Abstract
Rev Bras Ter Intensiva. 2019;31(3):354-360
DOI 10.5935/0103-507X.20190058
To evaluate the agreement between intensive care physicians with similar training in the use of bedside lung ultrasonography in identifying pulmonary B lines, visualized in real time, to verify the reproducibility of the method.
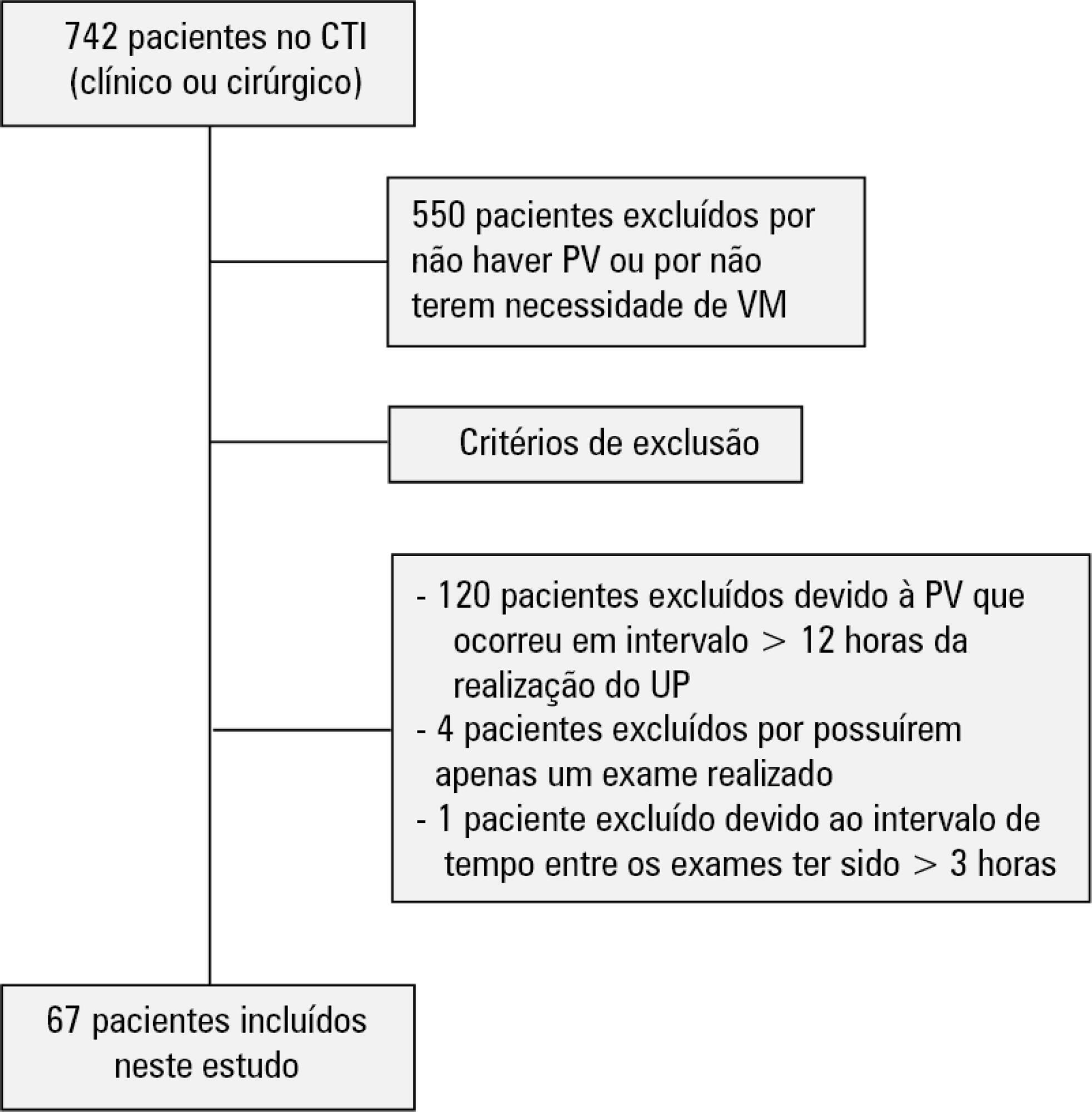
A total of 67 patients with some ventilatory deterioration identified within 12 hours after a pulmonary ultrasonography in the period from November 2016 to March 2017 were analyzed, and all were admitted to an intensive care unit of a private hospital in Belo Horizonte, Minas Gerais. The lung ultrasonographies were performed by three different professionals, termed A, B and C, and the time interval between each lung ultrasonography was less than 3 hours. The only visualized chest zones were the anterior and lateral, defined as right and left anterior (1) zones (Z1R and Z1L, respectively), which were delimited by the clavicle, the sternum and the horizontal line perpendicular to the xiphoid process and anterior axillary line. The right and left lateral (2) zones (Z2R and Z2L, respectively) covered the lateral area between the anterior and posterior axillary lines, with the lower limit being the same horizontal line corresponding to the height of the xiphoid process. A lung zone was considered positive for B lines upon visualization of three or more of these lines, suggesting the presence of alveolar-interstitial syndrome. Using the Kappa value, we evaluated the agreement among the four zones according to the execution of each pair of professionals (AB, AC and BC).
Approximately 80% of the areas that were visualized showed a moderate to substantial agreement, with the Kappa values ranging from 0.41 - 079 (p < 0.05; 95% CI). The highest levels of agreement occurred in the upper zones Z1R and Z1L between subgroups AC and BC, with a Kappa of approximately 0.65 (p < 0.001). In turn, Z2L showed one of the lowest agreements, with a Kappa of 0.36.
The possible limitation of an examiner-dependent effect on lung ultrasounds was not found in this study, suggesting the good reproducibility of this diagnostic modality at the bedside.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):393-402
DOI 10.5935/0103-507X.20190062
To review the scientific evidence regarding the initiation of enteral nutrition in the pediatric burn population.
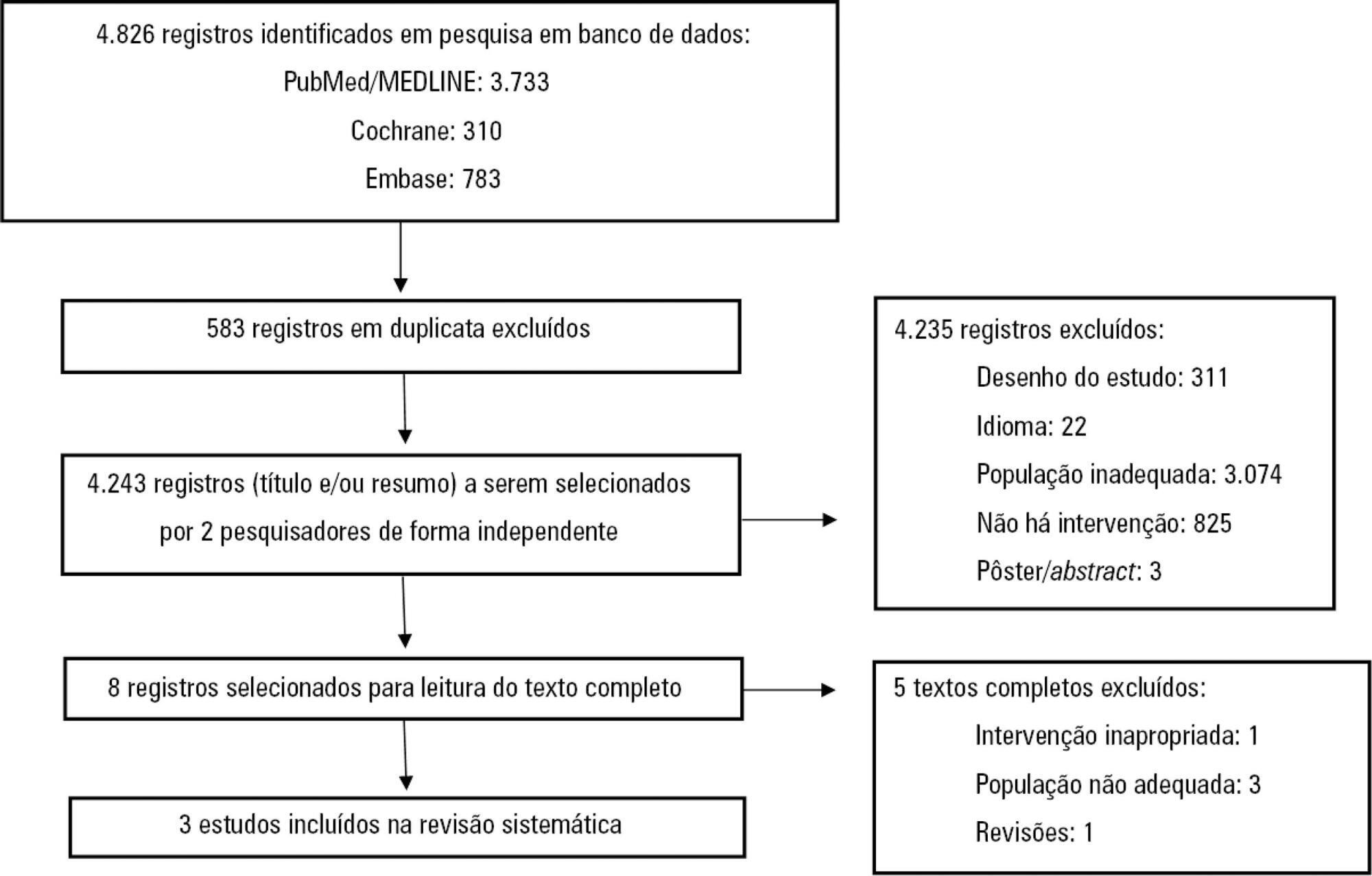
This study was a systematic review and meta-analysis of randomized clinical trials comparing early enteral nutrition and late enteral nutrition in individuals aged 1 month to 18 years with burns. The MEDLINE/PubMed, Embase and Cochrane Library databases were searched using the terms "burns", "fires", "child nutrition disorders", "nutritional support" and related terms.
Three articles that included a total of 781 patients were identified. There was no significant difference in the mortality rate between the early and late groups (OR = 0.72, 95%CI = 0.46 - 1.15, p = 0.17). Patients who received early enteral nutrition had a 3.69-day reduction in the length of hospital stay (mean difference = -3.69, 95%CI = -4.11 - -3.27, p < 0.00001). There was a higher incidence of diarrhea and vomiting and decreased intestinal permeability in the early group. This group also presented higher a serum insulin concentration and insulin/glucagon ratio as well as lower caloric deficit and weight loss when compared to the control group.
Analysis of the different intragroup variables suggests the importance of starting nutritional support early. Considering the number of pediatric burn patients, there is a need for robust studies with greater scientific impact.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):410-424
DOI 10.5935/0103-507X.20190063
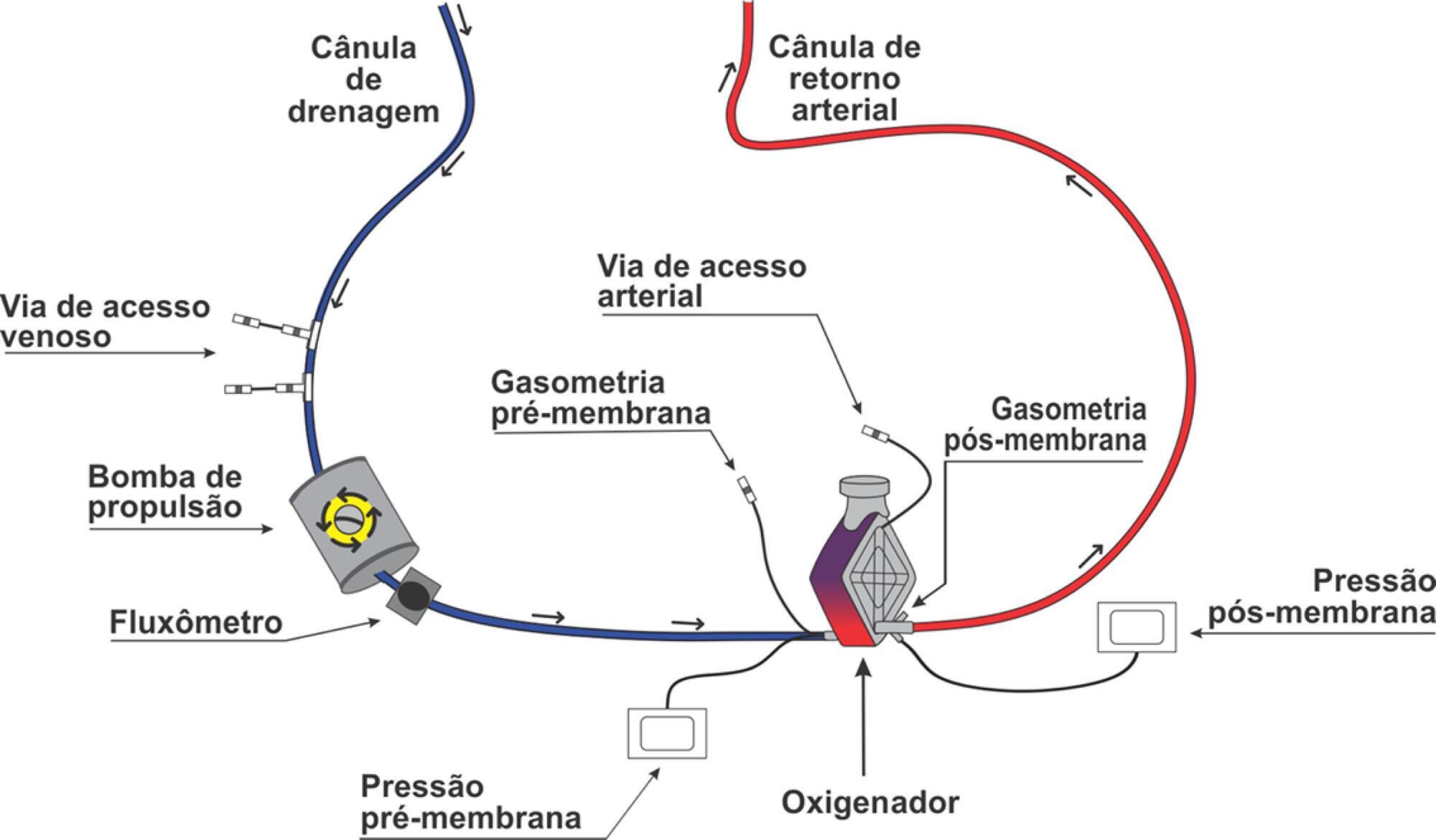
Extracorporeal membrane oxygenation is a modality of extracorporeal life support that allows for temporary support in pulmonary and/or cardiac failure refractory to conventional therapy. Since the first descriptions of extracorporeal membrane oxygenation, significant improvements have occurred in the device and the management of patients and, consequently, in the outcomes of critically ill patients during extracorporeal membrane oxygenation. Many important studies about the use of extracorporeal membrane oxygenation in patients with acute respiratory distress syndrome refractory to conventional clinical support, under in-hospital cardiac arrest and with cardiogenic refractory shock have been published in recent years. The objective of this literature review is to present the theoretical and practical aspects of extracorporeal membrane oxygenation support for respiratory and/or cardiac functions in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):258-261
DOI 10.5935/0103-507X.20190040
Rituximab safety and efficacy in patients with renal impairment have not been established, nor have the effects of hemodialysis on serum rituximab level. There are only a few published case reports assessing serum rituximab level pre- and postdialysis. No data have been published regarding the usage of rituximab in patients with continuous renal replacement therapy. The authors present a case of a 59-year-old female patient who presented with paraneoplastic tetraparesis. She was admitted to the intensive care unit due to alveolar hemorrhage with respiratory failure and acute kidney injury requiring continuous renal replacement therapy. After a diagnostic workup, the diagnosis of lymphoplasmacytic lymphoma was established. Therapy with rituximab and cyclophosphamide was started. Rituximab levels were determined in serum and dialysate. No rituximab was found in the dialysate. The patient died after 2 months in the intensive care unit from nosocomial pneumonia due to multidrug-resistant Pseudomonas aeruginosa.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):248-257
DOI 10.5935/0103-507X.20190038
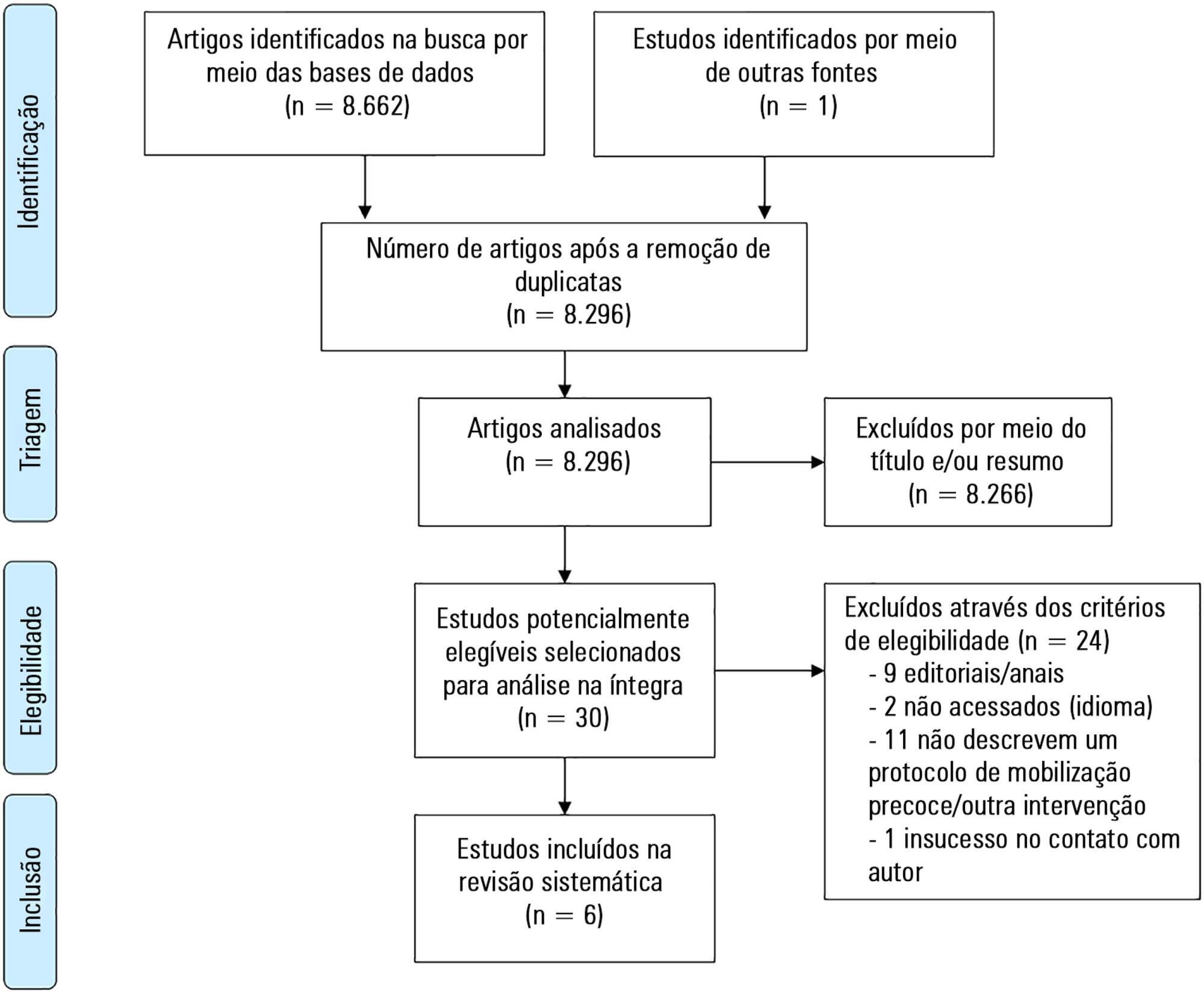
To describe the existing early mobilization protocols in pediatric intensive care units.
A systematic literature review was performed using the databases MEDLINE®, Embase, SciELO, LILACS and PeDRO, without restrictions of date and language. Observational and randomized and nonrandomized clinical trials that described an early mobilization program in patients aged between 29 days and 18 years admitted to the pediatric intensive care unit were included. The methodological quality of the studies was evaluated using the Newcastle-Ottawa Scale, Methodological Index for Non-Randomized Studies and the Cochrane Collaboration.
A total of 8,663 studies were identified, of which 6 were included in this review. Three studies described the implementation of an early mobilization program, including activities such as progressive passive mobilization, positioning, and discussion of mobilization goals with the team, in addition to contraindications and interruption criteria. Cycle ergometer and virtual reality games were also used as resources for mobilization. Four studies considered the importance of the participation of the multidisciplinary team in the implementation of early mobilization protocols.
In general, early mobilization protocols are based on individualized interventions, depending on the child's development. In addition, the use of a cycle ergometer may be feasible and safe in this population. The implementation of institutional and multidisciplinary protocols may contribute to the use of early mobilization in pediatric intensive care units; however, studies demonstrating the efficacy of such intervention are needed.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):193-201
DOI 10.5935/0103-507X.20190033
To characterize resource availability from a nationally representative random sample of intensive care units in Brazil.
A structured online survey of participating units in the Sepsis PREvalence Assessment Database (SPREAD) study, a nationwide 1-day point prevalence survey to assess the burden of sepsis in Brazil, was sent to the medical director of each unit.
A representative sample of 277 of the 317 invited units responded to the resources survey. Most of the hospitals had fewer than 500 beds (94.6%) with a median of 14 beds in the intensive care unit. Providing care for public-insured patients was the main source of income in two-thirds of the surveyed units. Own microbiology laboratory was not available for 26.8% of the surveyed intensive care units, and 10.5% did not always have access to blood cultures. Broad spectrum antibiotics were not always available in 10.5% of surveyed units, and 21.3% could not always measure lactate within three hours. Those institutions with a high resource availability (158 units, 57%) were usually larger and preferentially served patients from the private health system compared to institutions without high resource availability. Otherwise, those without high resource availability did not always have broad-spectrum antibiotics (24.4%), vasopressors (4.2%) or crystalloids (7.6%).
Our study indicates that a relevant number of units cannot perform basic monitoring and therapeutic interventions in septic patients. Our results highlight major opportunities for improvement to adhere to simple but effective interventions in Brazil.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):202-209
DOI 10.5935/0103-507X.20190032
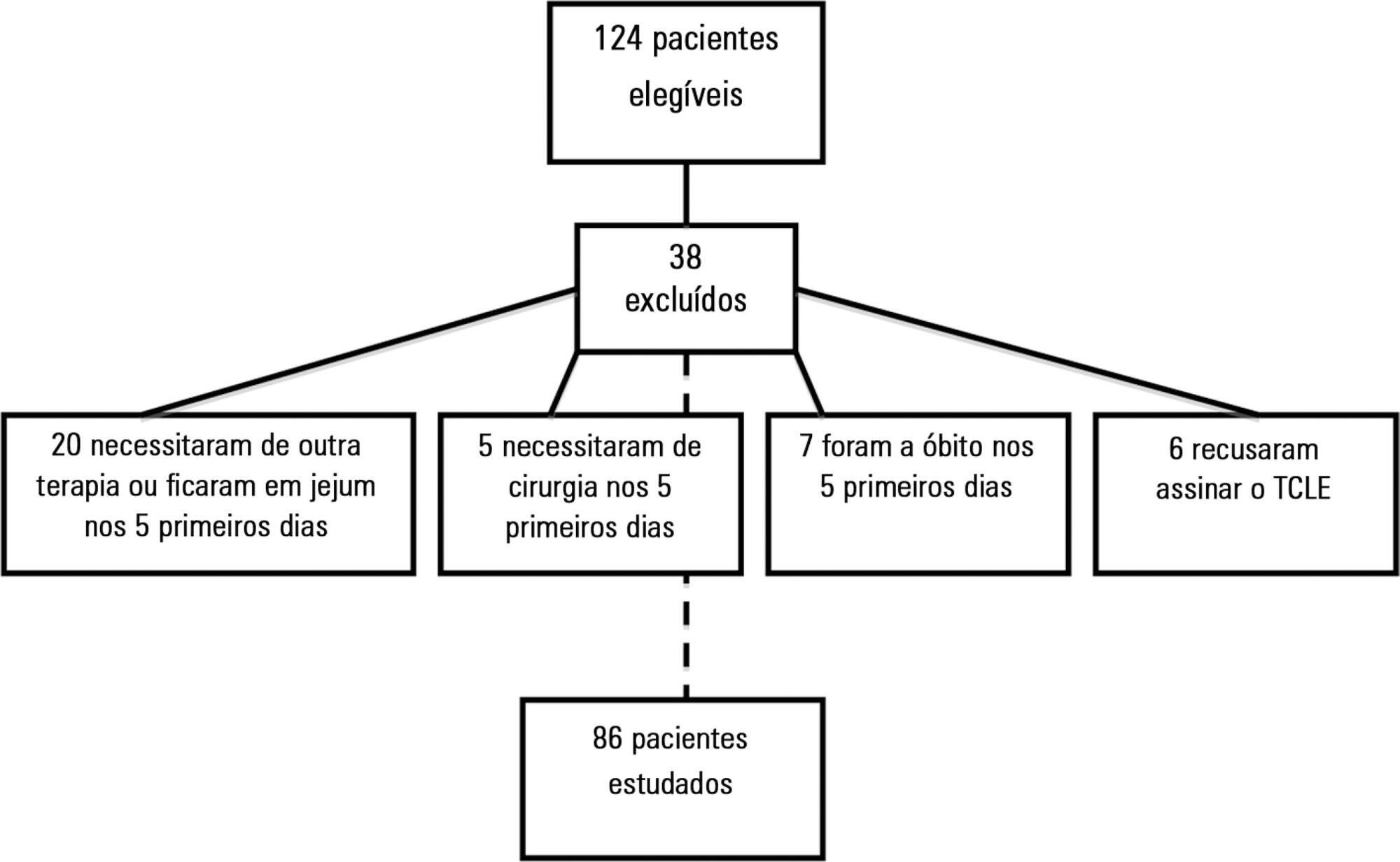
To evaluate the effects of intravenous infusion of fluids and sodium on the first day of admission on infusion of enteral nutrition in the first 5 days in intensive care patients.
A prospective cohort study was conducted with critical nonsurgical patients admitted for at least 5 days who were on mechanical ventilation and receiving enteral nutrition. The amount of intravenous fluids and sodium infused on the first day and the volume of enteral nutrition infused in the first 5 days were investigated. The volume of intravenous fluids > 35mL/kg or ≤ 35mL/kg of body weight and sodium (above or below the 25th percentile) infused on the first day was compared with infused enteral nutrition.
A total of 86 patients were studied, with a mean (± standard deviation) of 65 ± 17 years, of which 54.7% were female. On the first day, 3,393.7 ± 1,417.0mL of fluid (48.2 ± 23.0mL/kg) and 12.2 ± 5.1g of sodium were administered. Fifty-eight (67.4%) patients received more than 35mL/kg of fluids. In 5 days, 67 ± 19.8% (2,993.8 ± 1,324.4mL) of the prescribed enteral nutrition was received. Patients who received > 35mL/kg of intravenous fluids also received less enteral nutrition in 5 days (2,781.4 ± 1,337.9 versus 3,433.6 ± 1,202.2mL; p = 0.03) versus those who received ≤ 35mL/kg. Patients with intravenous sodium infusion above the 25th percentile (≥ 8.73g) on the first day received less enteral nutrition volume in 5 days (2,827.2 ± 1,398.0 versus 3,509.3 ± 911.9mL; p = 0.02).
The results of this study support the assumption that the administration of intravenous fluids > 35mL/kg and sodium ≥ 8.73g on the first day of hospitalization may contribute to the lower infusion of enteral nutrition in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):164-170
DOI 10.5935/0103-507X.20190028
To evaluate the satisfaction of patients admitted to the intensive care unit using a diary and analyze possible points for improving this instrument.
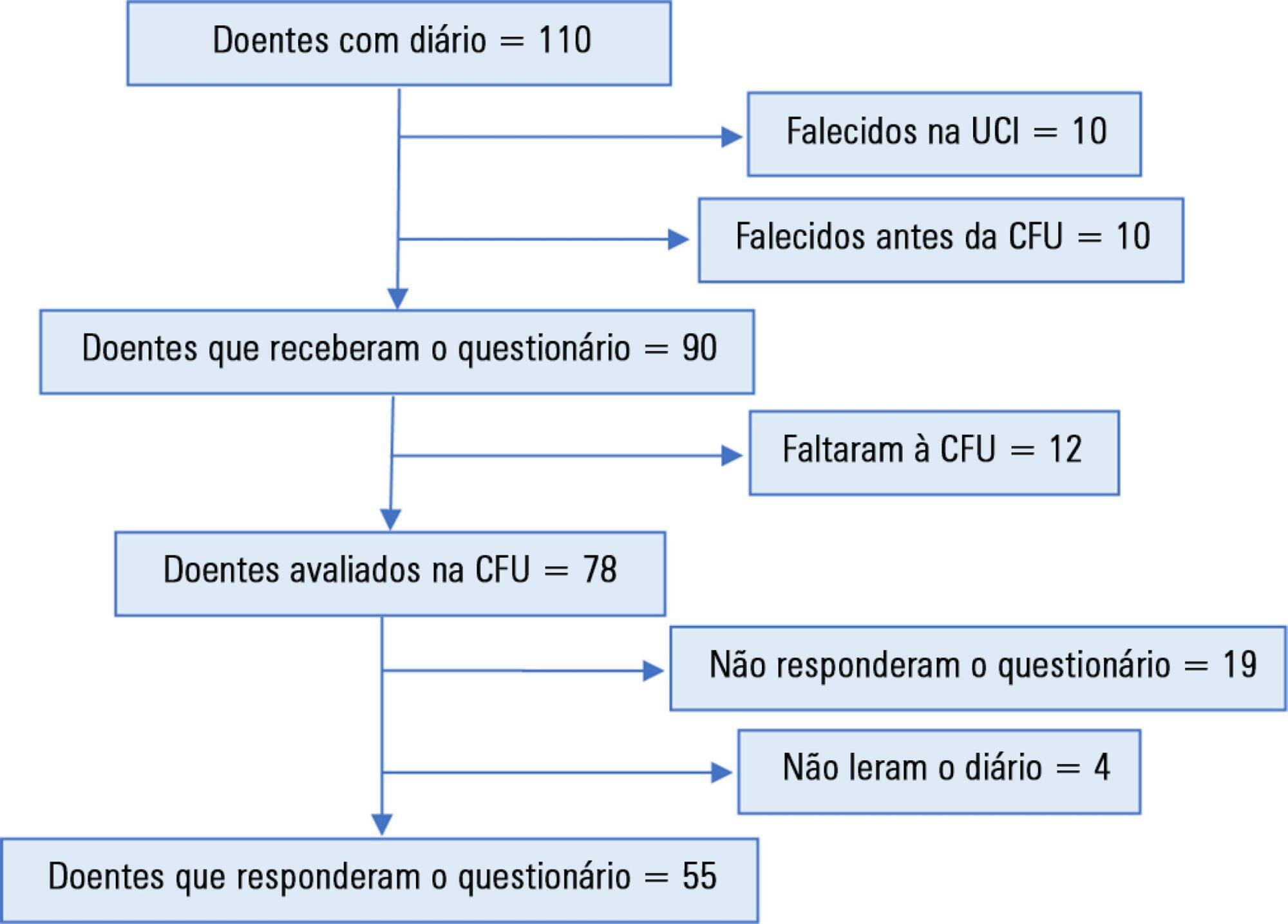
This was an observational, retrospective study, conducted between March 2014 and July 2017, in a multidisciplinary intensive care unit of a district hospital. The diary was implemented in patients sedated for 3 or more days. Three months after discharge, their satisfaction was assessed using a questionnaire. A patient who agreed with the 5 statements assessing the diary's help in clarifying the intensive care unit stay, in filling memory gaps, in recovery, in reassurance, and in the recommendation of this intervention was defined as satisfied.
A total of 110 patients were included, of whom 55 answered the questionnaire. Of these, 36 (65.5%) were classified as satisfied. Each item had a positive response in more than 74% of cases. A total of 60% of the participants suggested increasing the number of photographs. No significant differences were found in the subgroup analysis (age, sex, duration of sedation and ventilation, length of diary keeping, severity on admission, or delirium, depression, or anxiety in the intensive care unit).
Most patients were satisfied with the diary but suggested an increase in the number of photographs.