Abstract
Crit Care Sci. 2023;35(1):44-56
DOI 10.5935/2965-2774.20230340-pt
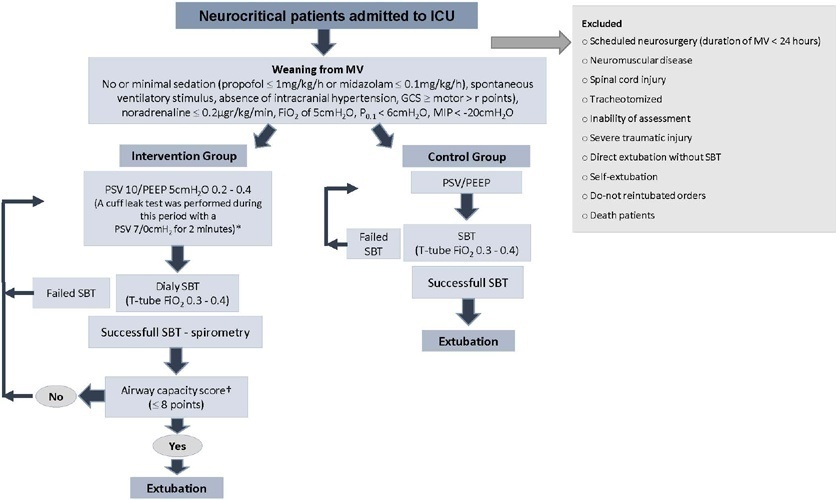
To investigate whether protocol-directed weaning in neurocritical patients would reduce the rate of extubation failure (as a primary outcome) and the associated complications (as a secondary outcome) compared with conventional weaning.
A quasi-experimental study was conducted in a medical-surgical intensive care unit from January 2016 to December 2018. Patients aged 18 years or older with an acute neurological disease who were on mechanical ventilation > 24 hours were included. All patients included in the study were ready to wean, with no or minimal sedation, Glasgow coma score ≥ 9, spontaneous ventilatory stimulus, noradrenaline ≤ 0.2μgr/kg/ minute, fraction of inspired oxygen ≤ 0.5, positive end-expiratory pressure ≤ 5cmH2O, maximal inspiratory pressure < -20cmH2O, and occlusion pressure < 6cmH2O.
Ninety-four of 314 patients admitted to the intensive care unit were included (50 in the Intervention Group and 44 in the Control Group). There was no significant difference in spontaneous breathing trial failure (18% in the Intervention Group versus 34% in the Control Group, p = 0.12). More patients in the Intervention Group were extubated than in the Control Group (100% versus 79%, p = 0.01). The rate of extubation failure was not signifiantly diffrent between the groups (18% in the Intervention Group versus 17% in the Control Group; relative risk 1.02; 95%CI 0.64 - 1.61; p = 1.00). The reintubation rate was lower in the Control Group (16% in the Intervention Group versus 11% in the Control Group; relative risk 1.15; 95%CI 0.74 - 1.82; p = 0.75). The need for tracheotomy was lower in the Intervention Group [4 (8%) versus 11 (25%) in the Control Group; relative risk 0.32; 95%CI 0.11 - 0.93; p = 0.04]. At Day 28, the patients in the Intervention Group had more ventilator-free days than those in the Control Group [28 (26 - 28) days versus 26 (19 - 28) days; p = 0.01]. The total duration of mechanical ventilation was shorter in the Intervention Group than in the Control Group [5 (2 - 13) days versus 9 (3 - 22) days; p = 0.01]. There were no diffrences in the length of intensive care unit stay, 28-day free from mechanical ventilation, hospital stay or 90-day mortality.
Considering the limitations of our study, the application of a weaning protocol for neurocritical patients led to a high percentage of extubation, a reduced need for tracheotomy and a shortened duration of mechanical ventilation. However, there was no reduction in extubation failure or the 28-day free of from mechanical ventilation compared with the Control Group.
Abstract
Crit Care Sci. 2023;35(1):57-65
DOI 10.5935/2965-2774.20230350-pt
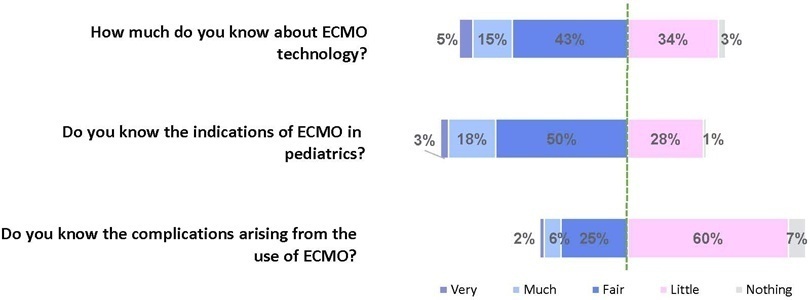
To assess Brazilian pediatric intensivists’ general knowledge of extracorporeal membrane oxygenation, including evidence for its use, the national funding model, indications, and complications.
This was a multicenter cross-sectional survey including 45 Brazilian pediatric intensive care units. A convenience sample of 654 intensivists was surveyed regarding their knowledge on managing patients on extracorporeal membrane oxygenation, its indications, complications, funding, and literature evidence.
The survey addressed questions regarding the knowledge and experience of pediatric intensivists with extracorporeal membrane oxygenation, including two clinical cases and 6 optional questions about the management of patients on extracorporeal membrane oxygenation. Of the 45 invited centers, 42 (91%) participated in the study, and 412 of 654 (63%) pediatric intensivists responded to the survey. Most pediatric intensive care units were from the Southeast region of Brazil (59.5%), and private/for-profit hospitals represented 28.6% of the participating centers. The average age of respondents was 41.4 (standard deviation 9.1) years, and the majority (77%) were women. Only 12.4% of respondents had taken an extracorporeal membrane oxygenation course. Only 19% of surveyed hospitals have an extracorporeal membrane oxygenation program, and only 27% of intensivists reported having already managed patients on extracorporeal membrane oxygenation. Specific extracorporeal membrane oxygenation management questions were responded to by only 64 physicians (15.5%), who had a fair/good correct response rate (median 63.4%; range 32.8% to 91.9%).
Most Brazilian pediatric intensivists demonstrated limited knowledge regarding extracorporeal membrane oxygenation, including its indications and complications. Extracorporeal membrane oxygenation is not yet widely available in Brazil, with few intensivists prepared to manage patients on extracorporeal membrane oxygenation and even fewer intensivists recognizing when to refer patients to extracorporeal membrane oxygenation centers.
Abstract
Crit Care Sci. 2023;35(1):66-72
DOI 10.5935/2965-2774.20230312-pt
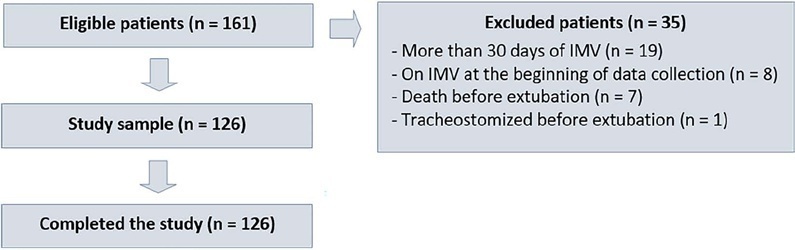
To evaluate whether a model of a daily fitness checklist for spontaneous breathing tests is able to identify predictive variables of extubation failure in pediatric patients admitted to a Brazilian intensive care unit.
This was a single-center, cross-sectional study with prospective data collection. The checklist model comprised 20 items and was applied to assess the ability to perform spontaneous breathing tests.
The sample consisted of 126 pediatric patients (85 males (67.5%)) on invasive mechanical ventilation, for whom 1,217 daily assessments were applied at the bedside. The weighted total score of the prediction model showed the highest discriminatory power for the spontaneous breathing test, with sensitivity and specificity indices for fitness failure of 89.7% or success of 84.6%. The cutoff point suggested by the checklist was 8, with a probability of extubation failure less than 5%. Failure increased progressively with increasing score, with a maximum probability of predicting extubation failure of 85%.
The extubation failure rate with the use of this model was within what is acceptable in the literature. The daily checklist model for the spontaneous breathing test was able to identify predictive variables of failure in the extubation process in pediatric patients.
Abstract
Crit Care Sci. 2023;35(1):73-83
DOI 10.5935/2965-2774.20230374-pt
To understand the perception of medical communication and needs of family members with loved ones in intensive care.
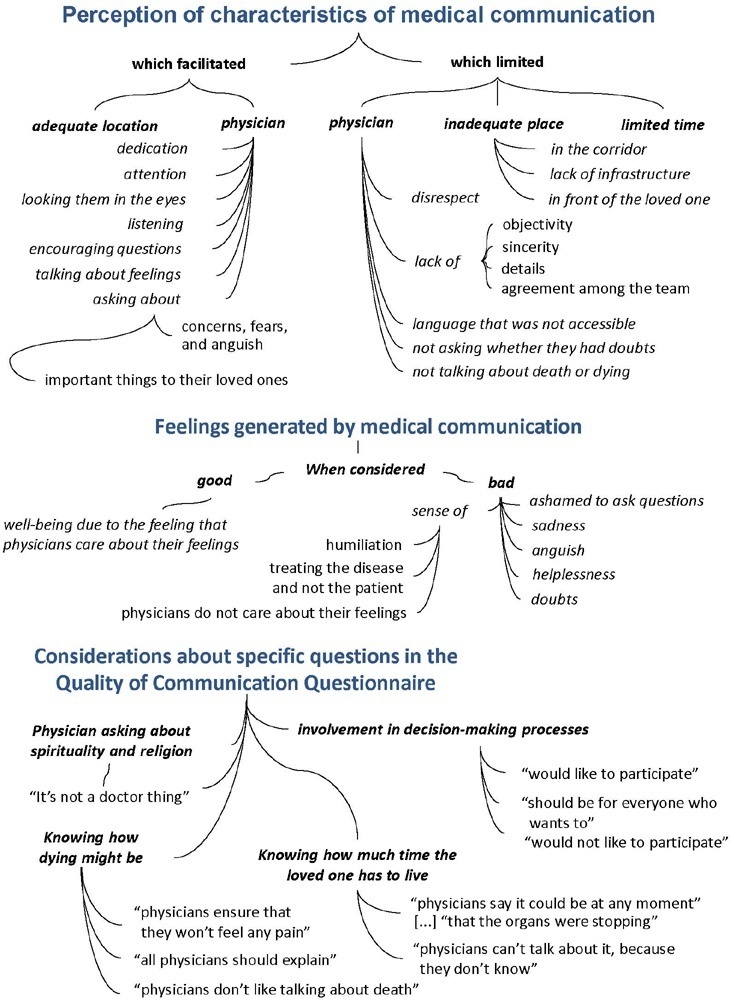
The study was mainly qualitative and exploratory, with thematic analysis of comments made by 92 family members with loved ones in intensive care units when answering in-person interviews comprising the Quality of Communication Questionnaire (QoC) and open-ended questions about their need for additional help, the appropriateness of the place where they received information, and additional comments.
The participants’ mean age was 46.8 years (SD = 11.8), and most of them were female, married and had incomplete or completed elementary education. The following themes were found: perception of characteristics of medical communication; feelings generated by communication; considerations about specific questions in the QoC; family members’ needs; and strategies to overcome needs regarding communication. Characteristics that facilitated communication included attention and listening. Characteristics that made communication difficult included aspects of information sharing, such as inaccessible language; lack of clarity, objectivity, sincerity, and agreement among the team; limited time; and inadequate location. Feelings such as shame, helplessness, and sadness were cited when communication was inadequate. Family members’ needs related to communication included more details about the loved one’s diagnosis, prognosis, and health condition; participation in decisionmaking; and being asked about feelings, spirituality, dying and death. Others were related to longer visitation time, psychological support, social assistance, and better infrastructure.
It is necessary to enhance medical communication and improve hospital infrastructure to improve the quality of care for family members.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):402-409
DOI 10.5935/0103-507X.20220299-en
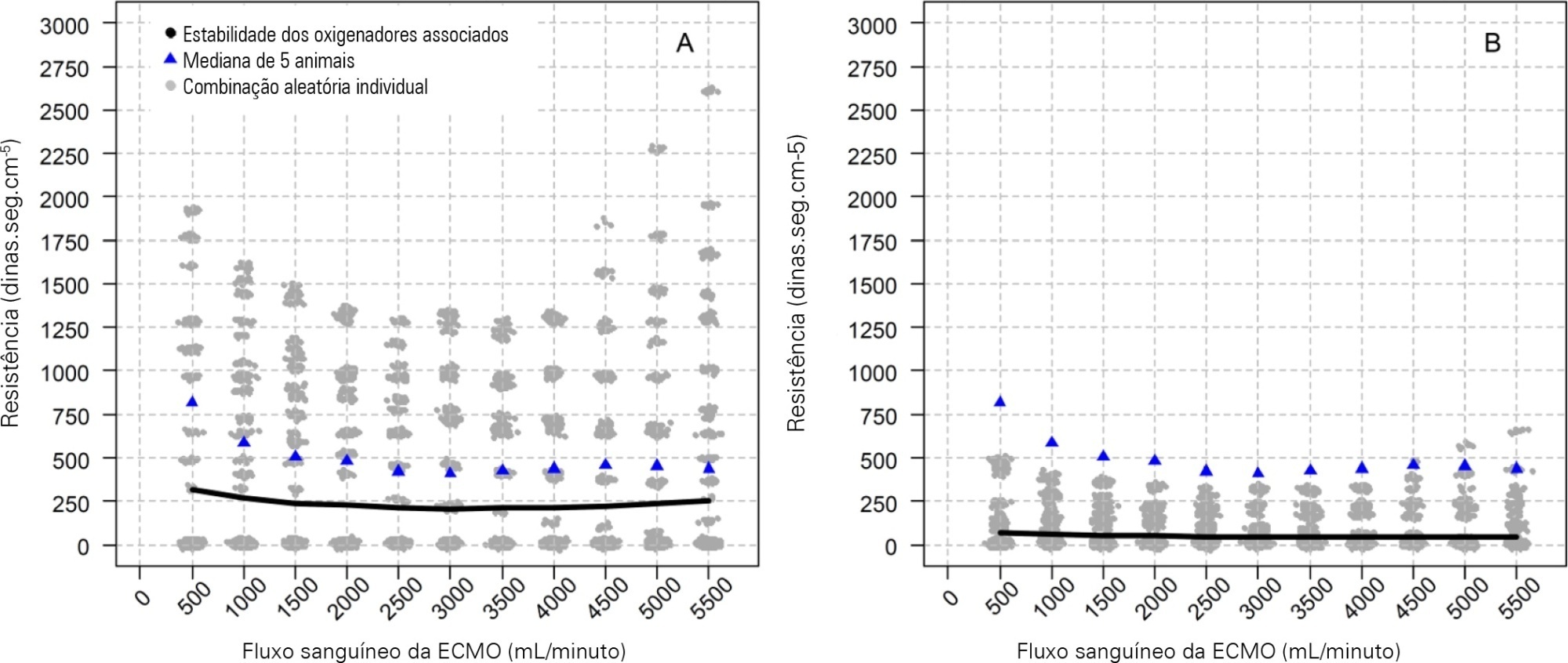
To characterize the pressures, resistances, oxygenation, and decarboxylation efficacy of two oxygenators associated in series or in parallel during venous-venous extracorporeal membrane oxygenation support.
Using the results of a swine severe respiratory failure associated with multiple organ dysfunction venous-venous extracorporeal membrane oxygenation support model and mathematical modeling, we explored the effects on oxygenation, decarboxylation and circuit pressures of in-parallel and in-series associations of oxygenators.
Five animals with a median weight of 80kg were tested. Both configurations increased the oxygen partial pressure after the oxygenators. The return cannula oxygen content was also slightly higher, but the impact on systemic oxygenation was minimal using oxygenators with a high rated flow (~ 7L/minute). Both configurations significantly reduced the systemic carbon dioxide partial pressure. As the extracorporeal membrane oxygenation blood flow increased, the oxygenator resistance decreased initially with a further increase with higher blood flows but with a small clinical impact.
Association of oxygenators in parallel or in series during venous-venous extracorporeal membrane oxygenation support provides a modest increase in carbon dioxide partial pressure removal with a slight improvement in oxygenation. The effect of oxygenator associations on extracorporeal circuit pressures is minimal.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):461-468
DOI 10.5935/0103-507X.20220132-en
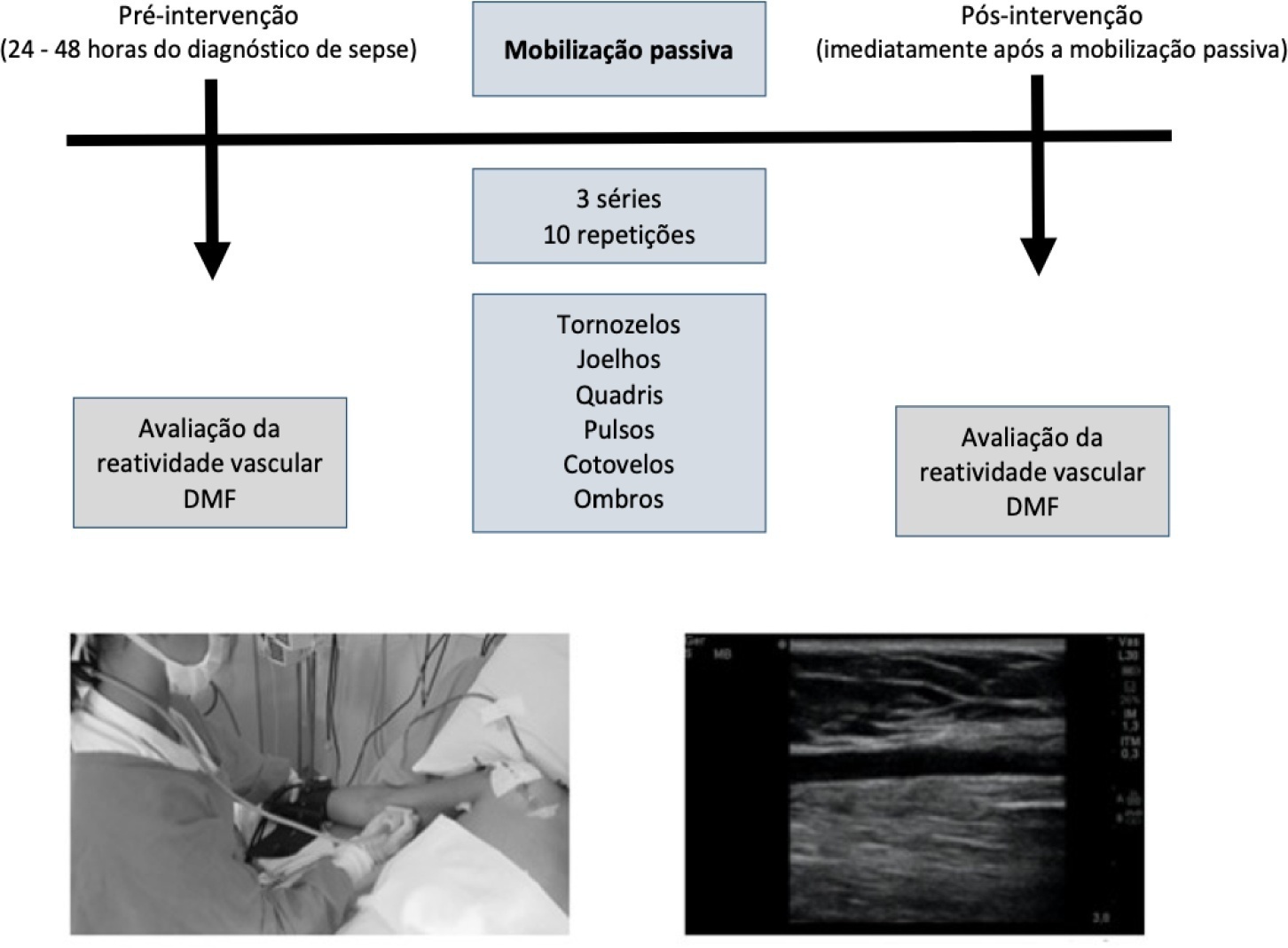
To investigate the influence of a passive mobilization session on endothelial function in patients with sepsis.
This was a quasi-experimental double-blind and single-arm study with a pre- and postintervention design. Twenty-five patients with a diagnosis of sepsis who were hospitalized in the intensive care unit were included. Endothelial function was assessed at baseline (preintervention) and immediately postintervention by brachial artery ultrasonography. Flow mediated dilatation, peak blood flow velocity and peak shear rate were obtained. Passive mobilization consisted of bilateral mobilization (ankles, knees, hips, wrists, elbows and shoulders), with three sets of ten repetitions each, totaling 15 minutes.
After mobilization, we found increased vascular reactivity function compared to preintervention: absolute flow-mediated dilatation (0.57mm ± 0.22 versus 0.17mm ± 0.31; p < 0.001) and relative flow-mediated dilatation (17.1% ± 8.25 versus 5.08% ± 9.16; p < 0.001). Reactive hyperemia peak flow (71.8cm/s ± 29.3 versus 95.3cm/s ± 32.2; p < 0.001) and shear rate (211s ± 113 versus 288s ± 144; p < 0.001) were also increased.
A passive mobilization session increases endothelial function in critical patients with sepsis. Future studies should investigate whether a mobilization program can be applied as a beneficial intervention for clinical improvement of endothelial function in patients hospitalized due to sepsis.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):410-417
DOI 10.5935/0103-507X.20220261-en
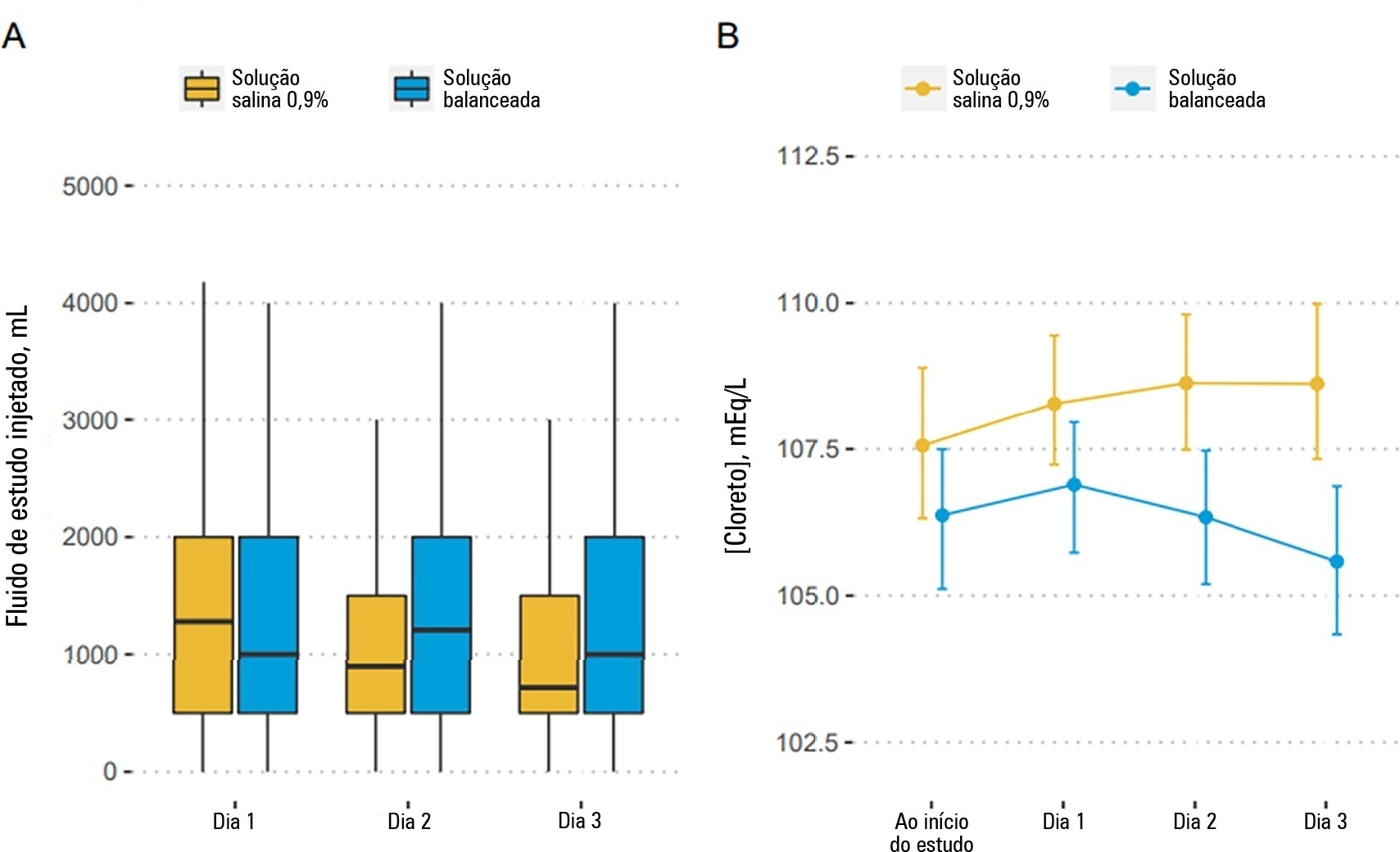
To describe the effects of balanced solution use on the short-term outcomes of patients with traumatic brain injury enrolled in BaSICS trial.
Patients were randomized to receive either 0.9% saline or balanced solution during their intensive care unit stay. The primary endpoint was 90-day mortality, and the secondary outcomes were days alive and free of intensive care unit stay at 28 days. The primary endpoint was assessed using Bayesian logistic regression. The secondary endpoint was assessed using a Bayesian zero-inflated beta binomial regression.
We included 483 patients (236 in the 0.9% saline arm and 247 in the balanced solution arm). A total of 338 patients (70%) with a Glasgow coma scale score ≤ 12 were enrolled. The overall probability that balanced solutions were associated with higher 90-day mortality was 0.98 (OR 1.48; 95%CrI 1.04 - 2.09); this mortality increment was particularly noticeable in patients with a Glasgow coma scale score below 6 at enrollment (probability of harm of 0.99). Balanced solutions were associated with -1.64 days alive and free of intensive care unit at 28 days (95%CrI -3.32 - 0.00) with a probability of harm of 0.97.
There was a high probability that balanced solutions were associated with high 90-day mortality and fewer days alive and free of intensive care units at 28 days.
Abstract
Rev Bras Ter Intensiva. 2022;34(4):469-476
DOI 10.5935/0103-507X.20220429-en
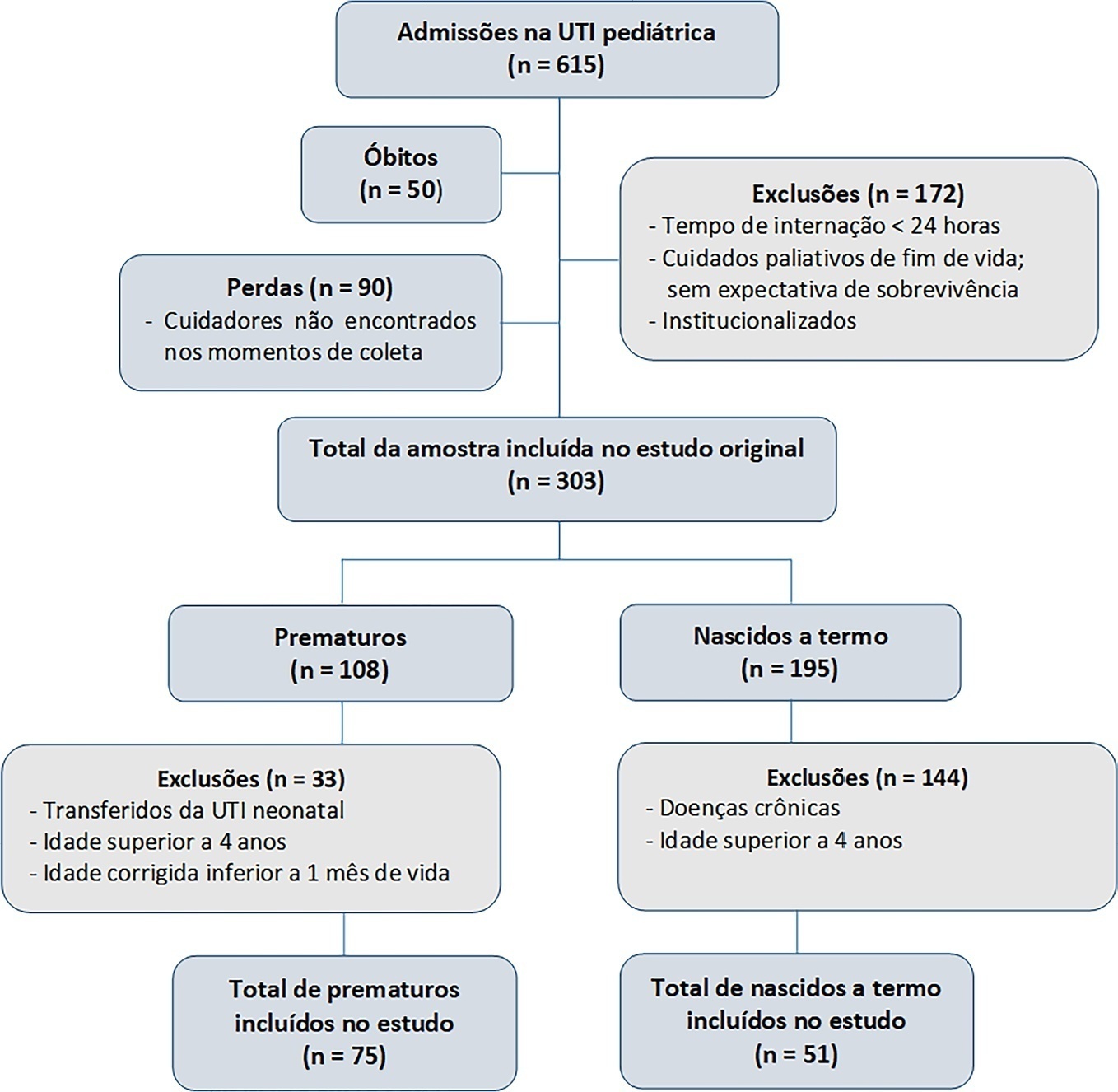
To evaluate the effects of critical illness on the functional status of children aged zero to 4 years with or without a history of prematurity after discharge from the pediatric intensive care unit.
This was a secondary cross-sectional study nested in an observational cohort of survivors from a pediatric intensive care unit. Functional assessment was performed using the Functional Status Scale within 48 hours after discharge from the pediatric intensive care unit.
A total of 126 patients participated in the study, 75 of whom were premature, and 51 of whom were born at term. Comparing the baseline and functional status at pediatric intensive care unit discharge, both groups showed significant differences (p < 0.001). Preterm patients exhibited greater functional decline at discharge from the pediatric intensive care unit (61%). Among patients born at term, there was a significant correlation between the Pediatric Index of Mortality, duration of sedation, duration of mechanical ventilation and length of hospital stay with the functional outcomes (p = 0.05).
Most patients showed a functional decline at discharge from the pediatric intensive care unit. Although preterm patients had a greater functional decline at discharge, sedation and mechanical ventilation duration influenced functional status among patients born at term.