Abstract
Rev Bras Ter Intensiva. 2022;34(4):524-528
DOI 10.5935/0103-507X.20220342-en
Acute massive pulmonary embolism is the most serious presentation of venous thromboembolism that can ultimately cause obstructive shock, leading to cardiac arrest and death. In this case report, the authors present a case of a 49-year-old female who successfully recovered from a massive pulmonary embolism with the combined use of venoarterial extracorporeal membrane oxygenation and pulmonary aspiration thrombectomy, with no complications from these procedures. Although evidence of benefit from mechanical support has not been established for patients with massive pulmonary embolism, the implementation of extracorporeal cardiocirculatory support during resuscitation may allow improvement of systemic organ perfusion and better chance of survival. Recent guidelines from the European Society of Cardiology state that venoarterial extracorporeal membrane oxygenation in combination with catheter-directed treatment may be considered for patients presenting with massive pulmonary embolism and refractory cardiac arrest. The use of extracorporeal membrane oxygenation as a stand-alone technique with anticoagulation remains controversial, and additional therapies, such as surgical or percutaneous embolectomy, must be considered. Since this intervention is not supported by high-quality studies, we believe it is important to report real-world successful cases. With this case report, we illustrate the benefit derived from resuscitation assisted by extracorporeal mechanical support and early aspiration thrombectomy in patients with massive pulmonary embolism. Additionally, it emphasizes the synergy that derives from integrated multidisciplinary systems for providing complex interventions, of which extracorporeal membrane oxygenation and Interventional Cardiology are clear examples.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):519-523
DOI 10.5935/0103-507X.20220314-en
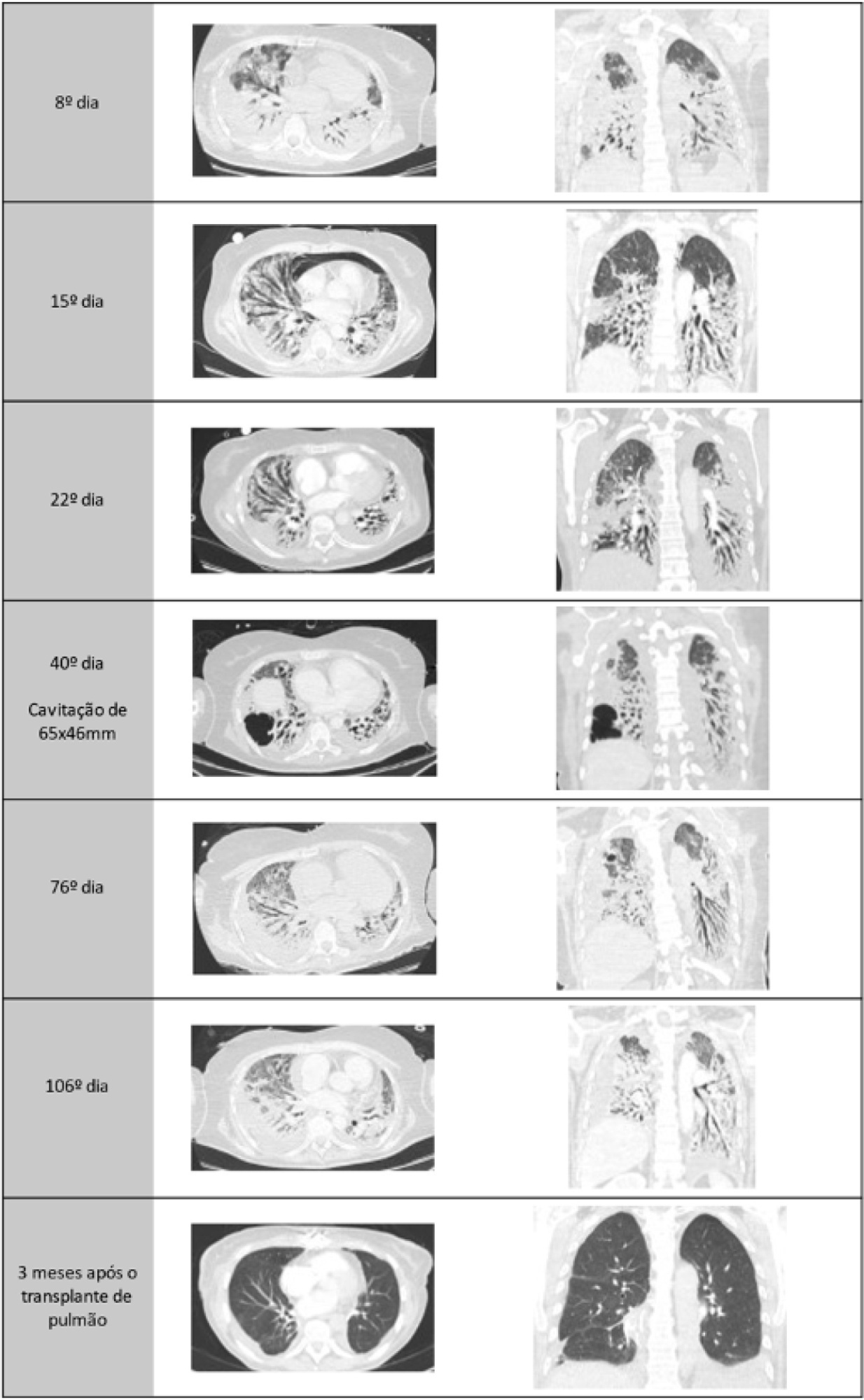
A healthy 55-year-old woman unvaccinated for SARS-CoV-2 was admitted to the hospital with a SARS-CoV-2 infection with rapid clinical deterioration. On the 17th day of disease, she was intubated, and on the 24th day, the patient was referred and admitted to our extracorporeal membrane oxygenation center. Extracorporeal membrane oxygenation support was initially used to enable lung recovery and allow the patient to rehabilitate and improve her physical condition. Despite an adequate physical condition, the lung function was not adequate to discontinue extracorporeal membrane oxygenation, and the patient was considered for lung transplantation. The intensive rehabilitation program was implemented to improve and maintain the physical status throughout all phases. The extracorporeal membrane oxygenation run had several complications that hindered successful rehabilitation: right ventricular failure that required venoarterial-venous extracorporeal membrane oxygenation for 10 days; six nosocomial infections, four with progression to septic shock; and knee hemarthrosis. To reduce the risk of infection, invasive devices (i.e., invasive mechanical ventilation, central venous catheter, and vesical catheter) were removed whenever possible, keeping only those essential for monitoring and care. After 162 days of extracorporeal membrane oxygenation support without other organ dysfunction, bilateral lobar lung transplantation was performed. Physical and respiratory rehabilitation were continued to promote independence in daily life activities. Four months after surgery, the patient was discharged.
Abstract
Rev Bras Ter Intensiva. 2022;34(2):295-299
DOI 10.5935/0103-507X.20220028-en
Posterior reversible encephalopathy syndrome is a rare clinical and radiological syndrome characterized by vasogenic edema of the white matter of the occipital and parietal lobes, which are usually symmetrical, resulting from a secondary manifestation of acute dysfunction of the posterior cerebrovascular system. We describe a case of posterior reversible encephalopathy syndrome secondary to SARS-CoV-2 infection in a 9-year-old boy who developed acute hypoxemic respiratory failure and required assisted mechanical ventilation. The child developed multisystem inflammatory syndrome, and he was monitored in the pediatric intensive care unit and was provided mechanical ventilation and vasoactive agents for hemodynamic support. Additionally, he developed pulmonary and extrapulmonary clinical manifestations along with neuropsychiatric manifestations that required close follow-up and were verified using brain magnetic resonance imaging for timely intervention. Currently, there are few reports of children with posterior reversible encephalopathy syndrome associated with multisystem inflammatory syndrome.
Abstract
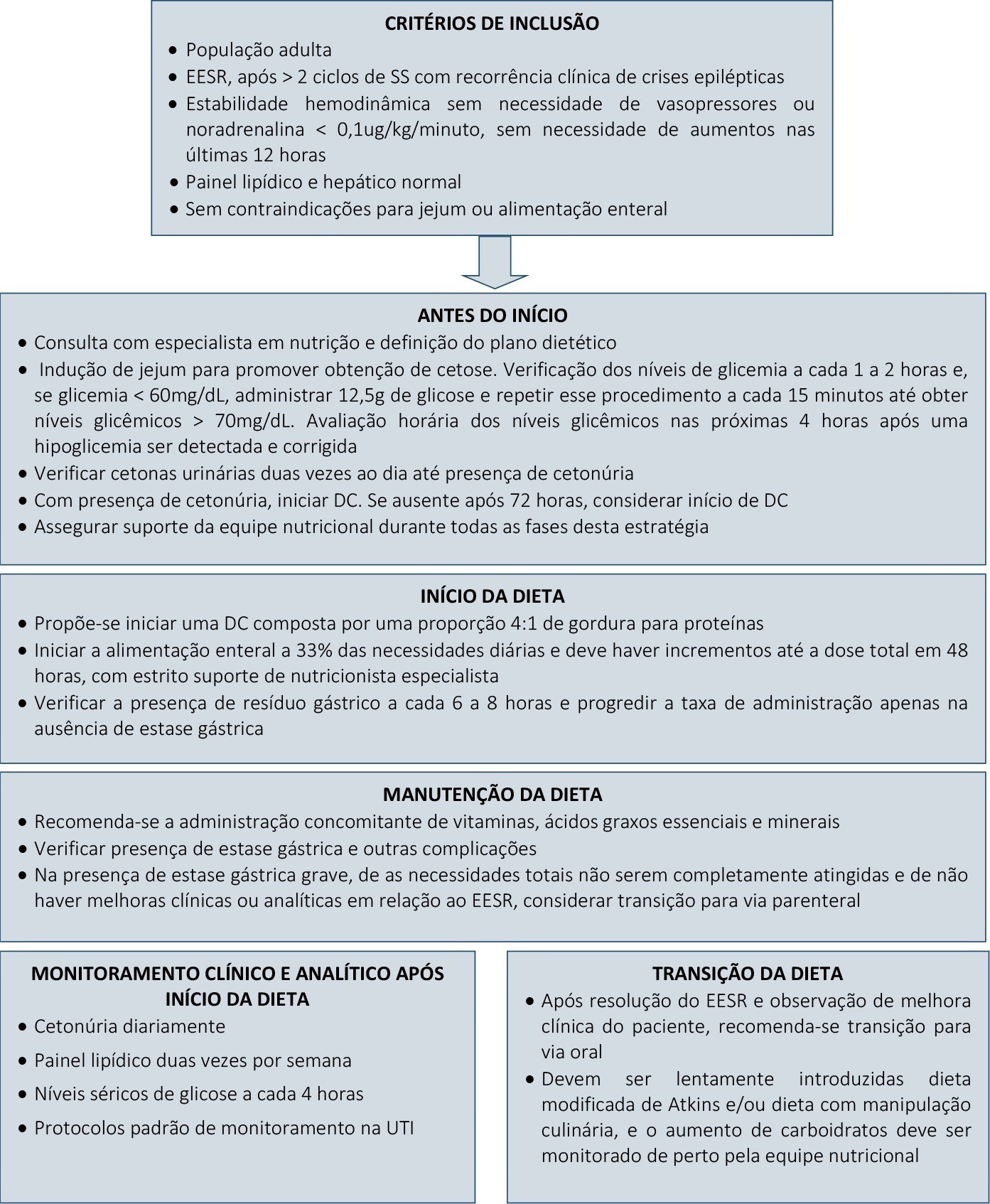
Rev Bras Ter Intensiva. 2021;33(4):635-639
DOI 10.5935/0103-507X.20210089
Super-refractory status epilepticus is defined as seizures that persist or reemerge in the setting of an intravenous anesthetic infusion for more than 24 hours. In recent years, attention has been driven to the potential benefits of a ketogenic diet in the management of these patients. However, the specific role of this strategy in the adult population, as well as its underlying mechanism of action and optimal time for the initiation and management of complications, remain widely debatable. We report a case series of three patients admitted to an intensive care unit due to super-refractory status epilepticus who were managed with a ketogenic diet and propose a clinical approach to its initiation, transition, and management of clinical intercurrences.
Abstract
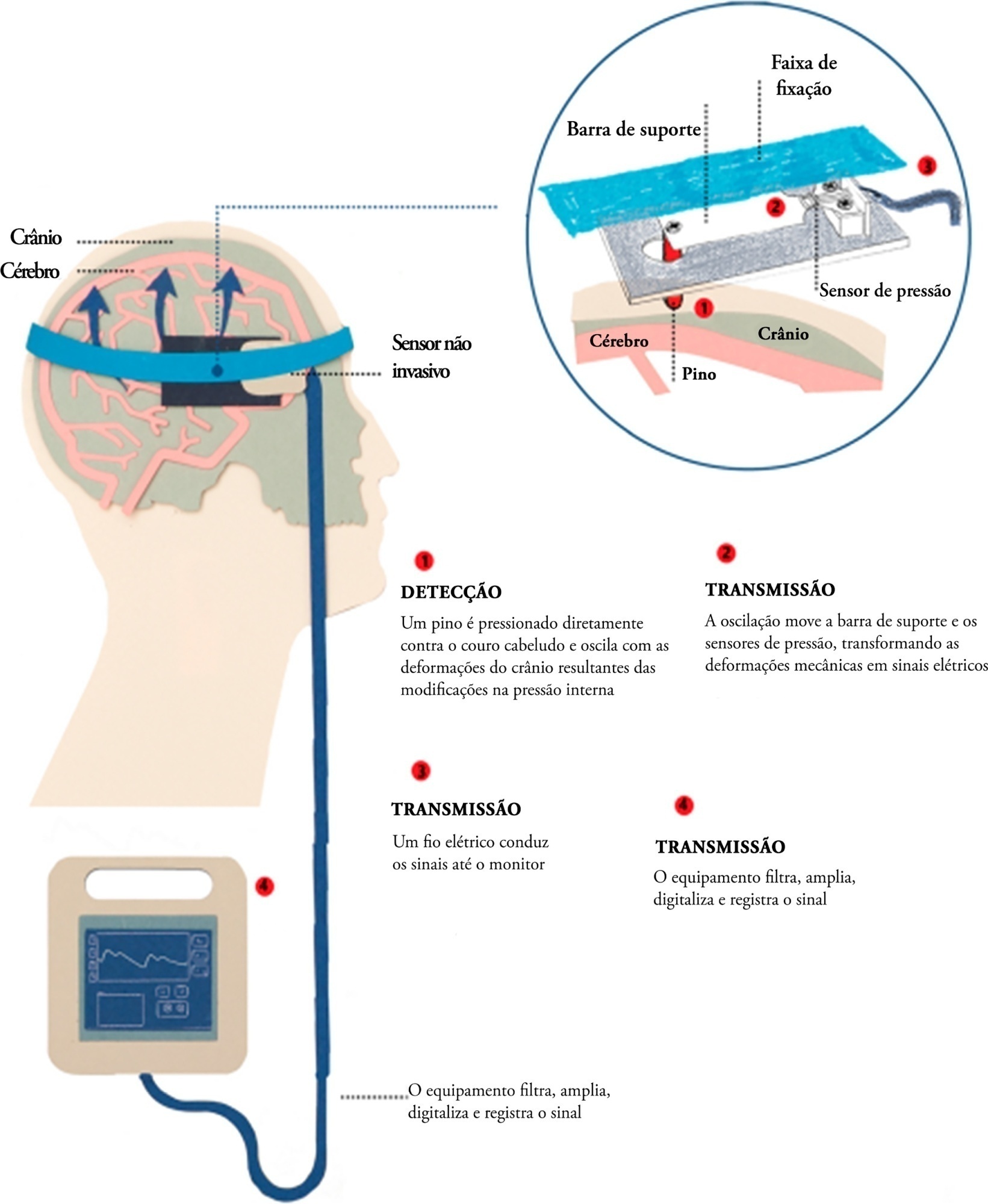
Rev Bras Ter Intensiva. 2021;33(3):469-476
DOI 10.5935/0103-507X.20210066
Brain injury caused by extracorporeal circulation during cardiovascular surgical procedures has been a recurring complication since the implementation of extracorporeal circulation five decades ago. There is no unique cause of brain injury due to the use of extracorporeal circulation, but it is known that brain injury affects about 70% of patients who undergo this procedure. Intracranial pressure assessment is one method that can guide the management of patients undergoing procedures associated with neurological disturbances. This study describes two cases of patients who underwent cardiovascular surgery with extracorporeal circulation in whom clinical protocols for neuroprotection in the postoperative phase were guided by intracranial pressure waveform findings obtained with a novel noninvasive intracranial pressure monitoring method.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):461-468
DOI 10.5935/0103-507X.20210061
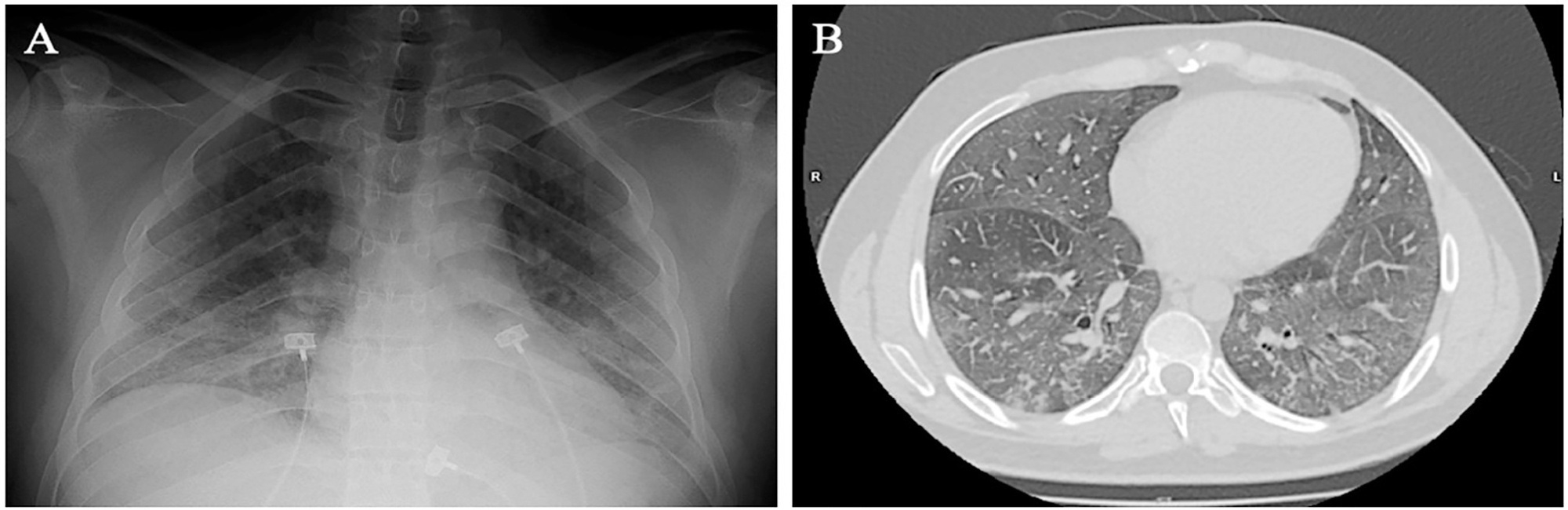
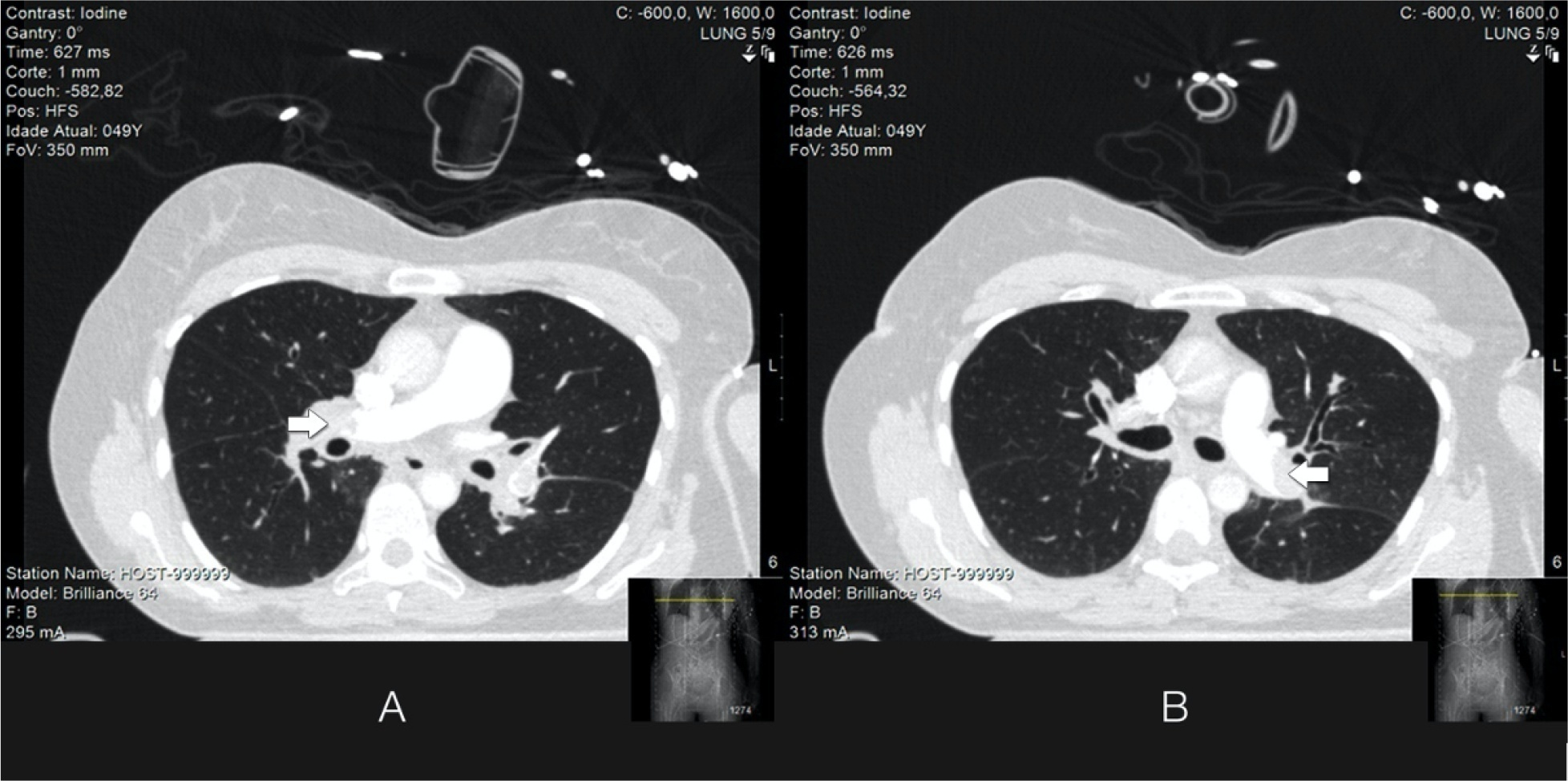
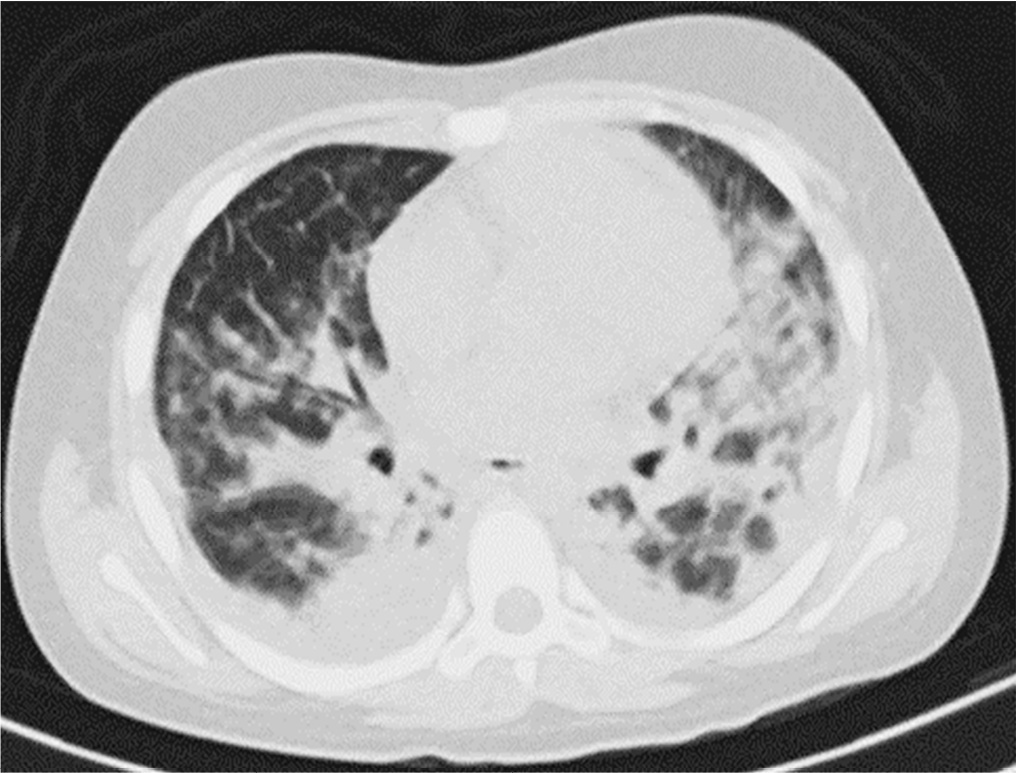
Spontaneous breathing can be deleterious in patients with previously injured lungs, especially in acute respiratory distress syndrome. Moreover, the failure to assume spontaneous breathing during mechanical ventilation and the need to switch back to controlled mechanical ventilation are associated with higher mortality. There is a gap of knowledge regarding which parameters might be useful to predict the risk of patient self-inflicted lung injury and to detect the inability to assume spontaneous breathing. We report a case of patient self-inflicted lung injury, the corresponding basic and advanced monitoring of the respiratory system mechanics and physiological and clinical results related to spontaneous breathing. The patient was a 33-year-old Caucasian man with a medical history of AIDS who developed acute respiratory distress syndrome and needed invasive mechanical ventilation after noninvasive ventilatory support failure. During the controlled ventilation periods, a protective ventilation strategy was adopted, and the patient showed clear clinical and radiographic improvement. However, during each spontaneous breathing period under pressure support ventilation, despite adequate initial parameters and a strictly adjusted ventilatory setting and monitoring, the patient developed progressive hypoxemia and worsening of respiratory system mechanics with a clearly correlated radiographic deterioration (patient self-inflicted lung injury). After failing three spontaneous breathing assumption trials, he died on day 29 due to refractory hypoxemia. Conventional basic and advanced monitoring variables in this case were not sufficient to identify the aptitude to breathe spontaneously or to predict the risk and development of patient self-inflicted lung injury during partial support ventilation.