flow and respiratory system mechanics in mechanically ventilated patients. METHODS: In this controlled and randomized clinical trial, respiratory mechanics and expiratory peak flow were assessed in male and female patients undergoing either tracheal suctioning alone, manually assisted cough followed by tracheal suctioning or optimized manually assisted cough followed by tracheal suctioning. RESULTS: Thirty-five patients completed the trial. Respiratory system resistance was significantly reduced after optimized manually assisted cough (16.0 ± 3.6 versus 12.4 ± 3.1 cmH2O/L/s; p = 0.04). The expiratory peak flow during optimized manually assisted cough was significantly higher in comparison with the values observed during manually assisted cough (112.3 ± 15.6 versus 95.8 ± 18.3 Lpm; p < 0.05). Both values were significantly higher than the values observed in the group undergoing tracheal suctioning alone (52.0 ± 7.6 Lpm; p < 0.001). CONCLUSION: Optimized manually assisted cough increases the expiratory peak flow in comparison with manually assisted cough; in addition, this procedure reduces respiratory system resistance.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):64-70
DOI 10.1590/S0103-507X2012000100010
OBJECTIVE: To assess the consciousness level, pulmonary and hemodynamic effects of orthostatic position in intensive care patients. METHODS: This study was conducted from April 2008 to July 2009 in the Adult Intensive Care Unit, Hospital das Clínicas, Universidade Estadual de Campinas, São Paulo, Brazil. Fifteen patients were included who were mechanically ventilated for more than seven days and had the following characteristics: tracheotomized; receiving intermittent nebulization; maximal inspiratory pressure of less than -25 cm H2O; Tobin score less than 105; preserved respiratory drive; not sedated; partial arterial oxygen pressure greater than 70 mm Hg; oxygen saturation greater than 90%; and hemodynamically stable. With inclinations of 0º, 30º and 50º, the following parameters were recorded: consciousness level; blinking reflex; thoracoabdominal cirtometry; vital capacity; tidal volume; minute volume; respiratory muscle strength; and vital signs. RESULTS: No neurological level changes were observed. Respiratory rate and minute volume (V E) decreased at 30% and later increased at 50%; however, these changes were not statistically significant. Abdominal cirtometry and maximal expiratory pressure increased, but again, the changes were not statistically significant. Regarding maximal inspiratory pressure and vital capacity, statistically significant increases were seen in the comparison between the 50º and 0º inclinations. However, tidal volume increased with time in the comparisons between 30º and 0º and between 50º and 0º. Mean blood pressure increased only for the comparison of 50º versus 0º. Heart rate increased with time for the comparisons between 30º and 0º, between 50º and 0º and between 50º and 30º. CONCLUSION: Passive orthostatism resulted in improved tidal volume and vital capacity, maximal inspiratory pressure and increased heart rate and mean blood pressure in critically ill patients.