Abstract
Rev Bras Ter Intensiva. 2017;29(3):331-336
DOI 10.5935/0103-507X.20170040
The goal was to determine the main drug-related problems in neonates who were using antimicrobials.
This was an observational, prospective and longitudinal study. Drug-related problems were classified according to version 6.2 of the Pharmaceutical Care Network Europe Foundation classification. A descriptive analysis was performed, in which the clinical and therapeutic variables were presented as absolute and relative frequencies or as the mean and standard deviation, as appropriate.
In total, 152 neonates with a predominance of males (58.5%), gestational age of 32.7 ± 4.2 weeks and weight of 1,903.1 ± 846.9g were included. The main diagnostic hypothesis of infection was early sepsis (66.5%), and 71.7% of the neonates had some risk factor for infection. Among the neonates, 33.6% had at least one drug-related problem. Of these, 84.8% were related to treatment effectiveness and 15.2% to adverse reactions. The main cause of drug-related problems was the selected dose, particularly for aminoglycosides and cephalosporins.
The use of antimicrobials in the neonatal intensive care is mainly associated with problems related to medication effectiveness, predominantly the prescription of subdoses of antimicrobials, especially aminoglycosides.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):230-235
DOI 10.1590/S0103-507X2012000300005
OBJECTIVE: This study established the incidence and primary causes of unplanned extubation in newborns in the neonatal intensive care units of the Hospital Sofia Feldman, Belo Horizonte (Minas Gerais). METHODS: This retrospective study was conducted between July 1, 2009 and April 30, 2010. Unplanned extubations and their primary causes were assessed using an adverse events form. The following variables were assessed: gender, corrected age, present weight, duration of mechanical ventilation time, and motives/causes of the event on the day of the unplanned extubation event. RESULTS: Fifty-four unplanned extubations occurred, which corresponded to an incidence of 1.0 event/100 days of mechanical ventilation. This rate was higher among newborns with a corrected age of 30 to 36 weeks and weight < 1,000 g. The primary causes of unplanned extubations included patient agitation, inappropriate handling of patients during the performance of procedures, and inappropriate fixation and positioning of the endotracheal tube. CONCLUSION: The incidence of unplanned extubation in the investigated neonatal intensive care units was low during the study period compared to previously reported data. Nevertheless, the assessment of the quality of procedures, the continuous follow-up of newborns, and the monitoring of the causes of extubation are required to further reduce this incidence.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):79-85
DOI 10.1590/S0103-507X2012000100012
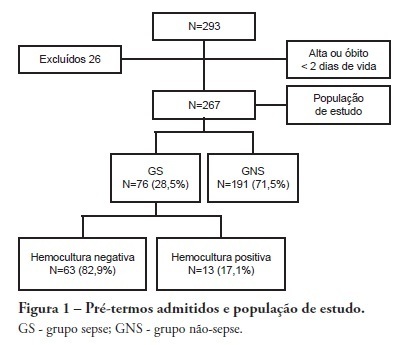
OBJECTIVE: To evaluate the prevalence factors and etiologies associated with late neonatal sepsis in preterm neonates in a neonatal intensive care unit. METHODS: This was a cross-sectional study of secondary data pertaining to preterm neonates admitted to the neonatal intensive care unit between 2008 and 2010 and was gathered from medical charts. The outcome variable, late neonatal sepsis, was characterized using the Brazilian national health surveillance agency criteria. Pearson's Chi-squared test, Fisher's exact test and the linear trend Chi-squared test were used to assess the qualitative variables for linear trends. The statistical significance level was set at p < 0.05. Bivariate and multivariate analyses of the independent and dependent variables were conducted to obtain a measure of the effect and prevalence ratios, considering a p-value of less than 0.20 to indicate statistical significance. RESULTS: This study included 267 preterm neonates. Of the participants, 28.5% were characterized as having late-onset sepsis. Positive blood cultures were recorded for 17.1% of the neonates. Death occurred in 8.2% of the total cases, and of these deaths, 68.2% occurred within the sepsis group. Three deaths were associated with positive blood cultures, all of which grew Gram-negative bacteria. The bivariate analysis demonstrated that as the gestational age and birth weight decreased, the prevalence of late-onset sepsis trended upward. Ten or more days on mechanical ventilation was associated with late-onset neonatal sepsis in 80.8% of cases. Peripherally inserted central catheters left in place for 11 or more days were associated with late-onset neonatal sepsis in 76.2% of cases. The multivariate analysis demonstrated that a peripherally inserted catheter left in place for less than 11 days was associated with late-onset neonatal sepsis. Gram-negative bacteria, including Klebsiella pneumoniae and Escherichia coli, were the most frequent causative agents. CONCLUSIONS: Late sepsis remains a concern because of its prevalence in intensive care units and because it increases the number of invasive procedures that preterm children usually undergo in these units. The authors emphasize the expanding role of Gram-negative bacteria in late-onset neonatal sepsis and the need for more efficient methods to identify confirmed sepsis.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):30-34
DOI 10.1590/S0103-507X2012000100005
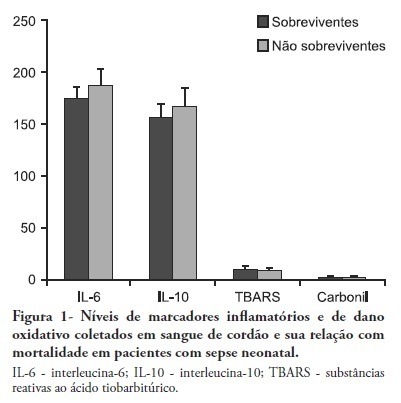
OBJECTIVES: Neonatal sepsis is a complex syndrome involving an uncontrolled systemic inflammatory response associated with an infection. It may result in the dysfunction or failure of one or more organs or even death. Given its high incidence in premature neonates, the identification of prognostic factors to optimize the early diagnosis and therapeutic interventions are highly desirable. This objective study determine the relationship between inflammatory markers and oxidative parameters as prognostic factors in early neonatal sepsis. METHODS: We conducted a prospective observational study by collecting data from 120 patients in the maternity unit of a university hospital. Preterm (<37 weeks of pregnancy) infants with at least one additional risk factor for neonatal sepsis were included. The levels of interleukin (IL)-6, IL-10, thiobarbituric acid reactive species (TBARS) and protein carbonyls and their association with sepsis severity were determined in the cord blood. RESULTS: Levels of IL-6 and TBARS, but not IL-10 and protein carbonyls, demonstrated a mild to moderate correlation with the SNAPPE-II severity score (r=0.435, p=0.02 and r = 0.385, p = 0.017, respectively). No correlations were found between these markers and mortality. CONCLUSION: TBARS and IL-6 have a mild to moderate correlation with SNAPPE-II, but none of the studied markers were able to predict mortality in our sample.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):462-469
DOI 10.1590/S0103-507X2011000400011
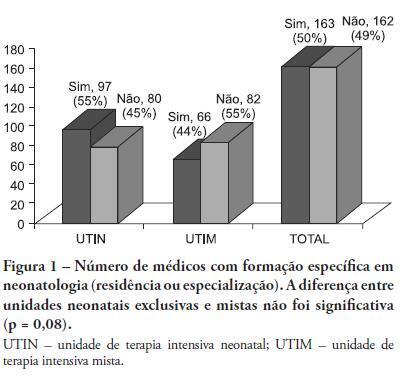
OBJECTIVE: This study described the sociodemographic profile and professional qualifications of pediatric intensive care physicians in the State of Rio de Janeiro (RJ), southeastern Brazil. METHODS: This investigation was an observational, cross-sectional and descriptive study that was conducted in neonatal, pediatric and mixed intensive care units in the State of Rio de Janeiro. Physicians working in the participating intensive care units voluntarily completed a semistructured and anonymous questionnaire. Questionnaires that were not returned within 30 days were considered lost, and questionnaires with less than 75% questions completed were excluded. The differences in neonatal and pediatric intensive care physicians' medical training were compared using the Chi-squared test with a 5% significance level. RESULTS: A total of 410 physicians were included in this study: 84% female, 48% between 30 and 39 years old and 45% with monthly incomes between US $1,700 to 2,700. Forty percent of these physicians worked exclusively in this specialty, and 72% worked in more than one intensive care unit. Only 50% of the participants had received specific training (either medical residency or specialization) in neonatology, and only 33% were board-certified specialists in this area. Only 27% of the physicians had received specific training in pediatric intensive care medicine, and only 17% were board-certified specialists (p < 0.0005 for both comparisons). Most (87%) physicians had participated in scientific events within the past 5 years, and 55% used the internet for continued medical education. However, only 25% had participated in any research. Most (63%) physicians were dissatisfied with their professional activity; 49% were dissatisfied due to working conditions, 23% due to low incomes and 18% due to training-related issues. CONCLUSION: These results suggested that the medical qualifications of neonatal and pediatric intensive care physicians in the State of Rio de Janeiro, Brazil are inadequate, especially in pediatric intensive care medicine. A high level of dissatisfaction was reported, which may jeopardize the quality of medical assistance that is provided by these professionals.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):327-334
DOI 10.1590/S0103-507X2011000300011
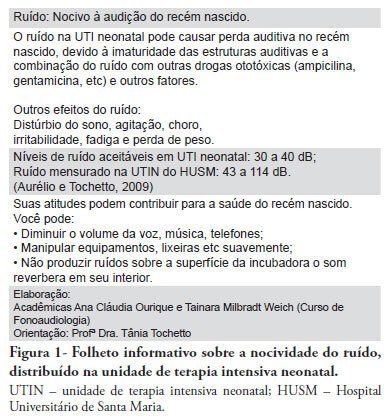
PURPOSE: To evaluate the effectiveness of a noise control program in the Neonatal Intensive Care Unit of the Hospital Universitário Santa Maria (NICU-HUSM) in Santa Maria, Rio Grande do Sul, Brazil. METHODS: NICU-HUSM professionals were initially contacted through informal interviews during the morning, afternoon and night shifts. Leaflets were delivered and posters were installed to raise awareness of the harmful effects of noise on neonates and professionals and to suggest behavioral changes to reduce noise levels. The suggestions included avoiding loud talking, careful handling of the incubator doors and keeping mobile phones on silent mode. One month later, questionnaires were used to assess behavioral changes since the first contact. RESULTS: Most of the professionals rated the NICU-HUSM noise level as moderate. Overall, 71.4% of the respondents acknowledged that their behaviors were noisy. The entire sample reported believing that the unit noise levels could be reduced by speaking lower, reacting more quickly to alarms and handling furniture more carefully. The NICU professionals reported adopting these behaviors. CONCLUSION: This noise control program was considered successful because the professionals became aware of the level of noise and adopted behavioral changes to avoid generating unnecessary noise.
Abstract
Rev Bras Ter Intensiva. 2008;20(3):261-266
DOI 10.1590/S0103-507X2008000300009
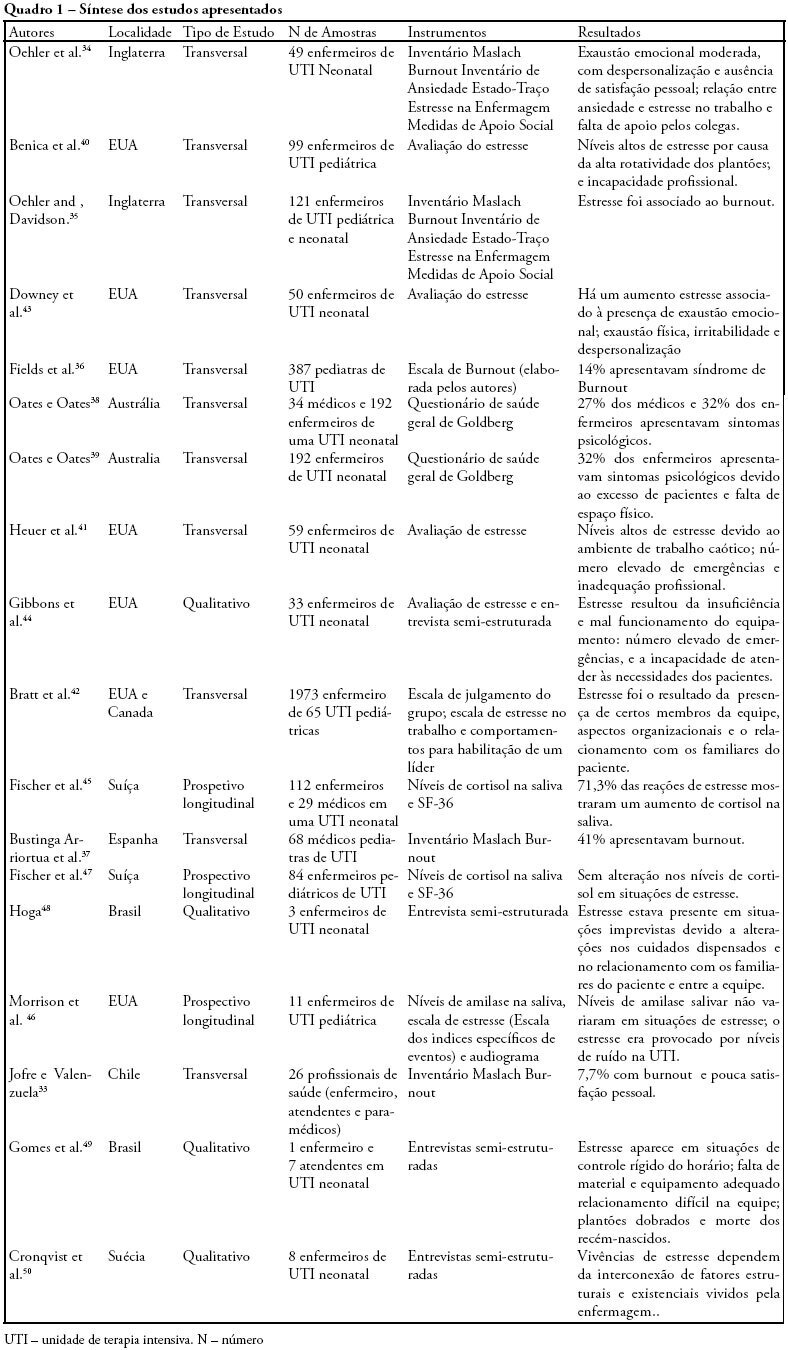
OBJECTIVES: Bibliographic review on occupational stress and burnout presence in physicians and nurses that work in pediatric and neonatal intensive care units. METHODS: The articles were selected from the MedLine, LILACS and SciElo data base using the key words: stress, burnout, physicians, nursing, intensive care unit, pediatric intensive care unit and neonatal intensive care unit. The studied period ranged from 1990 to 2007. RESULTS: Health professionals who work in pediatric and neonatal intensive care units are strong candidates for developing stress, psychological alterations and burnout syndrome. Researches on this subject identified important alterations suffered by these physicians and nurses, such as: work overload, burnout, desires of giving up their jobs, high levels of cortisol, among other alterations. CONCLUSIONS: Professionals, who work in pediatric and neonatal intensive care units, due to the specificity of their job, are liable to develop occupational stress, and consequently burnout. These results suggest the need for further research with the objective of developing preventive measures and intervention models.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)