Abstract
Rev Bras Ter Intensiva. 2016;28(4):444-451
DOI 10.5935/0103-507X.20160078
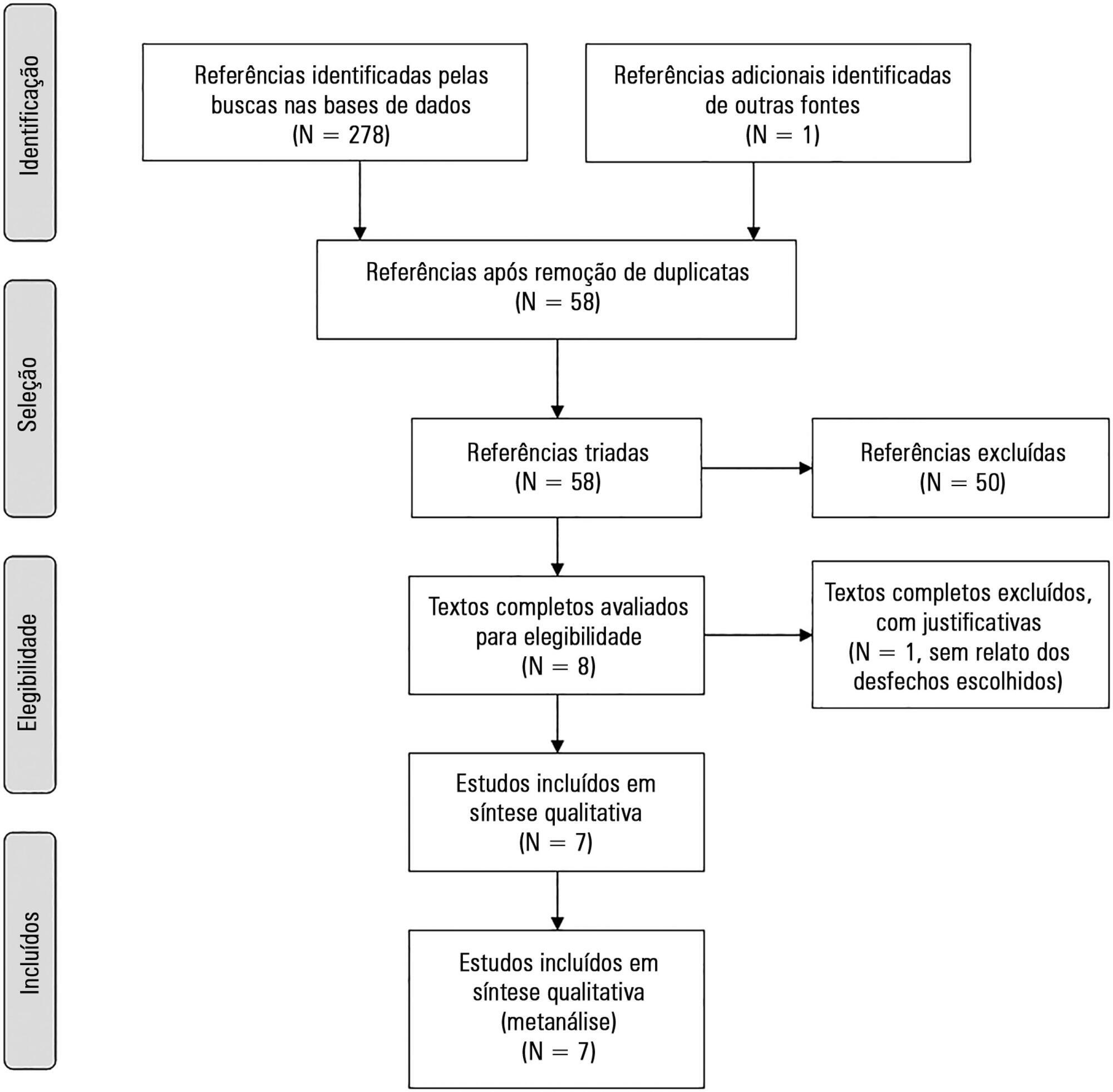
The aim of this study was to systematically review studies that compared a mild target sedation protocol with daily sedation interruption and to perform a meta-analysis with the data presented in these studies.
We searched Medline, Scopus and Web of Science databases to identify randomized clinical trials comparing sedation protocols with daily sedation interruption in critically ill patients requiring mechanical ventilation. The primary outcome was mortality in the intensive care unit.
Seven studies were included, with a total of 892 patients. Mortality in the intensive care unit did not differ between the sedation protocol and daily sedation interruption groups (odds ratio [OR] = 0.81; 95% confidence interval [CI] 0.60 - 1.10; I2 = 0%). Hospital mortality, duration of mechanical ventilation, intensive care unit and hospital length of stay did not differ between the groups either. Sedation protocols were associated with an increase in the number of days free of mechanical ventilation (mean difference = 6.70 days; 95%CI 1.09 - 12.31 days; I2 = 87.2%) and a shorter duration of hospital length of stay (mean difference = -5.05 days, 95%CI -9.98 - -0.11 days; I2 = 69%). There were no differences in regard to accidental extubation, extubation failure and the occurrence of delirium.
Sedation protocols and daily sedation interruption do not appear to differ in regard to the majority of analyzed outcomes. The only differences found were small and had a high degree of heterogeneity.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):252-259
DOI 10.5935/0103-507X.20150046
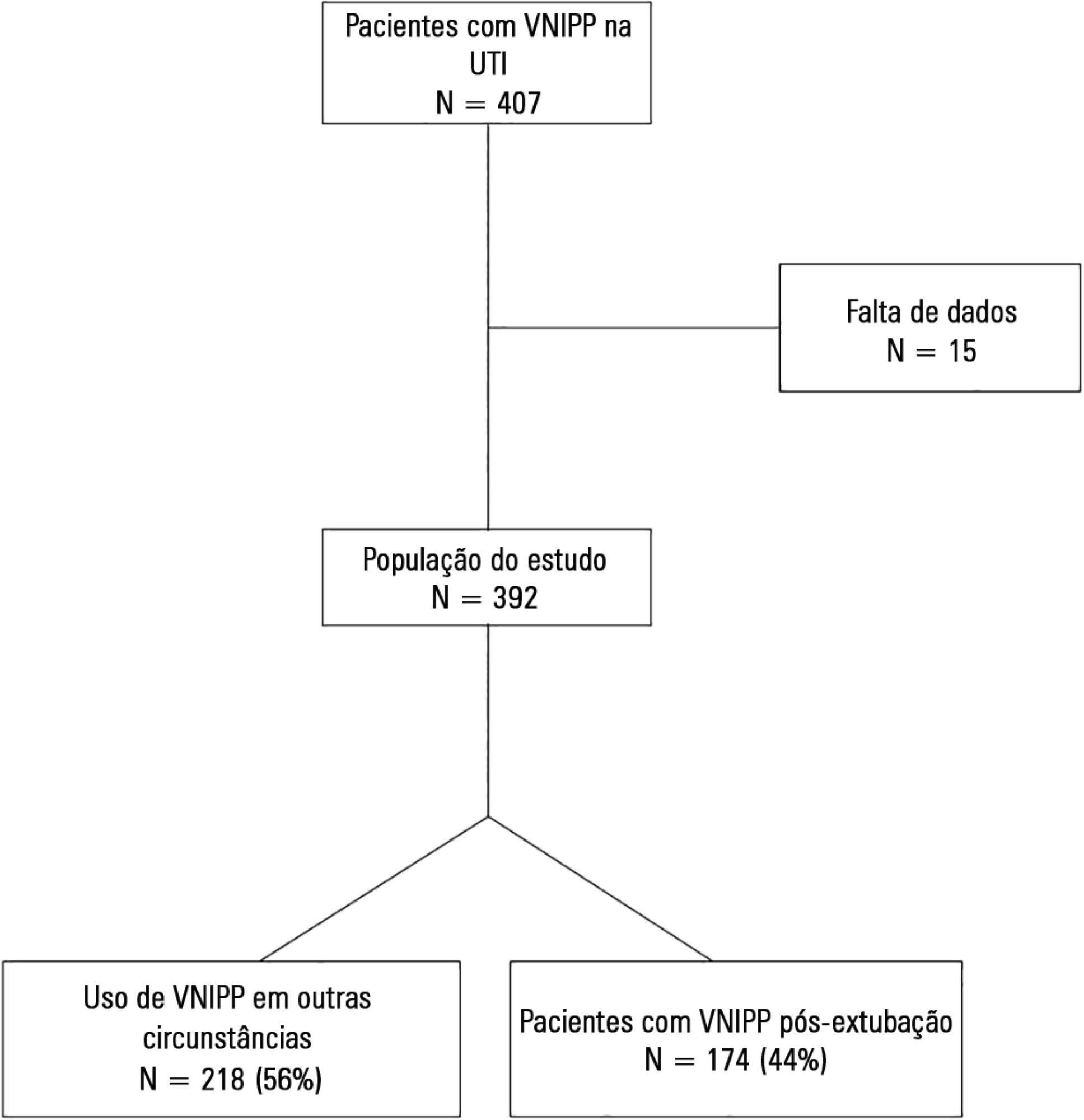
To describe postextubation noninvasive positive pressure ventilation use in intensive care unit clinical practice and to identify factors associated with noninvasive positive pressure ventilation failure.
This prospective cohort study included patients aged ≥ 18 years consecutively admitted to the intensive care unit who required noninvasive positive pressure ventilation within 48 hours of extubation. The primary outcome was noninvasive positive pressure ventilation failure.
We included 174 patients in the study. The overall noninvasive positive pressure ventilation use rate was 15%. Among the patients who used noninvasive positive pressure ventilation, 44% used it after extubation. The failure rate of noninvasive positive pressure ventilation was 34%. The overall mean ± SD age was 56 ± 18 years, and 55% of participants were male. Demographics; baseline pH, PaCO2 and HCO3; and type of equipment used were similar between groups. All of the noninvasive positive pressure ventilation final parameters were higher in the noninvasive positive pressure ventilation failure group [inspiratory positive airway pressure: 15.0 versus 13.7cmH2O (p = 0.015), expiratory positive airway pressure: 10.0 versus 8.9cmH2O (p = 0.027), and FiO2: 41 versus 33% (p = 0.014)]. The mean intensive care unit length of stay was longer (24 versus 13 days), p < 0.001, and the intensive care unit mortality rate was higher (55 versus 10%), p < 0.001 in the noninvasive positive pressure ventilation failure group. After fitting, the logistic regression model allowed us to state that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure compared with individuals with inspiratory positive airway pressure < 13.5 (OR = 3.02, 95%CI = 1.01 - 10.52, p value = 0.040).
The noninvasive positive pressure ventilation failure group had a longer intensive care unit length of stay and a higher mortality rate. Logistic regression analysis identified that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):205-211
DOI 10.5935/0103-507X.20150042
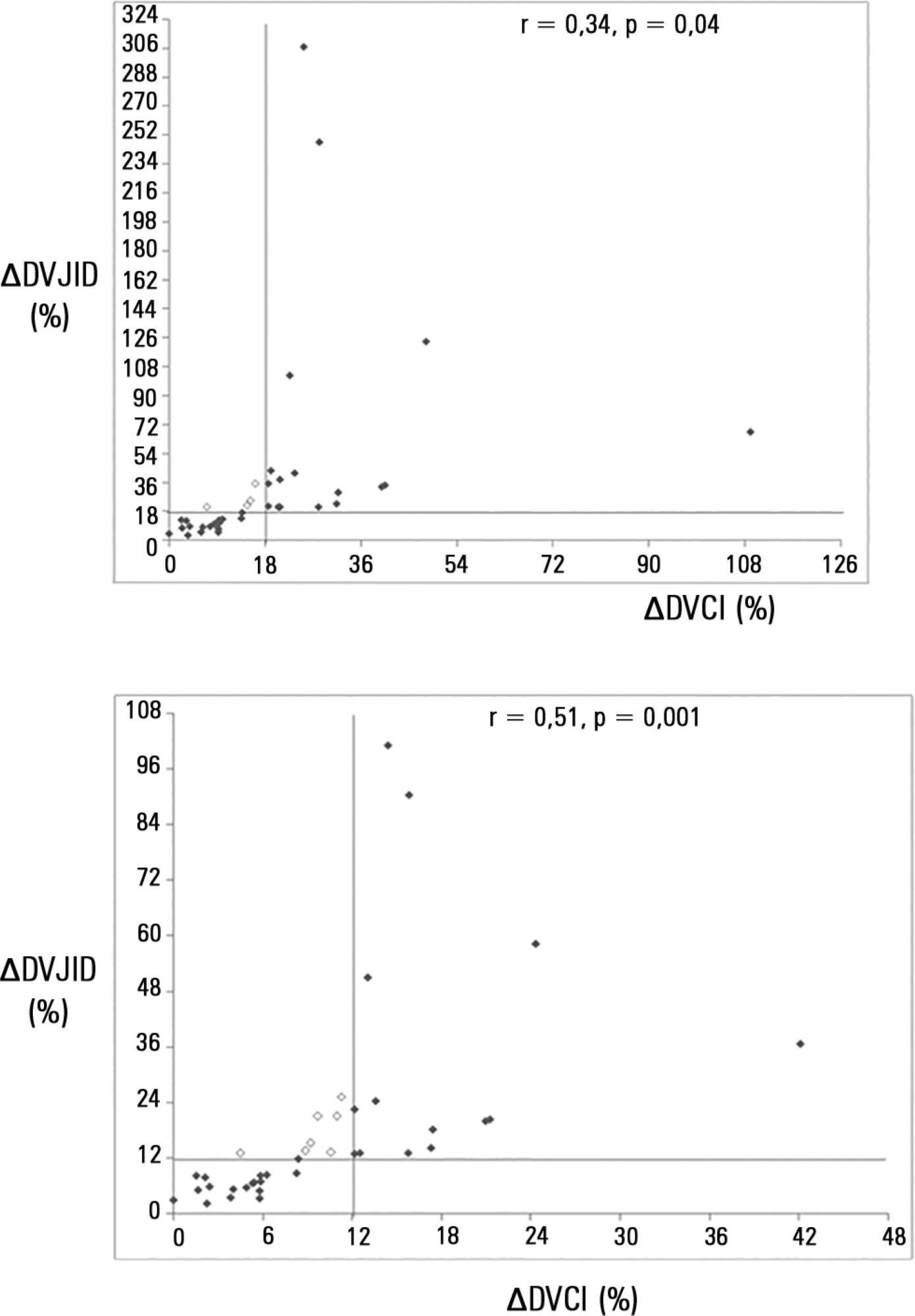
To investigate whether the respiratory variation of the inferior vena cava diameter (∆DIVC) and right internal jugular vein diameter (∆DRIJ) are correlated in mechanically ventilated patients.
This study was a prospective clinical analysis in an intensive care unit at a university hospital. Thirty-nine mechanically ventilated patients with hemodynamic instability were included. ∆DIVC and ∆DRIJ were assessed by echography. Vein distensibility was calculated as the ratio of (A) Dmax - Dmin/Dmin and (B) Dmax - Dmin/ mean of Dmax - Dmin and expressed as a percentage.
∆DIVC and ∆DRIJ were correlated by both methods: (A) r = 0.34, p = 0.04 and (B) r = 0.51, p = 0.001. Using 18% for ∆DIVC, indicating fluid responsiveness by method (A), 16 patients were responders and 35 measurements showed agreement (weighted Kappa = 0.80). The area under the ROC curve was 0.951 (95%CI 0.830 - 0.993; cutoff = 18.92). Using 12% for ∆DIVC, indicating fluid responsiveness by method (B), 14 patients were responders and 32 measurements showed agreement (weighted Kappa = 0.65). The area under the ROC curve was 0.903 (95%CI 0.765 - 0.973; cut-off value = 11.86).
The respiratory variation of the inferior vena cava and the right internal jugular veins are correlated and showed significant agreement. Evaluation of right internal jugular vein distensibility appears to be a surrogate marker for inferior vena cava vein distensibility for evaluating fluid responsiveness.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):212-219
DOI 10.5935/0103-507X.20150034
To evaluate the clinical characteristics of patients with hematological disease admitted to the intensive care unit and the use of noninvasive mechanical ventilation in a subgroup with respiratory dysfunction.
A retrospective observational study from September 2011 to January 2014.
Overall, 157 patients were included. The mean age was 45.13 (± 17.2) years and 46.5% of the patients were female. Sixty-seven (48.4%) patients had sepsis, and 90 (57.3%) patients required vasoactive vasopressors. The main cause for admission to the intensive care unit was acute respiratory failure (94.3%). Among the 157 studied patients, 47 (29.9%) were intubated within the first 24 hours, and 38 (24.2%) underwent noninvasive mechanical ventilation. Among the 38 patients who initially received noninvasive mechanical ventilation, 26 (68.4%) were subsequently intubated, and 12 (31.6%) responded to this mode of ventilation. Patients who failed to respond to noninvasive mechanical ventilation had higher intensive care unit mortality (66.7% versus 16.7%; p = 0.004) and a longer stay in the intensive care unit (9.6 days versus 4.6 days, p = 0.02) compared with the successful cases. Baseline severity scores (SOFA and SAPS 3) and the total leukocyte count were not significantly different between these two subgroups. In a multivariate logistic regression model including the 157 patients, intubation at any time during the stay in the intensive care unit and SAPS 3 were independently associated with intensive care unit mortality, while using noninvasive mechanical ventilation was not.
In this retrospective study with severely ill hematologic patients, those who underwent noninvasive mechanical ventilation at admission and failed to respond to it presented elevated intensive care unit mortality. However, only intubation during the intensive care unit stay was independently associated with a poor outcome. Further studies are needed to define predictors of noninvasive mechanical ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):266-273
DOI 10.5935/0103-507X.20150035
Acute respiratory distress syndrome is a disease of acute onset characterized by hypoxemia and infiltrates on chest radiographs that affects both adults and children of all ages. It is an important cause of respiratory failure in pediatric intensive care units and is associated with significant morbidity and mortality. Nevertheless, until recently, the definitions and diagnostic criteria for acute respiratory distress syndrome have focused on the adult population. In this article, we review the evolution of the definition of acute respiratory distress syndrome over nearly five decades, with a special focus on the new pediatric definition. We also discuss recommendations for the implementation of mechanical ventilation strategies in the treatment of acute respiratory distress syndrome in children and the use of adjuvant therapies.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):64-71
DOI 10.5935/0103-507X.20150011
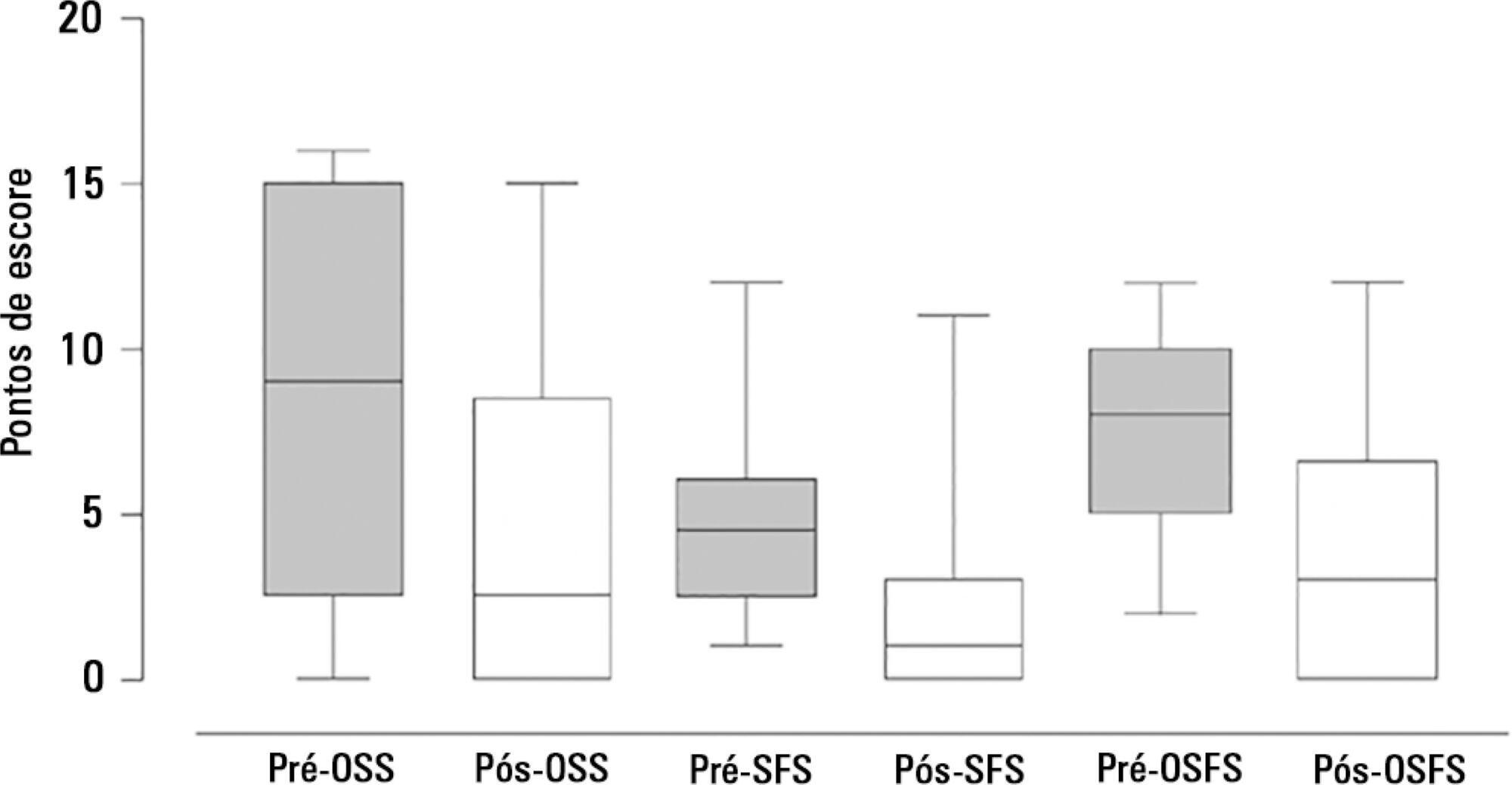
The aim of the present study was to assess the feasibility of the early implementation of a swallowing rehabilitation program in tracheostomized patients under mechanical ventilation with dysphagia.
This prospective study was conducted in the intensive care units of a university hospital. We included hemodynamically stable patients under mechanical ventilation for at least 48 hours following 48 hours of tracheostomy and with an appropriate level of consciousness. The exclusion criteria were previous surgery in the oral cavity, pharynx, larynx and/or esophagus, the presence of degenerative diseases or a past history of oropharyngeal dysphagia. All patients were submitted to a swallowing rehabilitation program. An oropharyngeal structural score, a swallowing functional score and an otorhinolaryngological structural and functional score were determined before and after swallowing therapy.
We included 14 patients. The mean duration of the rehabilitation program was 12.4 ± 9.4 days, with 5.0 ± 5.2 days under mechanical ventilation. Eleven patients could receive oral feeding while still in the intensive care unit after 4 (2 - 13) days of therapy. All scores significantly improved after therapy.
In this small group of patients, we demonstrated that the early implementation of a swallowing rehabilitation program is feasible even in patients under mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):119-124
DOI 10.5935/0103-507X.20150022
To evaluate the efficacy and safety of percutaneous tracheostomy by means of single-step dilation with fiber optic bronchoscopy assistance in critical care patients under mechanical ventilation.
Between the years 2004 and 2014, 512 patients with indication of tracheostomy according to clinical criteria, were prospectively and consecutively included in our study. One-third of them were high-risk patients. Demographic variables, APACHE II score, and days on mechanical ventilation prior to percutaneous tracheostomy were recorded. The efficacy of the procedure was evaluated according to an execution success rate and based on the necessity of switching to an open surgical technique. Safety was evaluated according to post-operative and operative complication rates.
The mean age of the group was 64 ± 18 years (203 women and 309 males). The mean APACHE II score was 21 ± 3. Patients remained an average of 11 ± 3 days on mechanical ventilation before percutaneous tracheostomy was performed. All procedures were successfully completed without the need to switch to an open surgical technique. Eighteen patients (3.5%) presented procedure complications. Five patients experienced transient desaturation, 4 presented low blood pressure related to sedation, and 9 presented minor bleeding, but none required a transfusion. No serious complications or deaths associated with the procedure were recorded. Eleven patients (2.1%) presented post-operative complications. Seven presented minor and transitory bleeding of the percutaneous tracheostomy stoma, 2 suffered displacement of the tracheostomy cannula, and 2 developed a superficial infection of the stoma.
Percutaneous tracheostomy using the single-step dilation technique with fiber optic bronchoscopy assistance seems to be effective and safe in critically ill patients under mechanical ventilation when performed by experienced intensive care specialists using a standardized procedure.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):155-160
DOI 10.5935/0103-507X.20150027
To evaluate the changes in ventilatory mechanics and hemodynamics that occur in patients dependent on mechanical ventilation who are subjected to a standard respiratory therapy protocol.
This experimental and prospective study was performed in two intensive care units, in which patients dependent on mechanical ventilation for more than 48 hours were consecutively enrolled and subjected to an established respiratory physiotherapy protocol. Ventilatory variables (dynamic lung compliance, respiratory system resistance, tidal volume, peak inspiratory pressure, respiratory rate, and oxygen saturation) and hemodynamic variables (heart rate) were measured one hour before (T-1), immediately after (T0) and one hour after (T+1) applying the respiratory physiotherapy protocol.
During the period of data collection, 104 patients were included in the study. Regarding the ventilatory variables, an increase in dynamic lung compliance (T-1 = 52.3 ± 16.1mL/cmH2O versus T0 = 65.1 ± 19.1mL/cmH2O; p < 0.001), tidal volume (T-1 = 550 ± 134mL versus T0 = 698 ± 155mL; p < 0.001), and peripheral oxygen saturation (T-1 = 96.5 ± 2.29% versus T0 = 98.2 ± 1.62%; p < 0.001) were observed, in addition to a reduction of respiratory system resistance (T-1 = 14.2 ± 4.63cmH2O/L/s versus T0 = 11.0 ± 3.43cmH2O/L/s; p < 0.001), after applying the respiratory physiotherapy protocol. All changes were present in the assessment performed one hour (T+1) after the application of the respiratory physiotherapy protocol. Regarding the hemodynamic variables, an immediate increase in the heart rate after application of the protocol was observed, but that increase was not maintained (T-1 = 88.9 ± 18.7 bpm versus T0 = 93.7 ± 19.2bpm versus T+1 = 88.5 ± 17.1bpm; p < 0.001).
Respiratory therapy leads to immediate changes in the lung mechanics and hemodynamics of mechanical ventilation-dependent patients, and ventilatory changes are likely to remain for at least one hour.