Abstract
Rev Bras Ter Intensiva. 2019;31(1):79-85
DOI 10.5935/0103-507X.20190012
We aimed to determine the incidence, risk factors, and outcomes of unplanned extubation among adult patients.
We conducted a prospective cohort study of adult intubated patients admitted to the charity wards of a government tertiary teaching hospital in the Philippines. Patients managed in both intensive care and nonintensive care settings were included. Patients were followed-up until discharge or until seven days postextubation.
The outcomes of the 191 included patients were planned extubation (35%), unplanned extubation (19%), death (39%), and discharge against advice (7%). Competing risk regression showed that male sex (Crude OR: 2.25, 95%CI: 1.10 - 4.63) and age (Crude OR 0.976, 95%CI: 0.957 - 0.996) were significant baseline factors. The night shift (Crude OR: 24.6, 95%CI: 2.87 - 211) was also consistently associated with more unplanned extubations. Among postextubation outcomes, reintubation (unplanned extubation: 61.1% versus planned extubation: 25.4%), acute respiratory failure (unplanned extubation: 38.9% versus planned extubation: 17.5%), and cardiovascular events (unplanned extubation: 8.33% versus planned extubation: 1.49%) occurred significantly more often among the unplanned extubation patients. Admission in an intensive care unit was not associated with a lower risk of unplanned extubation (Crude OR 1.15, 95%CI: 0.594 - 2.21).
Many intubated patients had unplanned extubation. Patients admitted in nonintensive care unit settings did not have significantly higher odds of unplanned extubation.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):34-38
DOI 10.5935/0103-507X.20190004
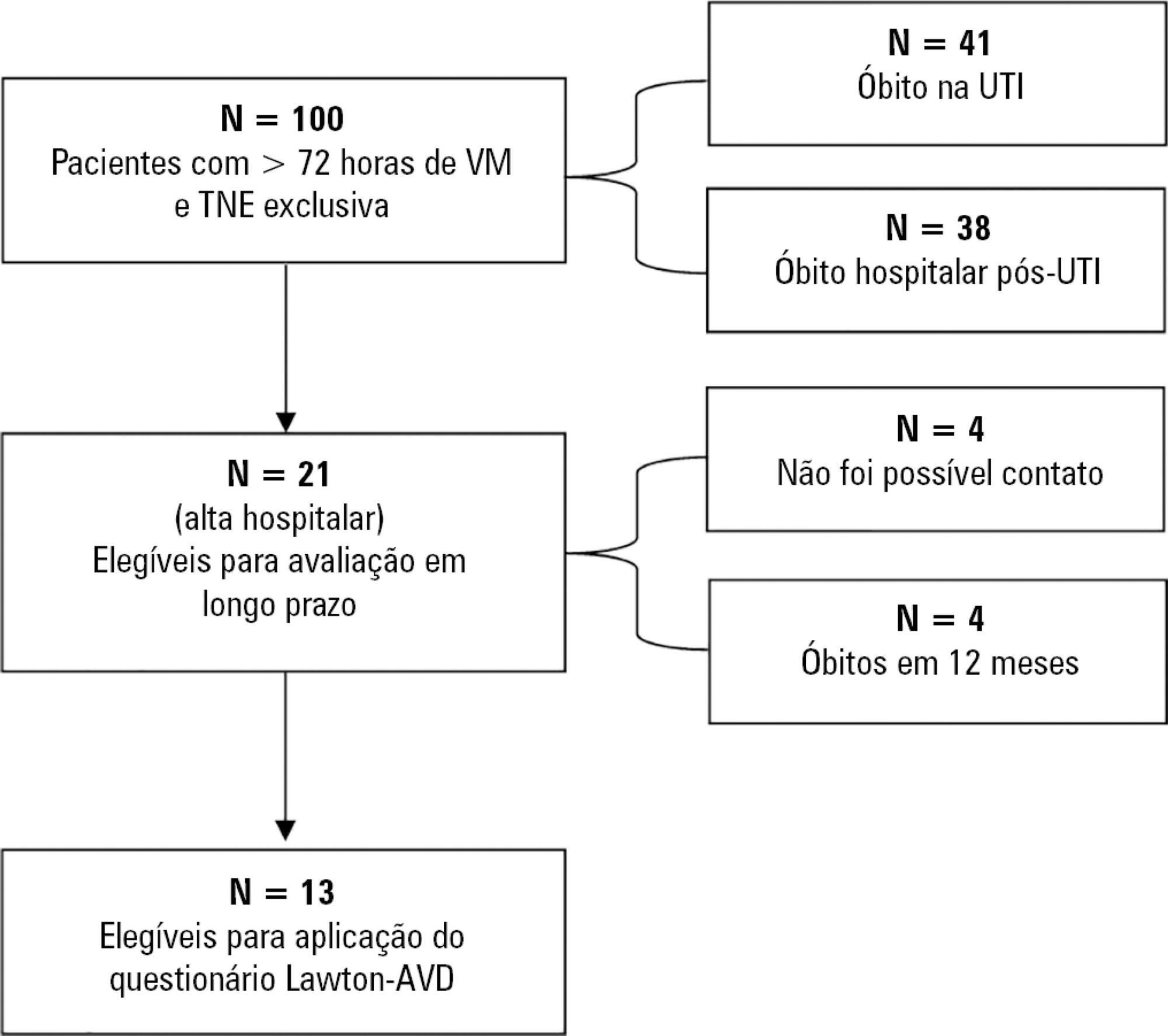
To correlate short-term (duration of mechanical ventilation and length of intensive care unit stay) and long-term (functional capacity) clinical outcomes of patients who reached nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization in the intensive care unit.
This was a prospective observational pilot study conducted in an 18-bed intensive care unit. A total of 100 mechanically ventilated patients receiving exclusive enteral nutritional support and receiving intensive care for more than 72 hours were included. Patients who never received enteral nutrition, those with spinal cord trauma, pregnant women, organ donors and cases of family refusal were excluded. The variables studied were nutritional adequacy ≥ 70% of predicted in the first 72 hours of hospitalization, length of intensive care unit stay, duration of mechanical ventilation and the ability to perform activities of daily living after 12 months, assessed via telephone contact using the Lawton Activities of Daily Living Scale.
The mean duration of mechanical ventilation was 18 ± 9 days, and the mean intensive care unit length of stay was 19 ± 8 days. Only 45% of the patients received more than 70% of the target nutrition in 72 hours. There was no association between nutritional adequacy and short-term (duration of mechanical ventilation, length of stay in the intensive care unit and mortality) or long-term (functional capacity and mortality) clinical outcomes.
Critically ill patients receiving caloric intake ≥ 70% in the first 72 hours of hospitalization did not present better outcomes in the short term or after 1 year.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):106-110
DOI 10.5935/0103-507X.20190015
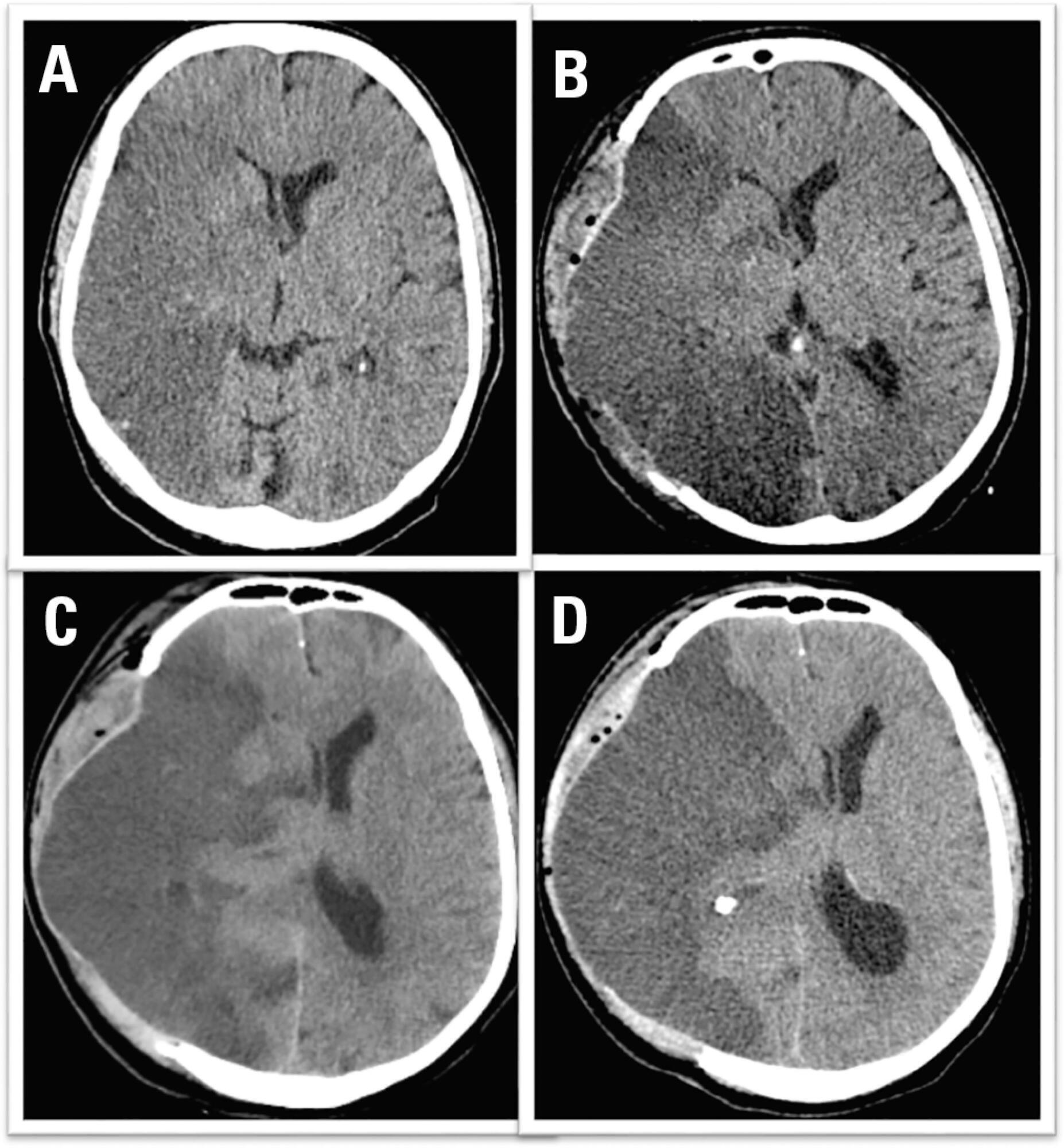
We report the case of a patient in whom brain death was suspected and associated with atelectasis and moderate to severe hypoxemia even though the patient was subjected to protective ventilation, a closed tracheal suction system, positive end-expiratory pressure, and recruitment maneuvers. Faced with the failure to obtain an adequate partial pressure of oxygen for the apnea test, we elected to place the patient in a prone position, use higher positive end-expiratory pressure, perform a new recruitment maneuver, and ventilate with a higher tidal volume (8mL/kg) without exceeding the plateau pressure of 30cmH2O. The apnea test was performed with the patient in a prone position, with continuous positive airway pressure coupled with a T-piece. The delay in diagnosis was 10 hours, and organ donation was not possible due to circulatory arrest. This report demonstrates the difficulties in obtaining higher levels of the partial pressure of oxygen for the apnea test. The delays in the diagnosis of brain death and in the organ donation process are discussed, as well as potential strategies to optimize the partial pressure of oxygen to perform the apnea test according to the current recommendations.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):57-63
DOI 10.5935/0103-507X.20180011
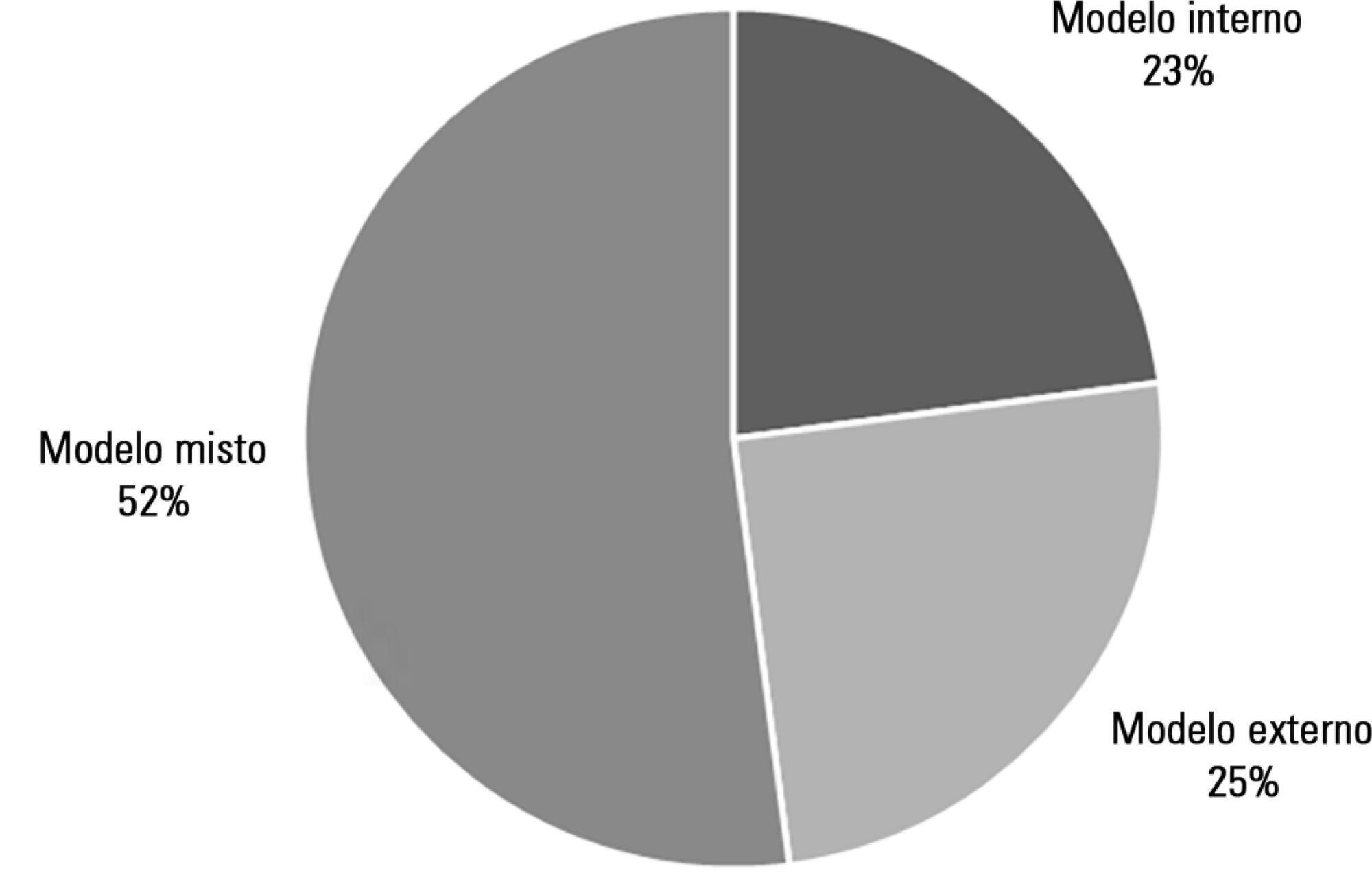
To describe the different rehabilitation care models in practice in Portuguese adult intensive care units.
A simple observational (cross-sectional) study was conducted through an online survey sent to the head nurses or individuals responsible for the 58 adult intensive care units that are part of the database of the Sociedade Portuguesa de Cuidados Intensivos.
We identified three models of organization of rehabilitation care: care provided by the staff of the intensive care unit (22.9%), care provided by specialized external teams (25.0%), and a mixture of the previous models, combining the two situations (52.1%). In the first model, the care was provided mainly by nurses with specialization in rehabilitation and, in the second model, the care was provided by physiotherapists. No significant differences were found between the models regarding the availability of care, in hours/day or days/week (p = 0.268 and 0.994, respectively), or results such as length of hospital stay in intensive care, ventilation time, or mortality rate in the unit (p = 0.418, 0.923, and 0.240, respectively).
The organization of rehabilitation care in Portuguese intensive care units is unique and heterogeneous. Despite different care organization models, the availability of hours of care is similar, as are the overall results observed in patients.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):153-159
DOI 10.5935/0103-507X.20180030
To investigate prognostic factors among critically ill patients with community-acquired bacterial meningitis and acute kidney injury.
A retrospective study including patients admitted to a tertiary infectious disease hospital in Fortaleza, Brazil diagnosed with community-acquired bacterial meningitis complicated with acute kidney injury. Factors associated with death, mechanical ventilation and use of vasopressors were investigated.
Forty-one patients were included, with a mean age of 41.6 ± 15.5 years; 56% were males. Mean time between intensive care unit admission and acute kidney injury diagnosis was 5.8 ± 10.6 days. Overall mortality was 53.7%. According to KDIGO criteria, 10 patients were classified as stage 1 (24.4%), 18 as stage 2 (43.9%) and 13 as stage 3 (31.7%). KDIGO 3 significantly increased mortality (OR = 6.67; 95%CI = 1.23 - 36.23; p = 0.028). Thrombocytopenia was not associated with higher mortality, but it was a risk factor for KDIGO 3 (OR = 5.67; 95%CI = 1.25 - 25.61; p = 0.024) and for mechanical ventilation (OR = 6.25; 95%CI = 1.33 - 29.37; p = 0.02). Patients who needed mechanical ventilation by 48 hours from acute kidney injury diagnosis had higher urea (44.6 versus 74mg/dL, p = 0.039) and sodium (138.6 versus 144.1mEq/L; p = 0.036).
Mortality among critically ill patients with community-acquired bacterial meningitis and acute kidney injury is high. Acute kidney injury severity was associated with even higher mortality. Thrombocytopenia was associated with severer acute kidney injury. Higher urea was an earlier predictor of severer acute kidney injury than was creatinine.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):496-507
DOI 10.5935/0103-507X.20180071
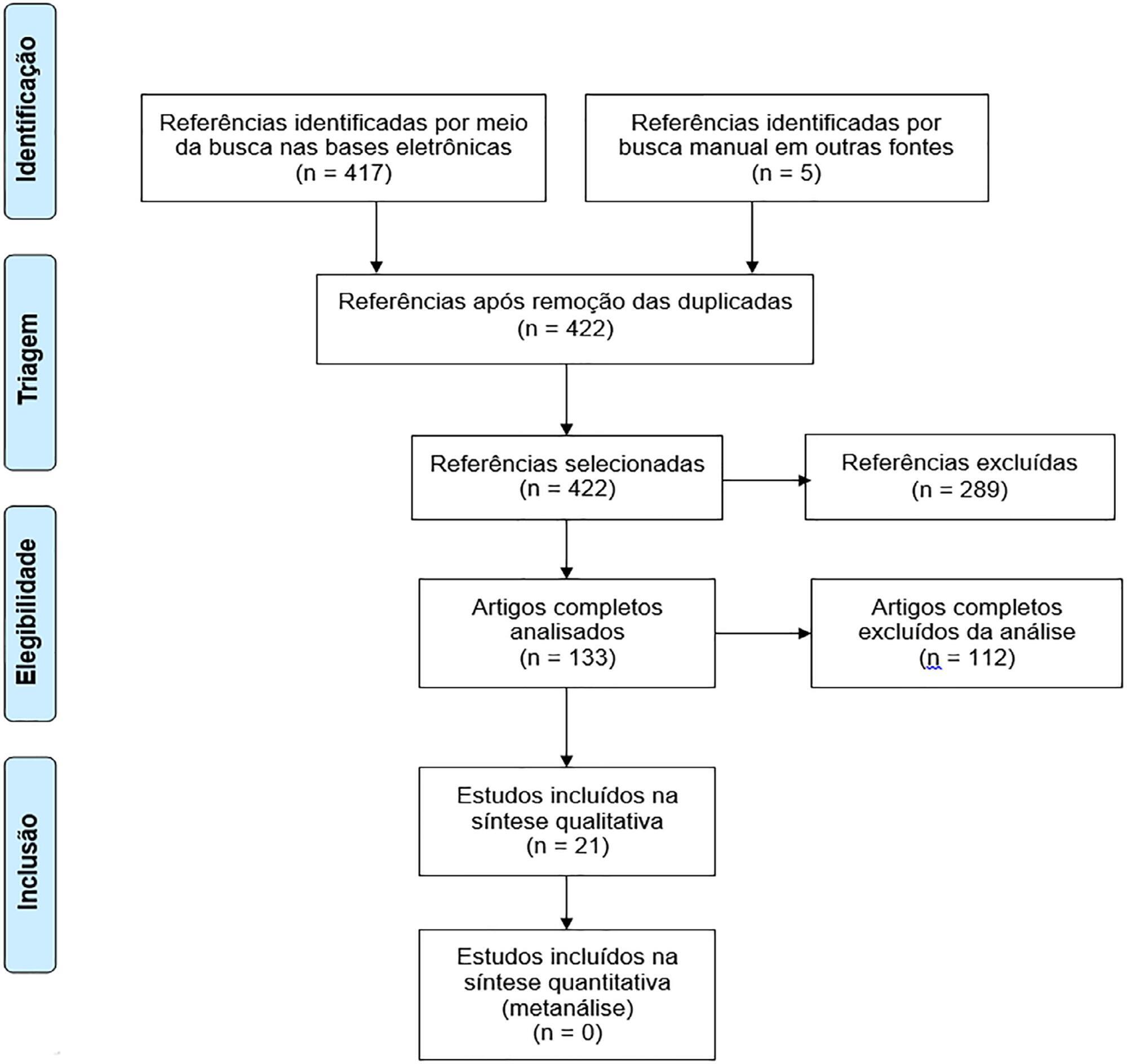
To assess the long-term, health-related quality of life of intensive care unit survivors by systematic review.
The search for, and selection and analysis of, observational studies that assessed the health-related quality of life of intensive care unit survivors in the electronic databases LILACS and MEDLINE® (accessed through PubMed) was performed using the indexed MESH terms "quality of life [MeSH Terms]" AND "critically illness [MeSH Terms]". Studies on adult patients without specific prior diseases published in English in the last 5 years were included in this systematic review. The citations were independently selected by three reviewers. Data were standardly and independently retrieved by two reviewers, and the quality of the studies was assessed using the Newcastle-Ottawa scale.
In total, 19 observational cohort and 2 case-control studies of 57,712 critically ill patients were included. The follow-up time of the studies ranged from 6 months to 6 years, and most studies had a 6-month or 1-year follow up. The health-related quality of life was assessed using two generic tools, the EuroQol and the Short Form Health Survey. The overall quality of the studies was low.
Long-term, health-related quality of life is compromised among intensive care unit survivors compared with the corresponding general population. However, it is not significantly affected by the occurrence of sepsis, delirium, and acute kidney injury during intensive care unit admission when compared with that of critically ill patient control groups. High-quality studies are necessary to quantify the health-related quality of life among intensive care unit survivors.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):460-465
DOI 10.5935/0103-507X.20170066
To evaluate the functional status of pediatric patients after discharge from the pediatric intensive care unit using the Functional Status Scale and to compare the time of invasive mechanical ventilation, length of stay in the pediatric intensive care unit, and Pediatric Index of Mortality 2 results among individuals with different degrees of functional impairment.
A cross-sectional study was conducted on patients who were discharged from a pediatric intensive care unit. The functional evaluation by the Functional Status Scale was performed on the first day after discharge from the unit, and the Pediatric Index of Mortality 2 was used to predict the mortality rate at the time of admission to the pediatric intensive care unit.
The sample consisted of 50 individuals, 60% of which were male, with a median age of 19 [6 - 61] months. The overall score of the Functional Status Scale was 11.5 [7 - 15], and the highest scores were observed in the "motor function" 3 [1 - 4] and "feeding" 4 [1 - 4] domains. Compared to patients who were not readmitted to the pediatric intensive care unit, patients who were readmitted presented a worse overall score (p = 0.01), worse scores in the "motor function" (p = 0.01), "feeding" (p = 0.02), and "respiratory" (p = 0.036) domains, and a higher mortality rate according to the Pediatric Index of Mortality 2 (p = 0.025).
Evaluation of the functional status using the Functional Status Scale indicated moderate impairment in patients after discharge from the pediatric intensive care unit, mainly in the "motor function" and "feeding" domains; patients who were readmitted to the pediatric intensive care unit demonstrated worse overall functional, motor function, feeding and respiratory scores. Individuals with greater functional impairment had longer times of invasive mechanical ventilation and hospitalization in the pediatric intensive care unit.