Abstract
Rev Bras Ter Intensiva. 2011;23(2):164-169
DOI 10.1590/S0103-507X2011000200008
OBJECTIVE: To evaluate the effects of hemodynamic, respiratory and metabolic changes on intracranial pressure in a model of acute lung injury and abdominal compartment syndrome. METHODS: Eight Agroceres pigs were submitted to five different clinical scenarios after instrumentation: 1) a baseline condition with low intra-abdominal pressure and healthy lungs; 2) pneumoperitoneum with 20 mmHg intra-abdominal pressure; 3) acute lung injury induced by pulmonary lavage with surfactant deactivation; 4) pneumoperitoneum with 20 mmHg intra-abdominal pressure with lung pulmonary injury and low positive end-expiratory pressure; and 5) 27 cmH2O positive end-expiratory pressure with pneumoperitoneum and acute lung injury. Respiratory and hemodynamic variables were collected. A multivariate analysis was conducted to search for variables associated with increased intracranial pressure in the five scenarios. RESULTS: Only plateau airway pressure showed a positive correlation with intracranial pressure in the multivariate analysis. In the models with acute lung injury, plateau airway pressure, CO2 arterial pressure, end tidal CO2 and central venous pressure were positively correlated with increased intracranial pressure. CONCLUSION: In a model of multiple organ dysfunction with associated clinical conditions causing increased intra-thoracic and abdominal pressure, increased intracranial pressure triggered by elevated intra-abdominal pressure is apparently caused by worsened respiratory system compliance and a reduced brain venous drainage gradient due to increased central venous pressure.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):190-198
DOI 10.1590/S0103-507X2011000200012
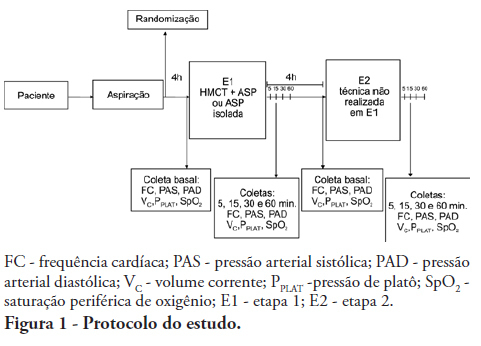
OBJECTIVES: To evaluate the effects of the manual hyperinflation with thoracic compression (MHTC) maneuver on the clearance of secretions, pulmonary mechanics, hemodynamics and oxygenation in mechanically ventilated patients. METHODS: This was a controlled, crossover study that included twenty patients who were under invasive ventilation for more than 48 hours. Four hours after the last airway suctioning procedure, the patients underwent the study interventions, Suction alone or MHTC plus Suction, in sequence at four hour intervals. The sequence order for the procedures was established by randomization. Data were collected before, during and 5, 15, 30 and 60 minutes after each intervention. The suctioned secretions were collected and weighed. RESULTS: No significant differences between the procedures were found regarding tidal volume, plateau pressure and pulmonary compliance (p>0.05). The hemodynamic variables showed increased pressures and heart rate during the procedures and returned to baseline values five minutes after the end of the procedure (p≤0.001). No significant hemodynamic differences were seen between the interventions (p>0.05). For the duration of the study, oxygen saturation was 99% with only two exceptions during the MHTC + Suction procedure, where saturation was 98% (p<0.05). No significant differences were observed between the techniques regarding the weight of the suctioned secretion. CONCLUSION: The results suggest that MHTC, as performed in this study, adds no benefit with respect to oxygenation optimization, pulmonary mechanics and clearance of secretions. However, the MHTC maneuver did not result in hemodynamic changes when compared to the suctioning procedure alone.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):199-206
DOI 10.1590/S0103-507X2011000200013
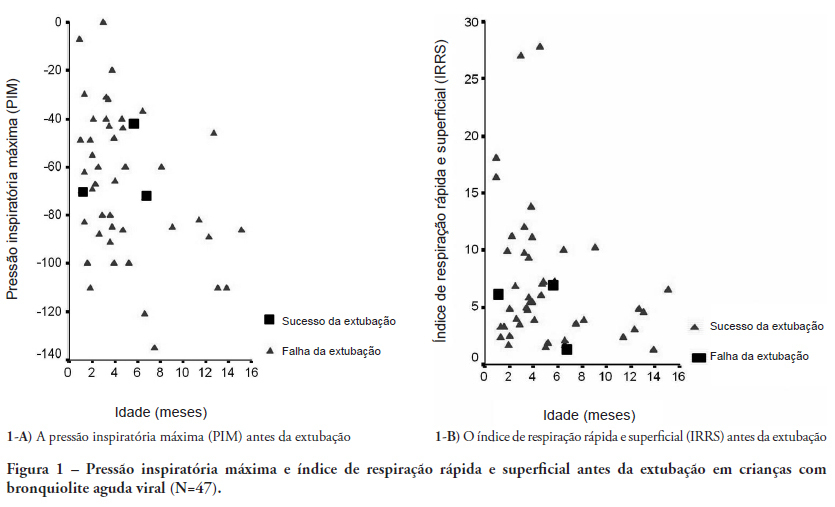
OBJECTIVES: Between 10% and 20% of children submitted to mechanical ventilation in the pediatric intensive care unit present extubation failure. Several ventilatory indexes have been proposed to predict extubation failure. The aim of this study was to analyze the accuracy of these indices in predicting successful extubation in children and to evaluate these variables according to the age of the patient and the specific disease. METHODS: A prospective observational study including all children submitted to mechanical ventilation in a Brazilian referral pediatric intensive care unit was conducted between August 2007 and August 2008. The tidal volume, maximal negative inspiratory pressure, rapid shallow breathing index and other ventilatory indexes were measured before extubation. These variables were analyzed according to the extubation outcome (success or failure) as well as age and specific disease (post cardiac surgery and acute viral bronchiolitis). RESULTS: A total of 100 patients were included (median age of 2.1 years old). Extubation failure was observed in 13% and was associated with lower weight (10.3+8.1 Kg vs. 5.5+2.4 Kg; p=0.01). We also evaluated the relationship between extubation failure and the main cause indicating mechanical ventilation: children who had received cardiac surgery (n=17) presented an extubation failure rate of 29.4% with a relative risk of 4.6 (1.2-17.2) when compared to children with acute viral bronchiolitis (n=47, extubation failure rate of 6.4%). The maximal inspiratory pressure was the only physiologic variable independently associated with the outcome. However, this variable showed a wide dispersion and lack of accuracy for predicting extubation success (sensitivity of 82% and specificity of 55% for a cut point of -37.5 cmH2O predicting successful extubation). The same wide dispersion was observed with other ventilatory indexes. CONCLUSION: The indexes for predicting extubation success in children submitted to mechanical ventilation are not accurate; they vary widely depending on age, main disease and other clinical aspects. New formulas including clinical variables should be developed for better prediction of extubation success in children submitted to mechanical ventilation
Abstract
Rev Bras Ter Intensiva. 2010;22(4):315-320
DOI 10.1590/S0103-507X2010000400001
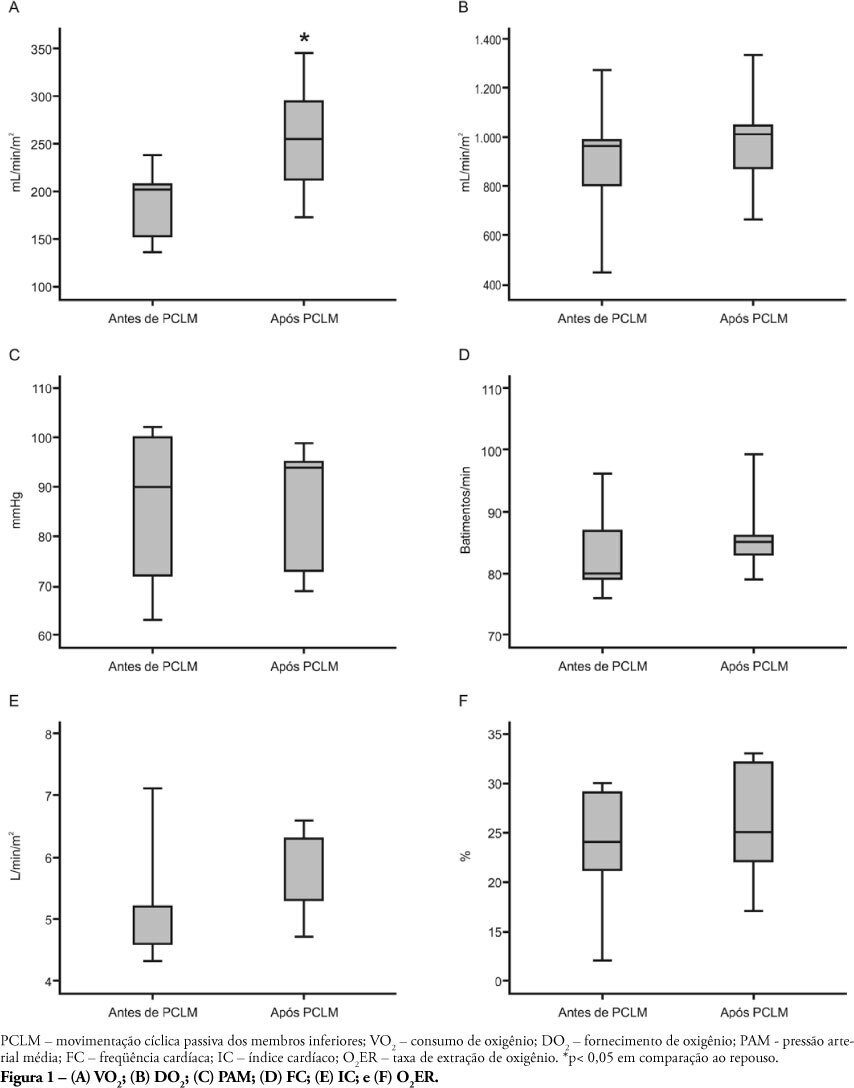
OBJECTIVE: Limb movements, passively performed by a physiotherapist, have been shown to result in significant increases in critically ill patients' metabolic and hemodynamic variables. This study objective was to determine whether passive cycling leg movement increases hemodynamic and metabolic variables in sedated mechanical ventilation dependent patients. METHODS: Five sedated mechanical ventilation dependent patients in a 18-bed intensive care unit of a university hospital were evaluated. Passive cycling leg movements were performed for 10min at a 30 movements/min rate. Complete hemodynamical data were recorded and arterial and mixed venous blood sample were collected 5 minutes before and after 5 minutes after the maneuver completion. RESULTS: All patients had increased oxygen consumption (VO2). The VO2 increase occurred with a concomitant drop in mixed venous blood saturation (SvO2), likely from both oxygen extraction ratio (O2ER) and cardiac index (CI) increase. CONCLUSION: passive cycling leg movements may influence hemodynamical and metabolic status in sedated mechanical ventilation-dependent patients.
Abstract
Rev Bras Ter Intensiva. 2010;22(4):333-338
DOI 10.1590/S0103-507X2010000400004
OBJECTIVES: To describe the clinical features and outcomes of patients admitted with influenza A (H1N1) infection in two private hospitals' intensive care units in São Paulo, Brazil, during the 2009 pandemics. METHODS: A retrospective cohort study was conducted to evaluate demographic data, initial clinical presentation, prognostic scores [Simplified Acute Physiology Score (SAPS) 3 and Sequential Organ Failure Assessment (SOFA)], comorbidities, outcomes and treatment of patients with confirmed pandemic influenza diagnosis from July to September 2009. RESULTS: 22 patients were admitted. Median age was 30 (25-43.5) years. Median SAPS 3 and SOFA were 42 (37-49) and 2 (1-3.5), respectively. Comorbidities were common (45.4%), especially obesity (22.7%). Two (9.1%) patients were pregnant. Five (22.7%) patients required invasive mechanical ventilation, with high positive end expiratory pressures (median of 16 cmH2O, interquartile range 10-25cmH2O). There was a 50% incidence of non-invasive ventilation failure. Most (77.2%) of patients were treated with oseltamivir. Hospital mortality was 4.5%. Initial SAPS 3, SOFA and PaO2/FiO2 ratio were associated with mechanical ventilation requirement (p<0.01). CONCLUSIONS: Pandemic influenza infection mainly affected young and obese patients. In this study, patients were less severe than those previously described, what explains our low mortality and mechanical ventilation needs. However, high positive end expiratory pressures were required for mechanically ventilated patients.
Abstract
Rev Bras Ter Intensiva. 2010;22(4):363-368
DOI 10.1590/S0103-507X2010000400009
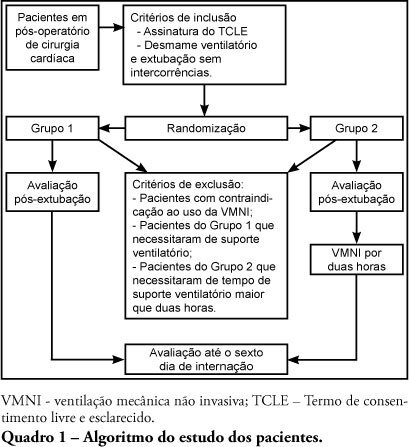
BACKGROUND: : Noninvasive ventilation is routine in acute respiratory failure patients; nevertheless, the literature is controversial for its use in cardiac surgery postoperative period. OBJECTIVE: To evaluate the effectiveness of preventive noninvasive ventilation in the immediate postoperative period of cardiac surgery, monitoring its impact until the sixth day of hospitalization. METHODS: This was a controlled study, where patients in immediate postoperative period of cardiac surgery were randomized into two groups: control (G1) and investigational (G2) which received noninvasive ventilation set on pressure support mode and positive end expiratory pressure, for 2 hours following extubation. Were evaluated ventilatory, hemodynamical and oxygenation variables both immediately after extubation and after noninvasive ventilation in G2. RESULTS: Thirty-two patients completed the study, 18 in G1 and 14 in G2. The mean age was 61±16.23 years for G1 and for G2 61.5 ± 9.4 years. Of the initial twenty-seven patients in G1, nine patients (33.3%) were excluded due to invasive ventilation requirements, and three patients (11.11%) had to go back to invasive mechanical ventilation. None of the 14 G2 patients was reintubated. Patients undergoing early ventilatory support showed better results in the assessments throughout the hospitalization time. CONCLUSION: Noninvasive post-cardiac surgery ventilation was proven effective, as demonstrated by increased vital capacity, decreased respiratory rate, prevention of post-extubation acute respiratory failure and reduced reintubation rates.
Abstract
Rev Bras Ter Intensiva. 2010;22(4):375-383
DOI 10.1590/S0103-507X2010000400011
Respiratory failure after cardiopulmonary bypass heart surgery can result from many pre-, intra- or postoperative respiratory system-related factors. This review was aimed to discuss some factors related to acute lung injury observed during the postoperative period of cardiac surgery and the mechanical ventilation modalities which should be considered to prevent hypoxemia.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):159-165
DOI 10.1590/S0103-507X2010000200010
OBJECTIVE: Neonates mechanic ventilation weaning has become a major clinical challenge, and constitutes a large portion of neonatal intensive care units workload. The spontaneous breathing trial (SBT), performed immediately before extubation, can provide useful information on the patient's spontaneous breathing ability. This study aimed to assess the SBT effectiveness for extubation success prediction in mechanically ventilated preterm infants. METHODS: After Ethics Committee approval, an observational, longitudinal, prospective study was conducted. A sample of 60 preterm infants compliant with the weaning criteria was categorized in two groups: 'SBT' group (n=30), with the patients who underwent 30 minutes spontaneous breathing trial (SBT) with continuous positive pressure airway (CPAP), and the control group (n=30) where the extubation was performed without spontaneous breathing trial. The heart rate (HR), respiratory rate (RR), pulse oxymetry oxygen saturation (SpO2) and the Silverman-Andersen score were recorded before and 10, 20 and 30 minutes after the spontaneous breathing trial. Were also assessed for both groups, and versus extubation success or failure, the weight, gestational age, Apgar score, mean airway pressure, inspired oxygen concentration, and tracheal tube time. The Chi-square test was used for categorical variables and the Mann-Whitney test for non-normal distribution. Extubation success was defined as a 48 hours period with no reintubation requirement. RESULTS: No significant differences were identified between the groups for the analyzed variables, except for the mean airway pressure. A significant association was shown between spontaneous breathing trial and successful extubation. CONCLUSION: The significant association between SBT and extubation success may contribute for prediction of successful weaning in preterm infants.