Abstract
Rev Bras Ter Intensiva. 2020;32(1):92-98
DOI 10.5935/0103-507X.20200014
To examine the impact of delayed transfer from the emergency room into the intensive care unit on the length of intensive care unit stay and death.
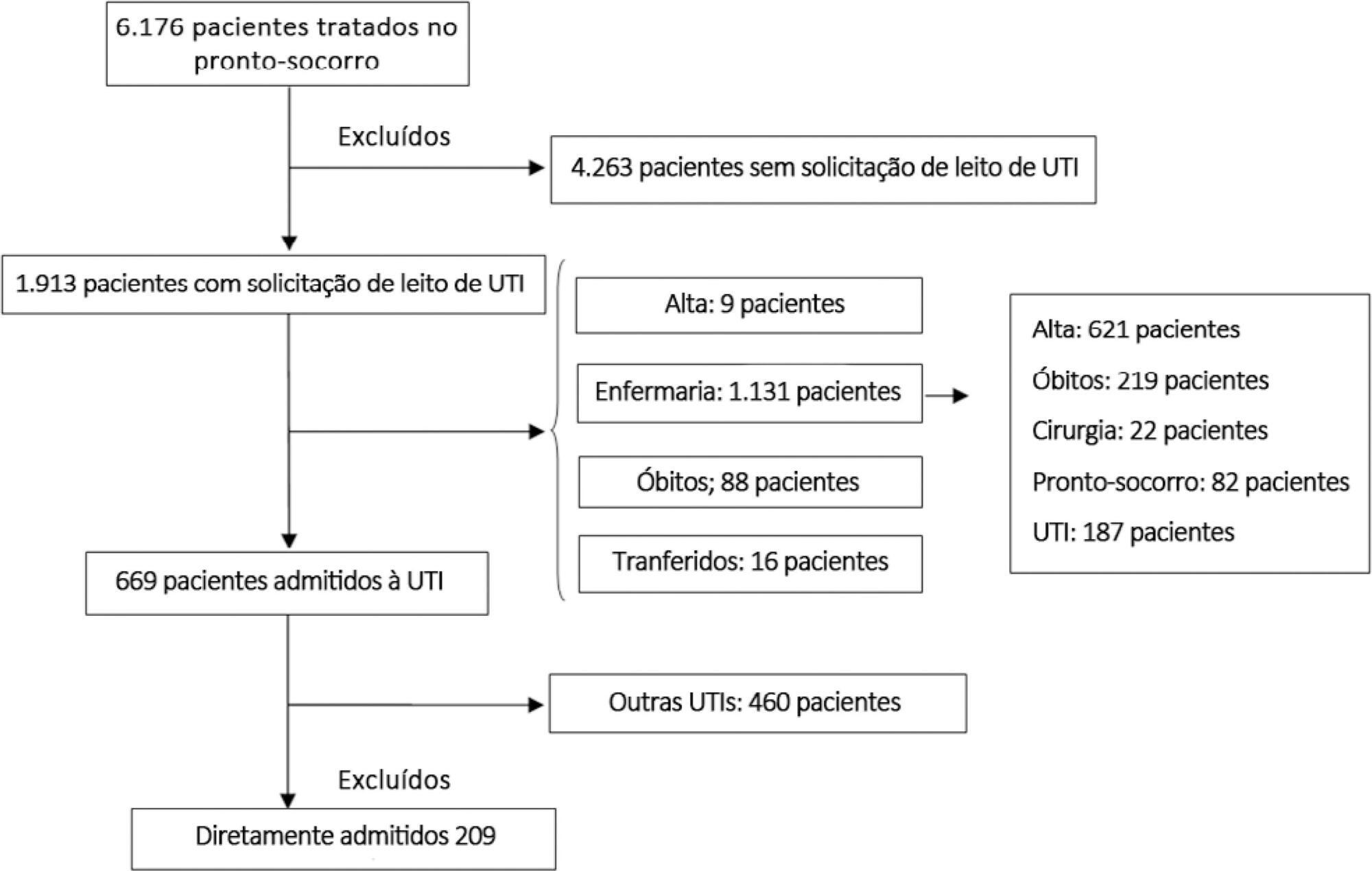
This prospective, cohort study performed in a tertiary academic hospital obtained data from 1913 patients admitted to the emergency room with a documented request for admission into the intensive care unit. The patients admitted directly into the medical-surgical intensive care unit (n = 209) were categorized into tertiles according to their waiting time for intensive care unit admission (Group 1: < 637 min, Group 2: 637 to 1602 min, and Group 3: > 1602 min). Patients who stayed in the intensive care unit for longer than 3.2 days (median time of intensive care unit length of stay of all patients) were considered as having a prolonged intensive care unit stay.
A total of 6,176 patients were treated in the emergency room during the study period, among whom 1,913 (31%) required a bed in the intensive care unit. The median length of stay in the emergency room was 17 hours [9 to 33 hours]. Hospitalization for infection/sepsis was an independent predictor of prolonged intensive care unit stay (OR 2.75 95%CI 1.38 - 5.48, p = 0.004), but waiting time for intensive care unit admission was not. The mortality rate was higher in Group 3 (38%) than in Group 1 (31%) but the difference was not statistically significant.
Delayed admission into the intensive care unit from the emergency room did not result in an increased intensive care unit stay or mortality.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):122-128
DOI 10.5935/0103-507X.20190037
To evaluate the impact of the presence of sepsis on in-hospital mortality after intensive care unit discharge.
Retrospective, observational, single-center study. All consecutive patients discharged alive from the intensive care unit of Hospital Vila Franca de Xira (Portugal) from January 1 to December 31, 2015 (N = 473) were included and followed until death or hospital discharge. In-hospital mortality after intensive care unit discharge was calculated for septic and non-septic patients.
A total of 61 patients (12.9%) died in the hospital after being discharged alive from the intensive care unit. This rate was higher among the patients with sepsis on admission, 21.4%, whereas the in-hospital, post-intensive care unit mortality rate for the remaining patients was nearly half that, 9.3% (p < 0.001). Other patient characteristics associated with mortality were advanced age (p = 0.02), male sex (p < 0.001), lower body mass index (p = 0.02), end-stage renal disease (p = 0.04) and high Simplified Acute Physiology Score II (SAPS II) at intensive care unit admission (p < 0.001), the presence of shock (p < 0.001) and medical admission (p < 0.001). We developed a logistic regression model and identified the independent predictors of in-hospital mortality after intensive care unit discharge.
Admission to the intensive care unit with a sepsis diagnosis is associated with an increased risk of dying in the hospital, not only in the intensive care unit but also after resolution of the acute process and discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):414-422
DOI 10.5935/0103-507X.20180059
To describe the improvements of an early warning system for the identification of septic patients on the time to diagnosis, antibiotic delivery, and mortality.
This was an observational cohort study that describes the successive improvements made over a period of 10 years using an early warning system to detect sepsis, including systematic active manual surveillance, electronic alerts via a telephonist, and alerts sent directly to the mobile devices of nurses. For all periods, after an alert was triggered, early treatment was instituted according to the institutional sepsis guidelines.
In total, 637 patients with sepsis were detected over the study period. The median triage-to-diagnosis time was reduced from 19:20 (9:10 - 38:15) hours to 12:40 (2:50 - 23:45) hours when the manual surveillance method was used (p = 0.14), to 2:10 (1:25 - 2:20) hours when the alert was sent automatically to the hospital telephone service (p = 0.014), and to 1:00 (0:30 - 1:10) hour when the alert was sent directly to the nurse's mobile phone (p = 0.016). The diagnosis-to-antibiotic time was reduced to 1:00 (0:55 - 1:30) hours when the alert was sent to the telephonist and to 0:45 (0:30 - 1:00) minutes when the alert was sent directly to the nurse's mobile phone (p = 0.02), with the maintenance of similar values over the following years. There was no difference in the time of treatment between survivors and non-survivors.
Electronic systems help reduce the triage-to-diagnosis time and diagnosis-to-antibiotic time in patients with sepsis.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):278-284
DOI 10.5935/0103-507X.20160045
To evaluate the implementation of a multidisciplinary rapid response team led by an intensive care physician at a university hospital.
This retrospective cohort study analyzed assessment forms that were completed during the assessments made by the rapid response team of a university hospital between March 2009 and February 2014.
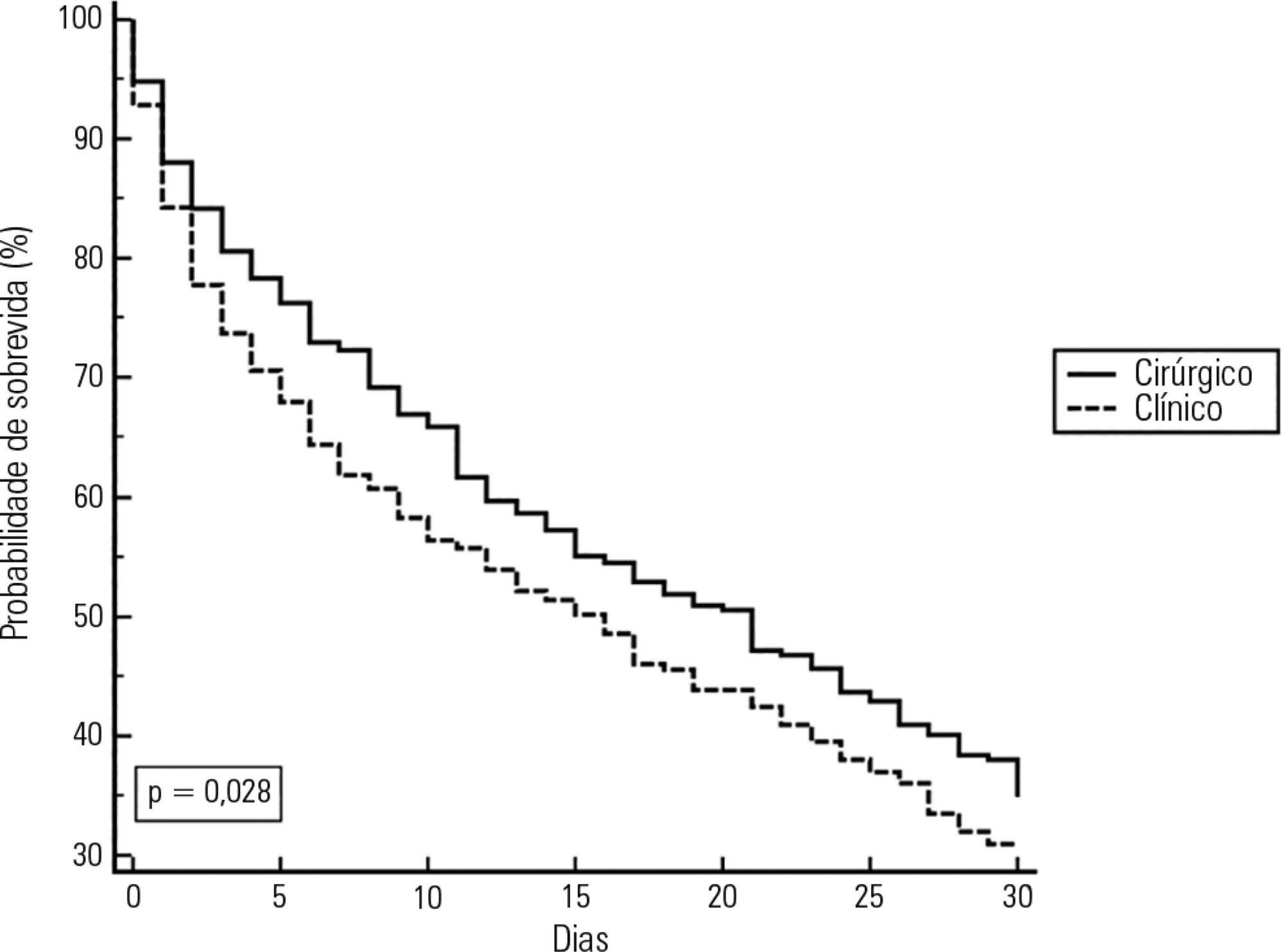
Data were collected from 1,628 assessments performed by the rapid response team for 1,024 patients and included 1,423 code yellow events and 205 code blue events. The number of assessments was higher in the first year of operation of the rapid response team. The multivariate analysis indicated that age (OR 1.02; 95%CI 1.02 - 1.03; p < 0.001), being male (OR 1.48; 95%CI 1.09 - 2.01; p = 0.01), having more than one assessment (OR 3.31; 95%CI, 2.32 - 4.71; p < 0.001), hospitalization for clinical care (OR 1.77; 95%CI 1.29 - 2.42; p < 0.001), the request of admission to the intensive care unit after the code event (OR 4.75; 95%CI 3.43 - 6.59; p < 0.001), and admission to the intensive care unit before the code event (OR 2.13; 95%CI 1.41 - 3.21; p = 0.001) were risk factors for hospital mortality in patients who were seen for code yellow events.
The hospital mortality rates were higher than those found in previous studies. The number of assessments was higher in the first year of operation of the rapid response team. Moreover, hospital mortality was higher among patients admitted for clinical care.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):420-426
DOI 10.5935/0103-507X.20160075
To determine the incidence of afferent limb failure of the in-hospital Medical Emergency Team, characterizing it and comparing the mortality between the population experiencing afferent limb failure and the population not experiencing afferent limb failure.
A total of 478 activations of the Medical Emergency Team of Hospital Pedro Hispano occurred from January 2013 to July 2015. A sample of 285 activations was obtained after excluding incomplete records and activations for patients with less than 6 hours of hospitalization. The sample was divided into two groups: the group experiencing afferent limb failure and the group not experiencing afferent limb failure of the Medical Emergency Team. Both populations were characterized and compared. Statistical significance was set at p ≤ 0.05.
Afferent limb failure was observed in 22.1% of activations. The causal analysis revealed significant differences in Medical Emergency Team activation criteria (p = 0.003) in the group experiencing afferent limb failure, with higher rates of Medical Emergency Team activation for cardiac arrest and cardiovascular dysfunction. Regarding patient outcomes, the group experiencing afferent limb failure had higher immediate mortality rates and higher mortality rates at hospital discharge, with no significant differences. No significant differences were found for the other parameters.
The incidence of cardiac arrest and the mortality rate were higher in patients experiencing failure of the afferent limb of the Medical Emergency Team. This study highlights the need for health units to invest in the training of all healthcare professionals regarding the Medical Emergency Team activation criteria and emergency medical response system operations.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):40-48
DOI 10.5935/0103-507X.20160012
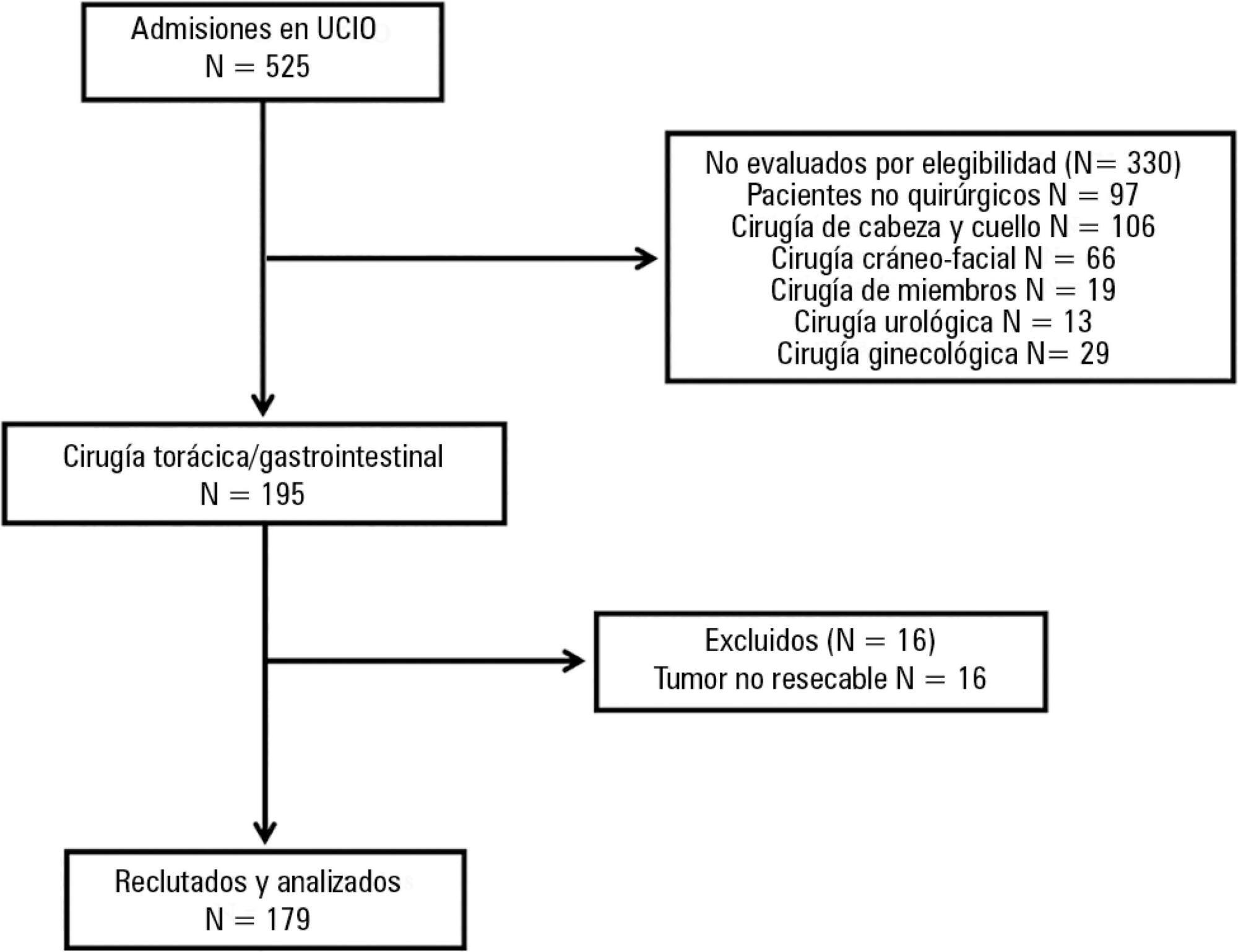
This study sought to determine the influence of postoperative complications on the clinical outcomes of patients who underwent thoracic and gastrointestinal cancer surgery.
A prospective cohort study was conducted regarding 179 consecutive patients who received thorax or digestive tract surgery due to cancer and were admitted to an oncological intensive care unit. The Postoperative Morbidity Survey was used to evaluate the incidence of postoperative complications. The influence of postoperative complications on both mortality and length of hospital stay were also assessed.
Postoperative complications were found for 54 patients (30.2%); the most common complications were respiratory problems (14.5%), pain (12.9%), cardiovascular problems (11.7%), infectious disease (11.2%), and surgical wounds (10.1%). A multivariate logistic regression found that respiratory complications (OR = 18.68; 95%CI = 5.59 - 62.39; p < 0.0001), cardiovascular problems (OR = 5.06, 95%CI = 1.49 - 17.13; p = 0.009), gastrointestinal problems (OR = 26.09; 95%CI = 6.80 - 100.16; p < 0.0001), infectious diseases (OR = 20.55; 95%CI = 5.99 - 70.56; p < 0.0001) and renal complications (OR = 18.27; 95%CI = 3.88 - 83.35; p < 0.0001) were independently associated with hospital mortality. The occurrence of at least one complication increased the likelihood of remaining hospitalized (log-rank test, p = 0.002).
Postoperative complications are frequent disorders that are associated with poor clinical outcomes; thus, structural and procedural changes should be implemented to reduce postoperative morbidity and mortality.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):246-251
DOI 10.1590/S0103-507X2012000300007
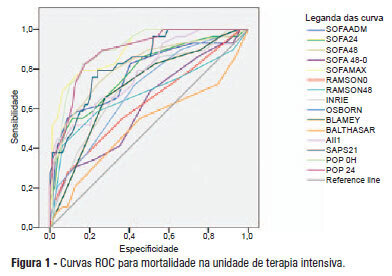
OBJECTIVE: This study compared the general and specific severity indices to assess the prognosis of severe acute pancreatitis at a polyvalent intensive care unit. METHODS: This retrospective study included 108 patients who were diagnosed with severe acute pancreatitis from July 1, 1999 to March 31, 2012. Their demographic and clinical data were collected, and the following severity indices were calculated: Ranson, Osborne, Blamey and Imrie, Balthazar, POP, APACHE II, SAPS II, and SOFA. The discriminative power of these indices with regard to mortality at the intensive care unit and hospital was assessed using the area under the ROC curve. RESULTS: The demographic data of the surviving and deceased patients did not significantly differ at baseline. The mortality rates were 27% and 39% at the intensive care unit and hospital, respectively. The severity indices that exhibited the greatest discriminative power with regard to mortality at the intensive care unit and hospital were the POP 0, POP 24, SOFA (at admission, 24 hours, 48 hours, and discharge), SAPS II, and APACHE II. CONCLUSION: The POP performed better than the other indices (aROC>0.8) at admission and 24 hours later (as originally described). The general physiological dysfunction indices also exhibited reasonable discriminative power (aROC=0.75-0.8), which was unlike the remaining pancreatitis specific indices, whose discriminative power was lower.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):359-368
DOI 10.1590/S0103-507X2009000400005
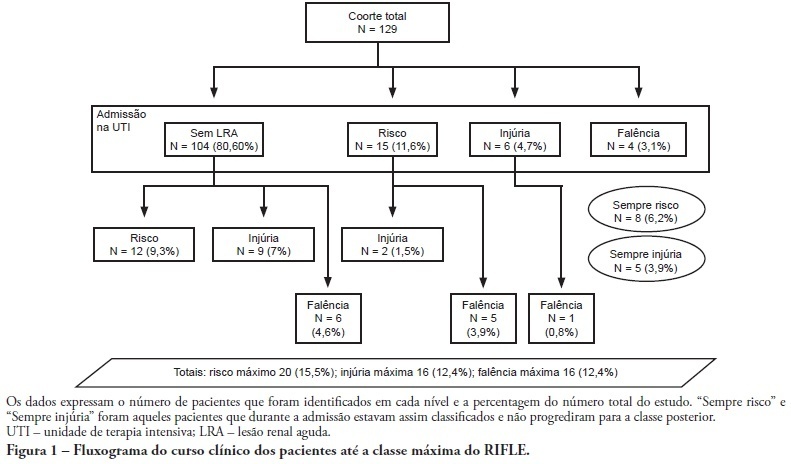
OBJECTIVE: To correlate the RIFLE classification with mortality and length of stay both in the intensive care unit and hospital. METHODS: A prospective, observational, longitudinal cohort study, approved by the Institution's Ethics Committee. Data were collected for all patients staying longer than 24 hours in the intensive care unit of Hospital Universitário Polydoro Ernani de São Thiago - Universidade Federal de Santa Catarina from September 2007 to March 2008, followed-up either until discharge or death. Patients were divided in two groups: with or without acute kidney injury. The acute kidney injury group was additionally divided according to the RIFLE and sub-divided according to the maximal score in Risk, Injury of Failure. Loss and End-stage classes were not included in the study. APACHE II and SOFA were also evaluated. The t Student and Chi-Square tests were used. A P<0.05 was considered statistically significant. RESULTS: The sample included 129 patients, 52 (40.3%) with acute kidney injury according to RIFLE. Patients were more severely ill in this group, with higher APACHE and SOFA scores (P<0.05). Compared to the without kidney injury group, the kidney injury severity caused increased intensive care unity (Risk 25%; Injury 37.5%; Failure 62.5%) and in-hospital (Risk 50%; Injury 37.5%; Failure 62.5%) mortality, and longer intensive care unit stay (P<0.05). CONCLUSION: The RIFLE system, according to the severity class, was a marker for risk of increased intensive care unit and in-hospital mortality, and longer intensive care unit stay. No relationship with in-hospital length of stay was found.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)