Abstract
Crit Care Sci. 2023;35(2):168-176
DOI 10.5935/2965-2774.20230410-pt
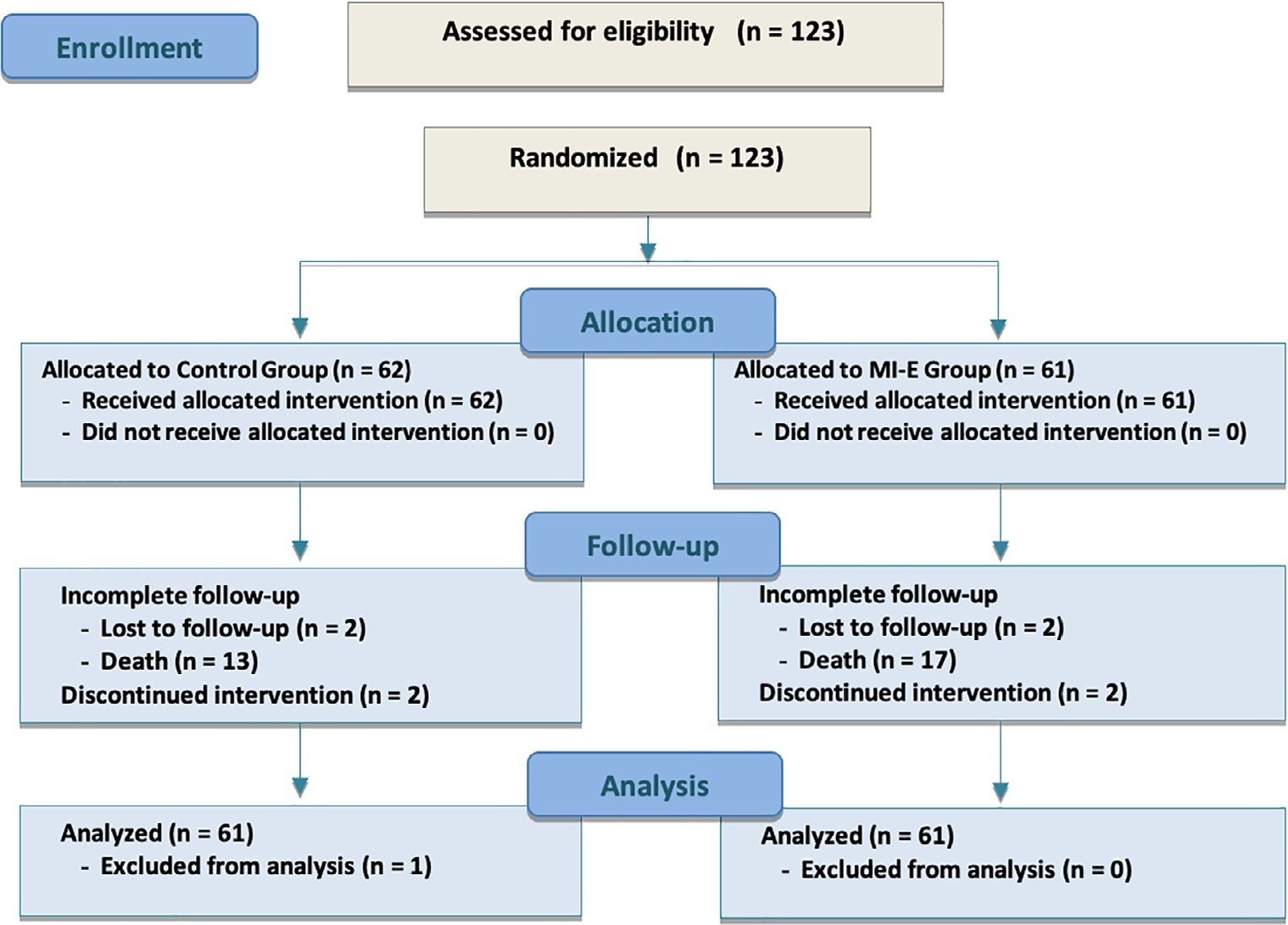
We hypothesized that the use of mechanical insufflation-exsufflation can reduce the incidence of acute respiratory failure within the 48-hour post-extubation period in intensive care unit-acquired weakness patients.
This was a prospective randomized controlled open-label trial. Patients diagnosed with intensive care unit-acquired weakness were consecutively enrolled based on a Medical Research Council score ≤ 48/60. The patients randomly received two daily sessions; in the control group, conventional chest physiotherapy was performed, while in the intervention group, chest physiotherapy was associated with mechanical insufflation-exsufflation. The incidence of acute respiratory failure within 48 hours of extubation was evaluated. Similarly, the reintubation rate, intensive care unit length of stay, mortality at 28 days, and survival probability at 90 days were assessed. The study was stopped after futility results in the interim analysis.
We included 122 consecutive patients (n = 61 per group). There was no significant difference in the incidence of acute respiratory failure between treatments (11.5% control group versus 16.4%, intervention group; p = 0.60), the need for reintubation (3.6% versus 10.7%; p = 0.27), mean length of stay (3 versus 4 days; p = 0.33), mortality at Day 28 (9.8% versus 15.0%; p = 0.42), or survival probability at Day 90 (21.3% versus 28.3%; p = 0.41).
Mechanical insufflation-exsufflation combined with chest physiotherapy seems to have no impact in preventing postextubation acute respiratory failure in intensive care unit-acquired weakness patients. Similarly, mortality and survival probability were similar in both groups. Nevertheless, given the early termination of the trial, further clinical investigation is strongly recommended.
Abstract
Crit Care Sci. 2023;35(2):196-202
DOI 10.5935/2965-2774.20230036-pt
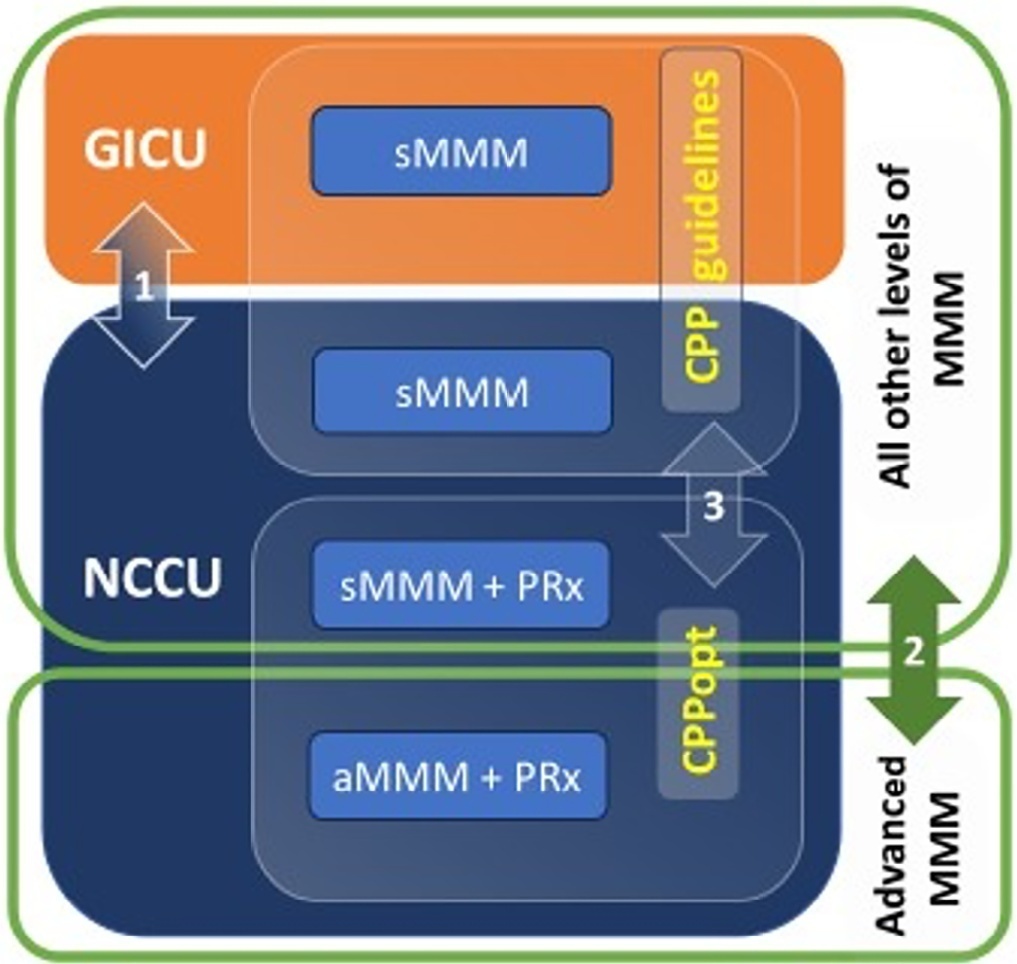
To evaluate the association between different intensive care units and levels of brain monitoring with outcomes in acute brain injury.
Patients with traumatic brain injury and subarachnoid hemorrhage admitted to intensive care units were included. Neurocritical care unit management was compared to general intensive care unit management. Patients managed with multimodal brain monitoring and optimal cerebral perfusion pressure were compared with general management patients. A good outcome was defined as a Glasgow outcome scale score of 4 or 5.
Among 389 patients, 237 were admitted to the neurocritical care unit, and 152 were admitted to the general intensive care unit. Neurocritical care unit management patients had a lower risk of poor outcome (OR = 0.228). A subgroup of 69 patients with multimodal brain monitoring (G1) was compared with the remaining patients (G2). In the G1 and G2 groups, 59% versus 23% of patients, respectively, had a good outcome at intensive care unit discharge; 64% versus 31% had a good outcome at 28 days; 76% versus 50% had a good outcome at 3 months (p < 0.001); and 77% versus 58% had a good outcome at 6 months (p = 0.005). When outcomes were adjusted by SAPS II severity score, using good outcome as the dependent variable, the results were as follows: for G1 compared to G2, the OR was 4.607 at intensive care unit discharge (p < 0.001), 4.22 at 28 days (p = 0.001), 3.250 at 3 months (p = 0.001) and 2.529 at 6 months (p = 0.006). Patients with optimal cerebral perfusion pressure management (n = 127) had a better outcome at all points of evaluation. Mortality for those patients was significantly lower at 28 days (p = 0.001), 3 months (p < 0.001) and 6 months (p = 0.001).
Multimodal brain monitoring with autoregulation and neurocritical care unit management were associated with better outcomes and should be considered after severe acute brain injury.
Abstract
Crit Care Sci. 2023;35(1):31-36
DOI 10.5935/2965-2774.20230113-pt
To evaluate the impact of an educational website on satisfaction and symptoms of anxiety and depression among family members of critically ill adult patients.
We embedded an analysis of website access in a cohort study conducted in intensive care units with flexible visiting hours in Brazil. Family members were guided to access an educational website designed to help them understand the processes and emotions associated with an intensive care unit stay. Subjects were evaluated for baseline data within the first 48 hours following enrollment and outcome assessment at up to 7 days after patient discharge from the intensive care unit, death, or until the 30th day of the study. The main outcomes were satisfaction using the Critical Care Family Needs Inventory and the presence of anxiety and depression symptoms using the Hospital Anxiety and Depression Scale.
A total of 532 family members were evaluated during the study period. Of these, 61 (11.5%) accessed the website. After adjustments, family members who accessed the website had significantly better mean Critical Care Family Needs Inventory scores (152.8 versus 145.2, p = 0.01) and a lower prevalence of probable clinical anxiety (prevalence ratio 0.35; 95%CI 0.14 - 0.89) than family members who did not access the website. There were no differences regarding symptoms of depression.
Access to an educational website was associated with higher family satisfaction with care and a lower prevalence of clinical anxiety.
Abstract
Crit Care Sci. 2023;35(1):73-83
DOI 10.5935/2965-2774.20230374-pt
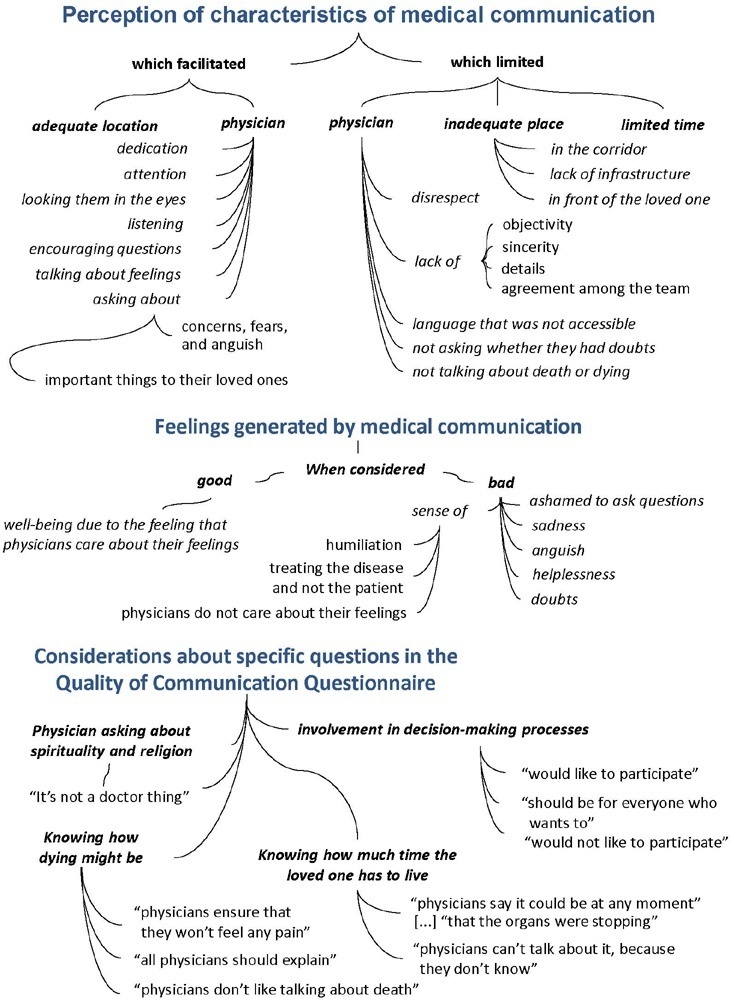
To understand the perception of medical communication and needs of family members with loved ones in intensive care.
The study was mainly qualitative and exploratory, with thematic analysis of comments made by 92 family members with loved ones in intensive care units when answering in-person interviews comprising the Quality of Communication Questionnaire (QoC) and open-ended questions about their need for additional help, the appropriateness of the place where they received information, and additional comments.
The participants’ mean age was 46.8 years (SD = 11.8), and most of them were female, married and had incomplete or completed elementary education. The following themes were found: perception of characteristics of medical communication; feelings generated by communication; considerations about specific questions in the QoC; family members’ needs; and strategies to overcome needs regarding communication. Characteristics that facilitated communication included attention and listening. Characteristics that made communication difficult included aspects of information sharing, such as inaccessible language; lack of clarity, objectivity, sincerity, and agreement among the team; limited time; and inadequate location. Feelings such as shame, helplessness, and sadness were cited when communication was inadequate. Family members’ needs related to communication included more details about the loved one’s diagnosis, prognosis, and health condition; participation in decisionmaking; and being asked about feelings, spirituality, dying and death. Others were related to longer visitation time, psychological support, social assistance, and better infrastructure.
It is necessary to enhance medical communication and improve hospital infrastructure to improve the quality of care for family members.
Abstract
Crit Care Sci. 2023;35(1):84-96
DOI 10.5935/2965-2774.20230405-pt
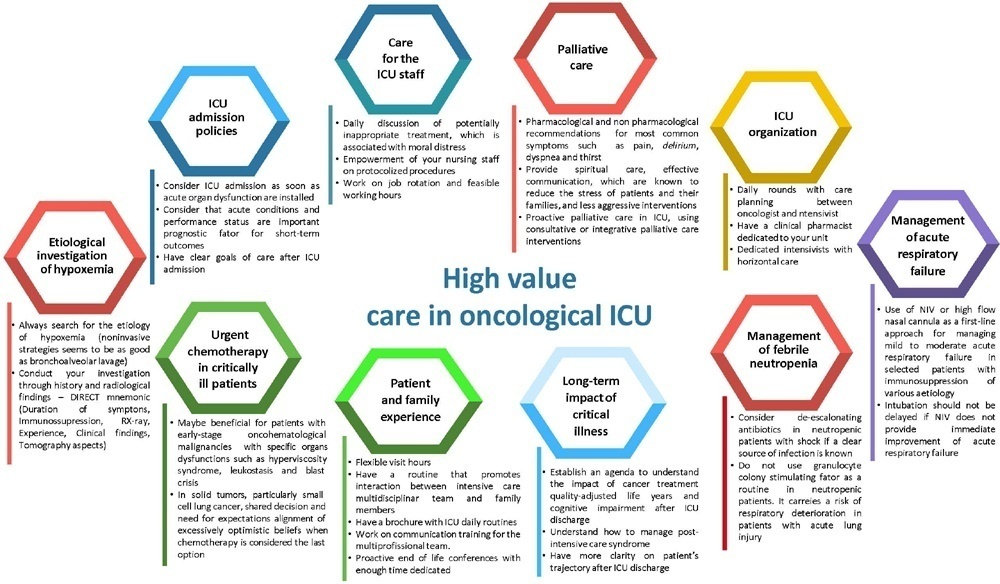
The number of patients with cancer requiring intensive care unit admission is increasing around the world. The improvement in the pathophysiological understanding of this group of patients, as well as the increasingly better and more targeted treatment options for their underlying disease, has led to a significant increase in their survival over the past three decades. Within the organizational concepts, it is necessary to know what adds value in the care of critical oncohematological patients. Practices in medicine that do not benefit patients and possibly cause harm are called low-value practices, while high-value practices are defined as high-quality care at relatively low cost. In this article, we discuss ten domains with high-value evidence in the care of cancer patients: (1) intensive care unit admission policies; (2) intensive care unit organization; (3) etiological investigation of hypoxemia; (4) management of acute respiratory failure; (5) management of febrile neutropenia; (6) urgent chemotherapy treatment in critically ill patients; (7) patient and family experience; (8) palliative care; (9) care of intensive care unit staff; and (10) long-term impact of critical disease on the cancer population. The disclosure of such policies is expected to have the potential to change health care standards. We understand that it is a lengthy process, and initiatives such as this paper are one of the first steps in raising awareness and beginning a discussion about high-value care in various health scenarios.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):469-476
DOI 10.5935/0103-507X.20220429-en
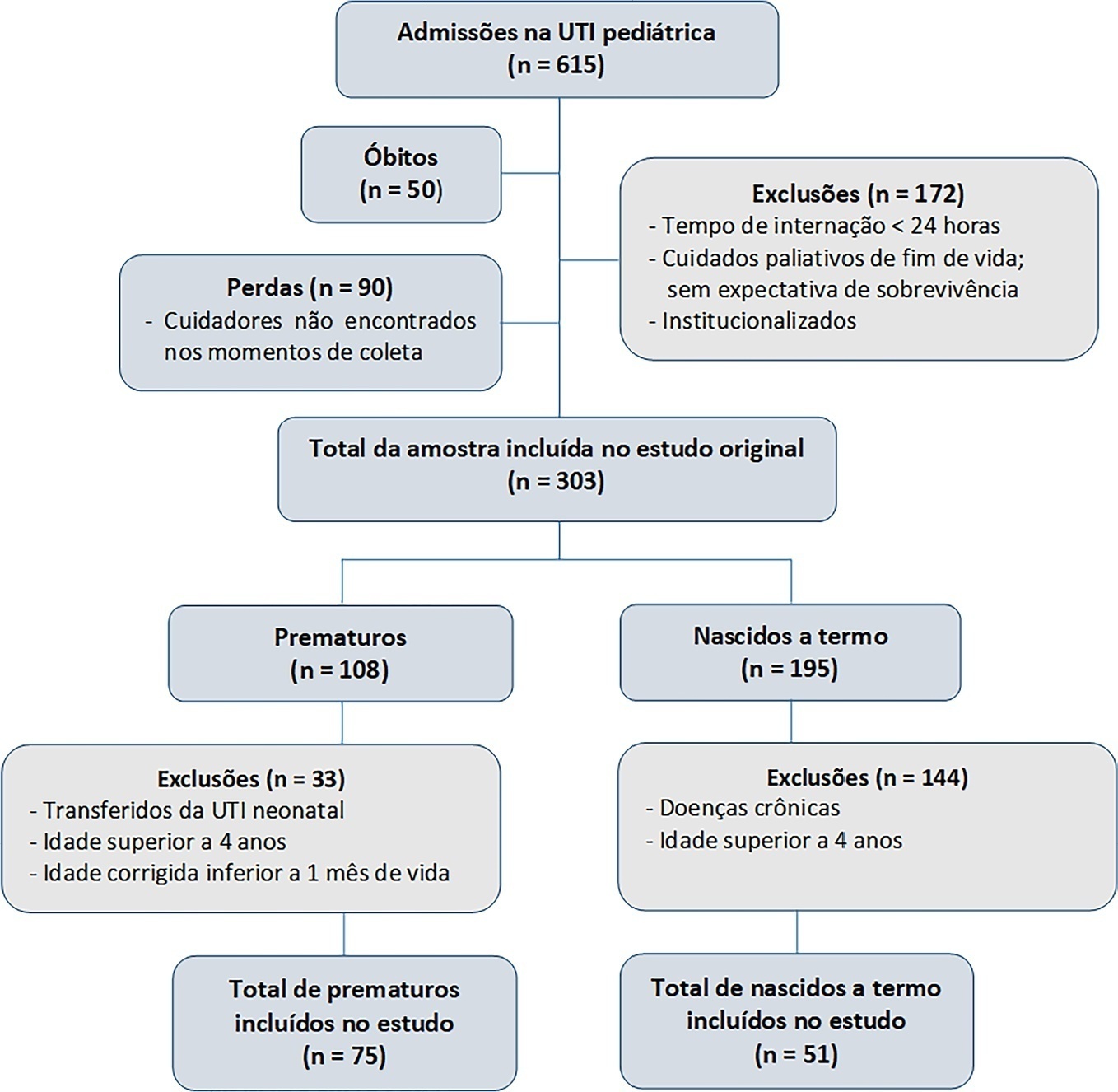
To evaluate the effects of critical illness on the functional status of children aged zero to 4 years with or without a history of prematurity after discharge from the pediatric intensive care unit.
This was a secondary cross-sectional study nested in an observational cohort of survivors from a pediatric intensive care unit. Functional assessment was performed using the Functional Status Scale within 48 hours after discharge from the pediatric intensive care unit.
A total of 126 patients participated in the study, 75 of whom were premature, and 51 of whom were born at term. Comparing the baseline and functional status at pediatric intensive care unit discharge, both groups showed significant differences (p < 0.001). Preterm patients exhibited greater functional decline at discharge from the pediatric intensive care unit (61%). Among patients born at term, there was a significant correlation between the Pediatric Index of Mortality, duration of sedation, duration of mechanical ventilation and length of hospital stay with the functional outcomes (p = 0.05).
Most patients showed a functional decline at discharge from the pediatric intensive care unit. Although preterm patients had a greater functional decline at discharge, sedation and mechanical ventilation duration influenced functional status among patients born at term.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):477-483
DOI 10.5935/0103-507X.20220280-en
To create and validate a model for predicting septic or hypovolemic shock from easily obtainable variables collected from patients at admission to an intensive care unit.
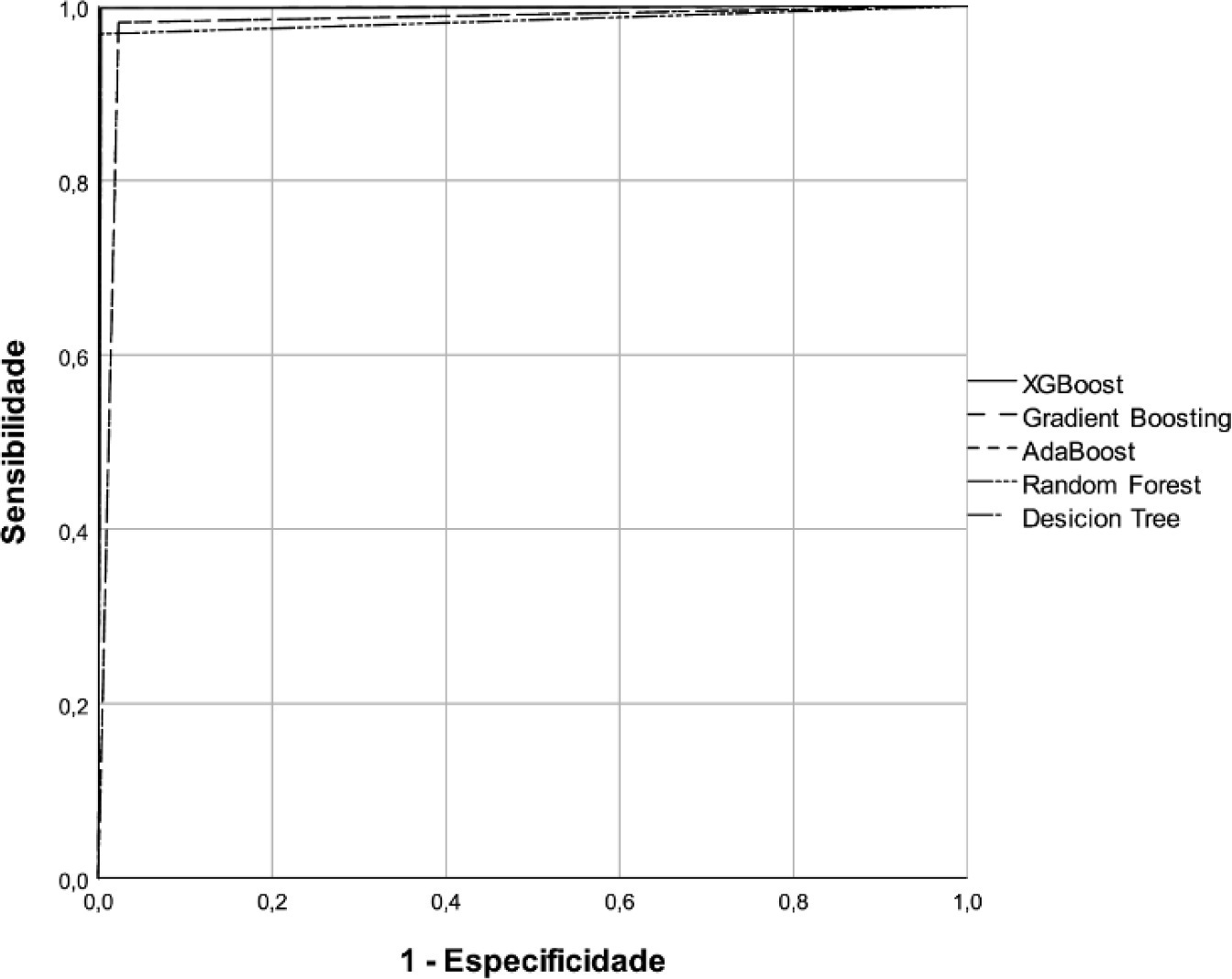
A predictive modeling study with concurrent cohort data was conducted in a hospital in the interior of northeastern Brazil. Patients aged 18 years or older who were not using vasoactive drugs on the day of admission and were hospitalized from November 2020 to July 2021 were included. The Decision Tree, Random Forest, AdaBoost, Gradient Boosting and XGBoost classification algorithms were tested for use in building the model. The validation method used was k-fold cross validation. The evaluation metrics used were recall, precision and area under the Receiver Operating Characteristic curve.
A total of 720 patients were used to create and validate the model. The models showed high predictive capacity with areas under the Receiver Operating Characteristic curve of 0.979; 0.999; 0.980; 0.998 and 1.00 for the Decision Tree, Random Forest, AdaBoost, Gradient Boosting and XGBoost algorithms, respectively.
The predictive model created and validated showed a high ability to predict septic and hypovolemic shock from the time of admission of patients to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):484-491
DOI 10.5935/0103-507X.20220264-en
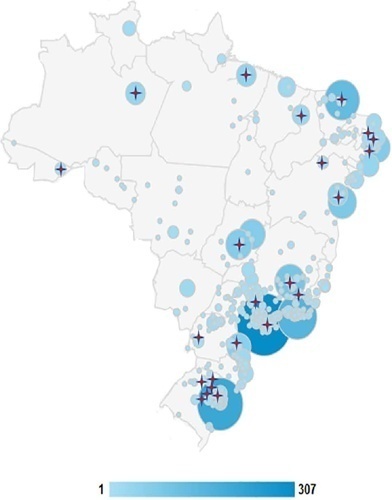
To obtain data on bed refusal in intensive care units in Brazil and to evaluate the use of triage systems by professionals.
A cross-sectional survey. Using the Delphi methodology, a questionnaire was created contemplating the objectives of the study. Physicians and nurses enrolled in the research network of the Associação de Medicina Intensiva Brasileira (AMIBnet) were invited to participate. A web platform (SurveyMonkey®) was used to distribute the questionnaire. The variables in this study were measured in categories and expressed as proportions. The chi-square test or Fisher’s exact test was used to verify associations. The significance level was set at 5%.
In total, 231 professionals answered the questionnaire, representing all regions of the country. The national intensive care units had an occupancy rate of more than 90% always or frequently for 90.8% of the participants. Among the participants, 84.4% had already refused admitting patients to the intensive care unit due to the capacity of the unit. Half of the Brazilian institutions (49.7%) did not have triage protocols for admission to intensive beds.
Bed refusal due to high occupancy rates is common in Brazilian intensive care units. Even so, half of the services in Brazil do not adopt protocols for triage of beds.