Abstract
Rev Bras Ter Intensiva. 2020;32(3):474-478
DOI 10.5935/0103-507X.20200078
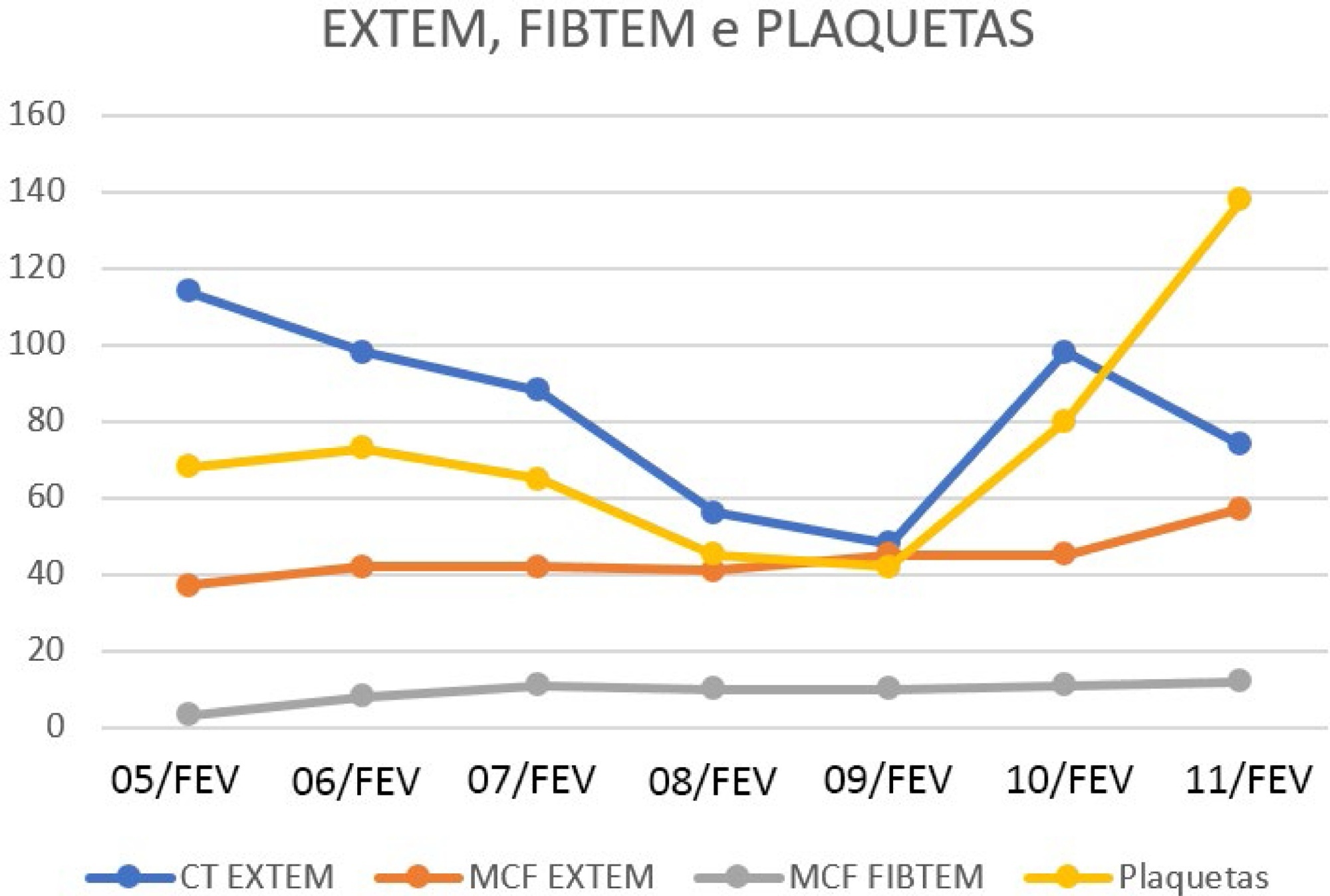
This case report a severe case of yellow fever complicated by liver failure and disseminated intravascular coagulation. Thromboelastometry was capable of identifying clotting disorders and guiding hemostatic therapy. We report the case of a 23-year-old male admitted to the Intensive Care Unit with sudden onset of fever, generalized muscle pain associated with liver failure, and disseminated intravascular coagulation. The results of conventional laboratory tests showed thrombocytopenia, whereas thromboelastometry suggested coagulopathy with slight hypofibrinogenemia, clotting factor consumption, and, consequently, an increased risk of bleeding. Unlike conventional laboratory tests, thromboelastometry identified the specific coagulation disorder and thereby guided hemostatic therapy. Both fibrinogen concentrates and vitamin K were administered, and no blood component transfusion was required, even in the presence of thrombocytopenia. Administration of hemostatic drugs, including fibrinogen concentrate and vitamin K, improved thromboelastometric parameters, correcting the complex coagulation disorder. Blood component transfusion was not performed, and there was no bleeding.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):394-397
DOI 10.5935/0103-507X.20180056
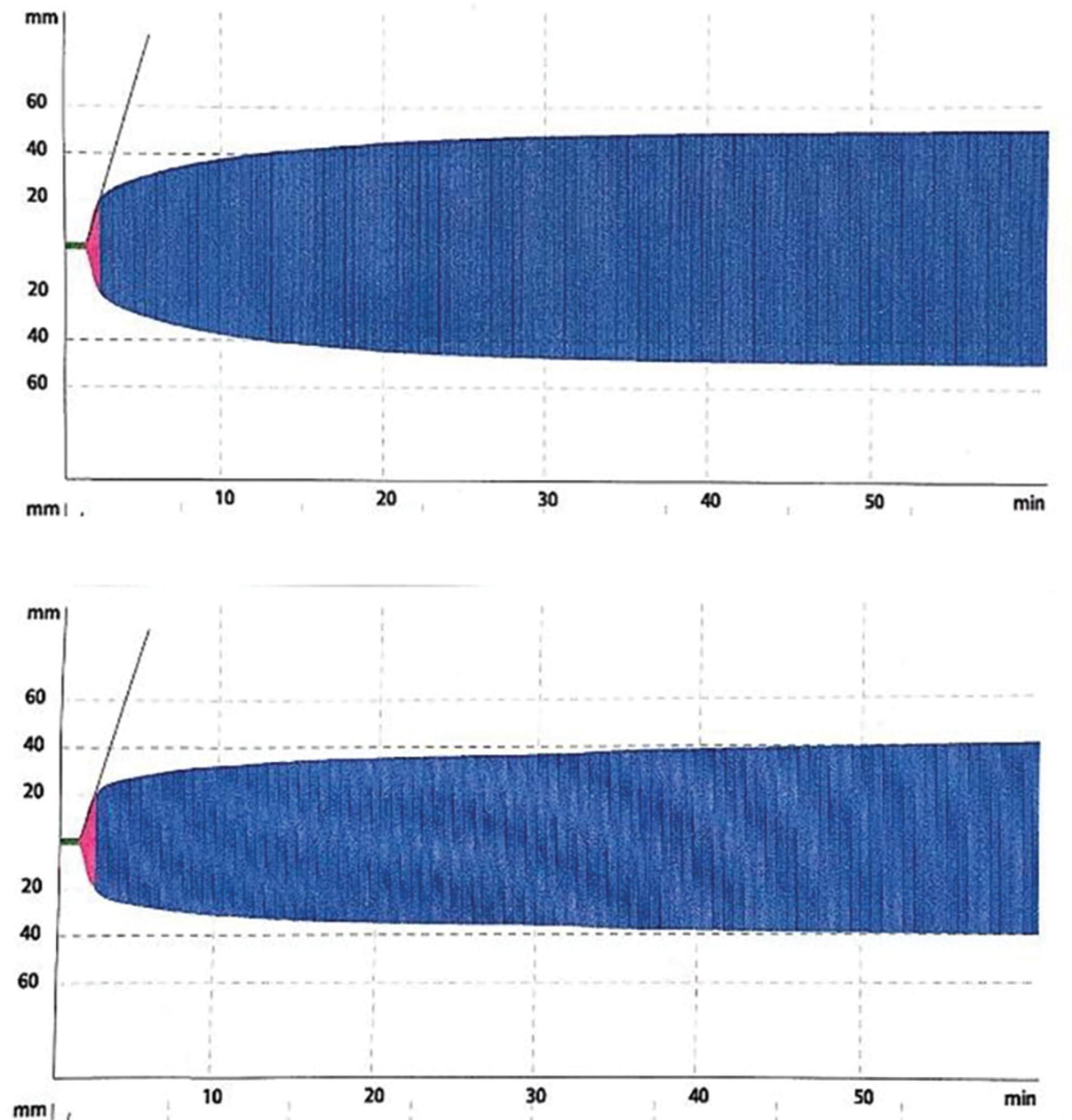
Platelet transfusion is a common practice to prevent spontaneous bleeding or bleeding due to invasive procedures. Transfusion of allogeneic blood components is associated with increased mortality and a worse clinical outcome. The clot strength is assessed by thromboelastometry and determined by the interaction between platelets and fibrinogen. The compensatory effect of high levels of fibrinogen on clot strength in patients with thrombocytopenia has been demonstrated in different clinical settings including sepsis. We report the case of a patient with severe thrombocytopenia whose thromboelastometry showed clot strength that was compensated for by the increase in plasma fibrinogen levels as an acute phase reactant of septic patients. Here, we report a case of a 62-year-old female diagnosed with bone marrow aplasia admitted in the intensive care unit with septic shock and severe thrombocytopenia. During the first 24 hours in the intensive care unit, she presented acute respiratory insufficiency and circulatory shock. The use of invasive mechanical ventilation and norepinephrine was required. Her chest X-ray showed bilateral lung injury. Thus, bronchoscopy with bronchoalveolar lavage was requested. Thromboelastometry was performed and resulted in a normal coagulable profile. Despite severe thrombocytopenia (1,000/mm3), fibrinogen levels were increased (1,050mg/dL) due to septic shock. Bronchoscopy was performed without any active or further bleeding. Here, we report the use of thromboelastometry in the diagnosis of coagulation disorders, preventing unnecessary prophylactic platelet transfusion.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):35-42
DOI 10.1590/S0103-507X2012000100006
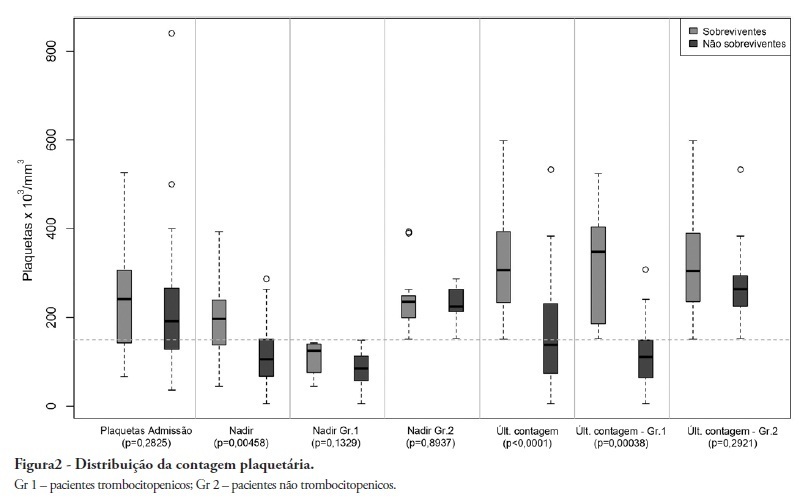
OBJECTIVE: To demonstrate an association between thrombocytopenia and platelet behavior in predicting mortality in septic patients. METHODS: Patients with criteria for sepsis at admission or at any time during hospitalization were selected; patients hospitalized for less than 24 hours were excluded. Thrombocytopenia was defined as a platelet count lower than 150.000/mm³, and recovery was defined as returning to levels above 150.000/mm³ after showing thrombocytopenia. We assessed the admission prognosis variables (APACHE II), platelet counts during the hospitalization and outcomes. RESULTS: Of the 56 patients included, 34 developed thrombocytopenia during sepsis (Group 1) and had a 76.4% mortality rate. The mortality rate among patients not showing thrombocytopenia (Group 2) was 40.9% (RR 1.87; 95% CI 1.12 - 3.12; p = 0.0163). In 44.1% of Group 1 patients, the platelet counts drops by >50% compared with the admission counts; 93.3% of these patients eventually died (RR 1.48; 95% CI 0.93 - 2.36; p = 0.0528). Among the Group 1 patients showing recovered platelet counts, 53.3% survived; 100% of the patients with unrecovered thrombocytopenia died (RR 2.14; 95% CI 1.35 - 3.39; p = 0.0003). Among the patients with APACHE II scores > 22, the thrombocytopenic patients had an 81.8% mortality rate (p = 0.25), while no deaths occurred among the non-thrombocytopenic patients. For the patients with APACHE II scores ≤ 22, the mortality rate of the thrombocytopenic patients was 74% (p = 0.0741), versus 42.8% for the non-thrombocytopenic patients. CONCLUSION: For this sample of septic patients, thrombocytopenia and its progression, defined as a >50% drop or failure to recover platelet count, were shown to be markers of poor prognosis.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)