Abstract
Rev Bras Ter Intensiva. 2021;33(3):346-352
DOI 10.5935/0103-507X.20210053
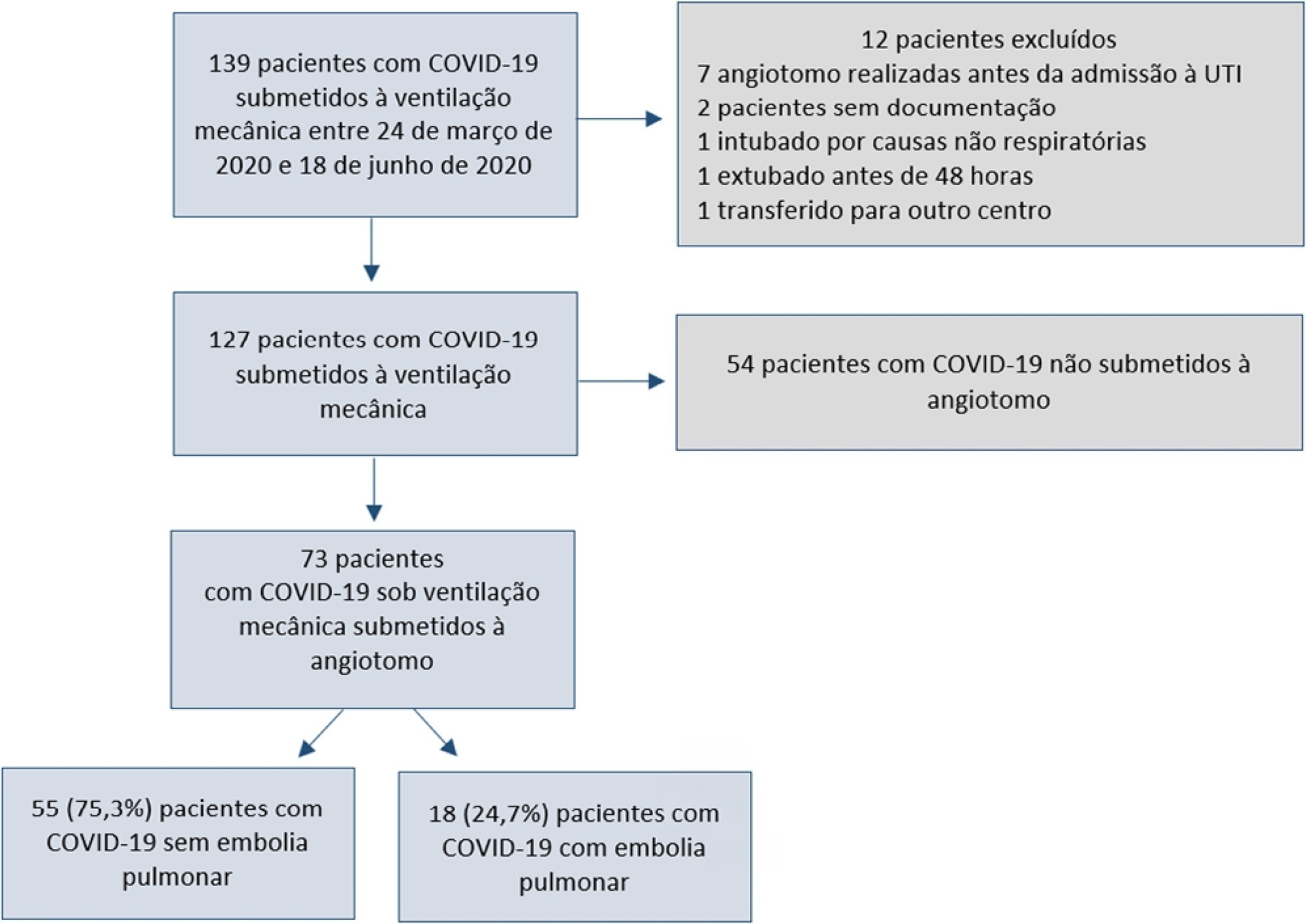
To assess pulmonary embolism incidence, its relationship with D-dimer levels and other possible associated factors in addition to anticoagulation and contrast medium adverse effects.
A retrospective observational cohort study at a Chilean public hospital was performed. Intensive care unit mechanically ventilated COVID-19 patients older than 18 years old between March and June 2020 were included. All patients received heparin thromboprophylaxis, which was increased to the anticoagulation dose with D-dimer greater than 3µg/mL.
A total of 127 patients were followed up, of whom 73 underwent pulmonary computed tomography angiography (mean age, 54 ± 12 years; 49 men). Sixty-two of the 73 patients (84.9%) received full anticoagulation before computed tomography angiography. In addition, 18 of the 73 patients had pulmonary embolism (24.7%). When comparing patients with and without pulmonary embolism, no significant differences were observed in age, sex, obesity, smoking, Wells and revised Geneva scores, D-dimer or mortality. Anticoagulant use was similar in both groups. Days from the start of anticoagulation until computed tomography angiography were significantly lower in the pulmonary embolism group (p = 0.002). Three patients presented post contrast-acute kidney injury (4.1%), and one patient had major bleeding.
Despite anticoagulation, one in four COVID-19 patients connected to mechanical ventilation and evaluated with pulmonary computed tomography angiography had pulmonary embolism. With a longer the delay in performing computed tomography angiography once empirical anticoagulation was started, significantly less pulmonary embolism was identified.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):362-373
DOI 10.5935/0103-507X.20210059
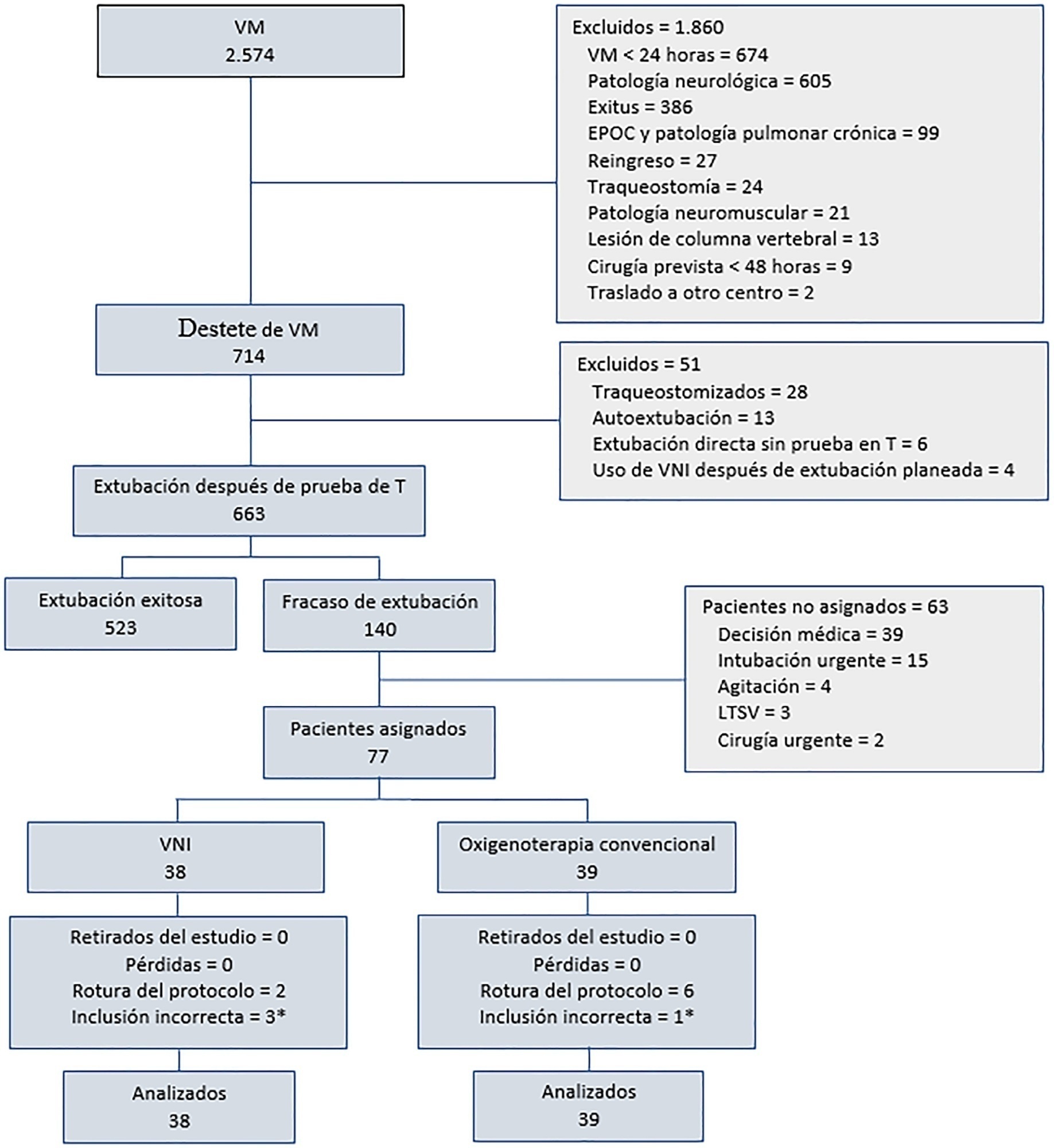
To determine the effectiveness of noninvasive ventilation versus conventional oxygen therapy in patients with acute respiratory failure after extubation failure.
A pragmatic clinical trial was conducted in an intensive care unit from March 2009 to September 2016. Patients on mechanical ventilation > 24 hours who developed acute respiratory failure after scheduled extubation were included and were assigned to noninvasive ventilation or conventional oxygen therapy. The primary objective was to reduce the reintubation rate. The secondary objectives were to improve respiratory parameters and reduce complications, the duration of mechanical ventilation, the intensive care unit stay, the hospital stay, and mortality in the intensive care unit, in the hospital, and 90 days after discharge. Factors correlated with reintubation were also analyzed.
Of a total of 2,574 patients, 77 were analyzed (38 in the noninvasive ventilation group and 39 in the conventional oxygen therapy group). Noninvasive ventilation reduced the respiratory and cardiac rates more rapidly than conventional oxygen therapy. Reintubation was less common in the noninvasive ventilation group [12 (32%) versus 22 (56%) in the conventional oxygen therapy group, relative risk 0.58 (95%CI 0.34 - 0.97), p = 0.039]. The rest of the parameters did not show significant differences. In the multivariate analysis, noninvasive ventilation protected against reintubation [OR 0.17 (95%CI 0.05 - 0.56), p = 0.004], while liver failure before extubation and the inability to maintain airway patency predisposed patients to reintubation.
The use of noninvasive ventilation in patients who failed extubation could be beneficial compared to conventional oxygen therapy.
Abstract
Rev Bras Ter Intensiva. 2021;33(3):422-427
DOI 10.5935/0103-507X.20210057
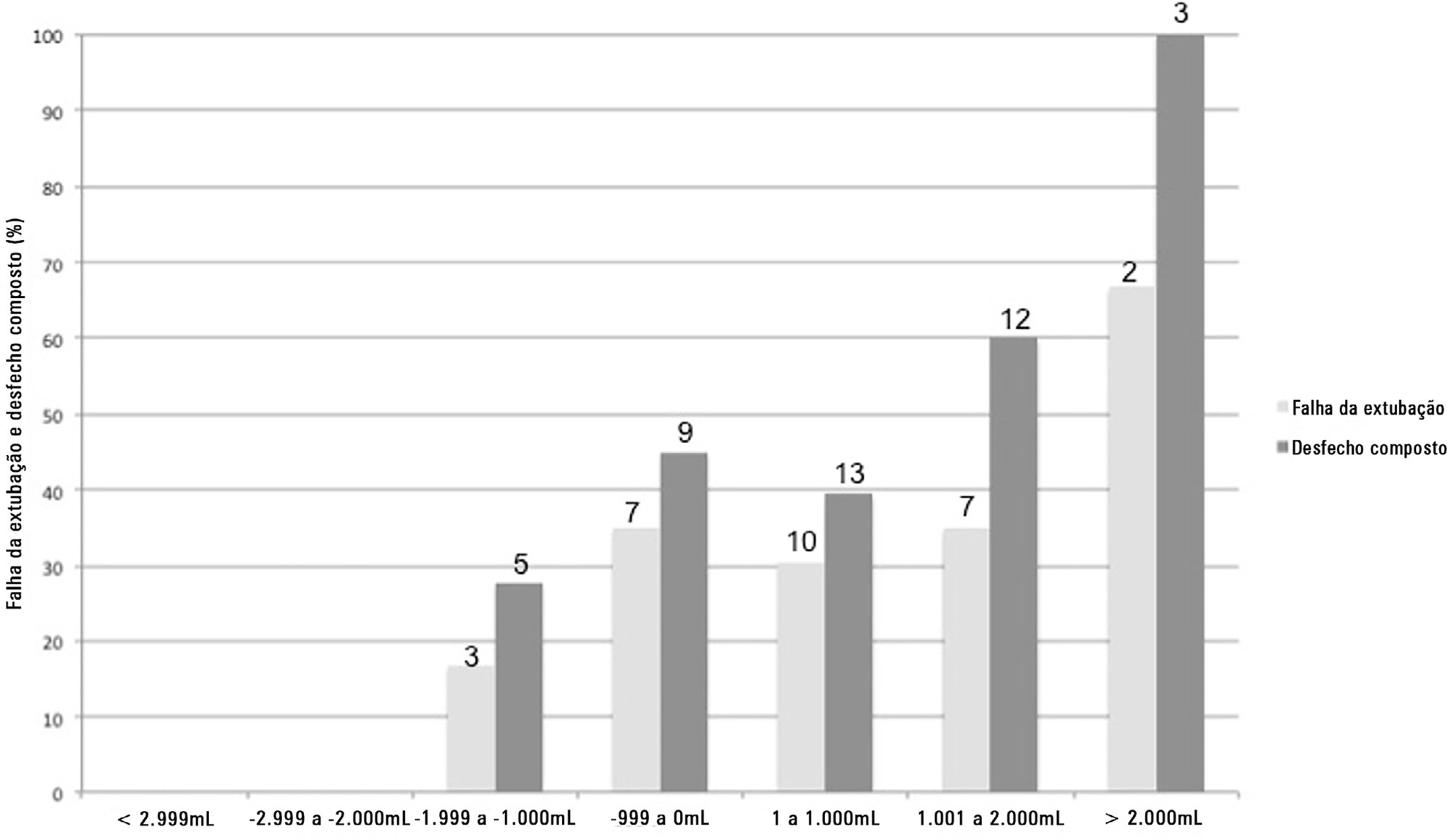
To assess whether there is an association between 48-hour postextubation fluid balance and extubation failure.
This was a prospective cohort study that included patients admitted to the intensive care unit of a tertiary hospital in southern Brazil from March 2019 to December 2019. Patients who required mechanical ventilation for at least 24 hours and who were extubated during the study period were included. The primary outcome was extubation failure, considered as the need for reintubation in the first 72 hours after extubation. The secondary outcome was a combined outcome with extubation failure or the need for therapeutic noninvasive ventilation.
A total of 101 patients were included. Extubation failure was observed in 29 (28.7%) patients. In univariate analysis, patients with a negative 48-hour postextubation fluid balance higher than one liter had a lower rate of extubation failure (12.0%) than patients with a negative 48-hour postextubation fluid balance lower than 1L (34.2%; p = 0.033). Mechanical ventilation duration and negative 48-hour postextubation fluid balance lower than one liter were associated with extubation failure when corrected for Simplified Acute Physiology Score 3 in multivariate analysis. When we evaluated the combined outcome, only negative 48-hour postextubation lower than 1L maintained an association when corrected for for Simplified Acute Physiology Score 3 and mechanical ventilation duration.
The 48-hour postextubation fluid balance is associated with extubation failure. Further studies are necessary to assess whether avoiding positive fluid balance in this period might improve weaning outcomes.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):188-195
DOI 10.5935/0103-507X.20210026
To describe the usual practice of mobility therapy in the adult intensive care unit for patients with and without COVID-19.
Online survey in which physical therapists working in an adult intensive care unit in Argentina participated. Sixteen multiple-choice or single-response questions grouped into three sections were asked. The first section addressed personal, professional and work environment data. The second section presented questions regarding usual care, and the third focused on practices under COVID-19 pandemic conditions.
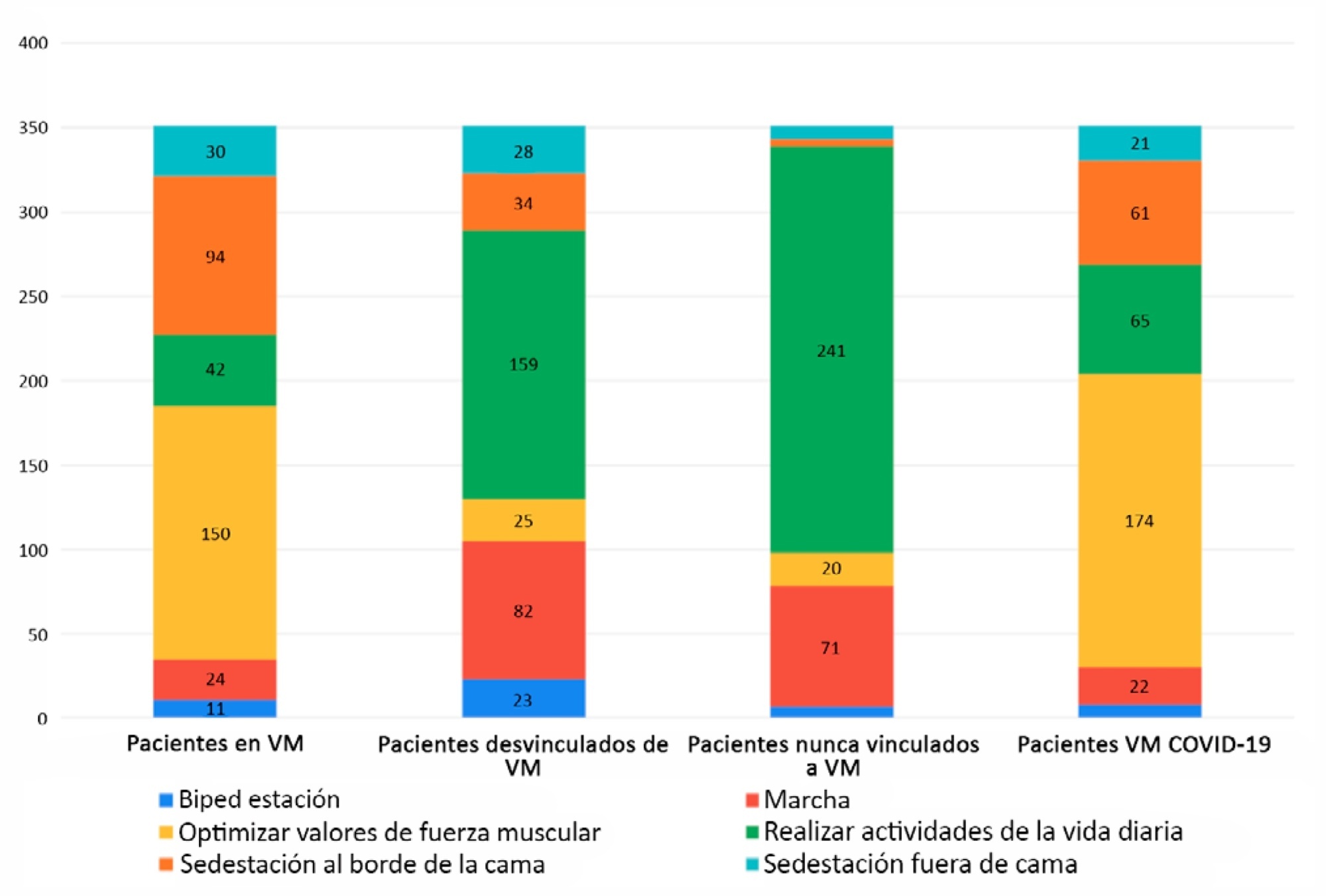
Of 351 physical therapists, 76.1% answer that they were exclusively responsible for patient mobility. The highest motor-based goal varied according to four patient scenarios: Mechanically ventilated patients, patients weaned from mechanical ventilation, patients who had never required mechanical ventilation, and patients with COVID-19 under mechanical ventilation. In the first and last scenarios, the highest goal was to optimize muscle strength, while for the other two, it was to perform activities of daily living. Finally, the greatest limitation in working with patients with COVID-19 was respiratory and/or contact isolation.
Physical therapists in Argentina reported being responsible for the mobility of patients in the intensive care unit. The highest motor-based therapeutic goals for four classic scenarios in the closed area were limited by the need for mechanical ventilation. The greatest limitation when mobilizing patients with COVID-19 was respiratory and contact isolation.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):243-250
DOI 10.5935/0103-507X.20210031
To relate functional independence to the degree of pulmonary impairment in adult patients 3 months after discharge from the intensive care unit.
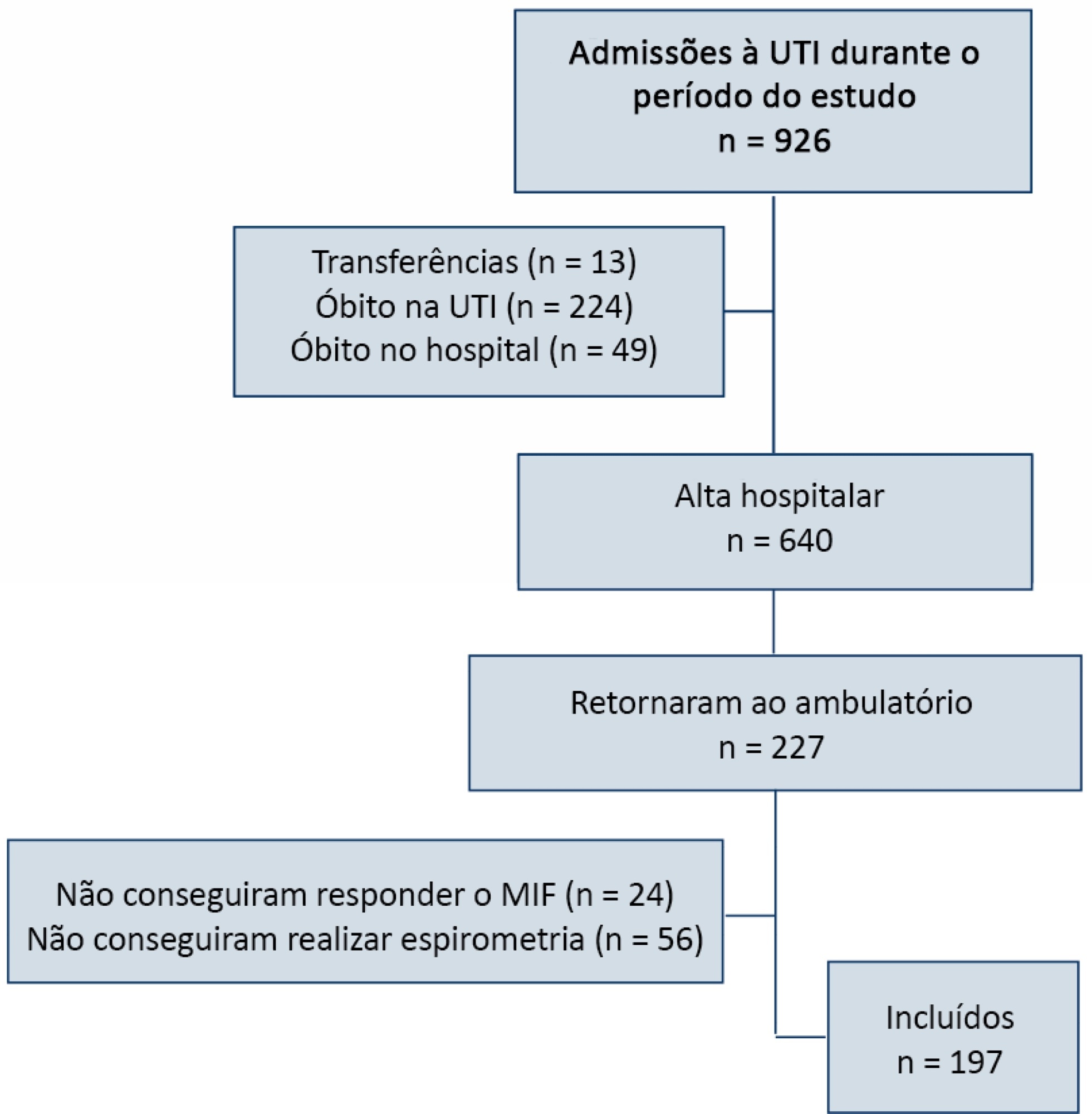
This was a retrospective cohort study conducted in one adult intensive care unit and a multi-professional post-intensive care unit outpatient clinic of a single center. Patients admitted to the intensive care unit from January 2012 to December 2013 who underwent (3 months later) spirometry and answered the Functional Independence Measure Questionnaire were included.
Patients were divided into groups according to the classification of functional independence and spirometry. The study included 197 patients who were divided into greater dependence (n = 4), lower dependence (n = 12) and independent (n = 181) groups. Comparing the three groups, regarding the classification of the Functional Independence Measure, patients with greater dependence had higher Acute Physiology and Chronic Health Evaluation II and Sequential Organ Failure Assessment values at intensive care unit admission with more advanced age, more days on mechanical ventilation, and longer stay in the intensive care unit and hospital. The majority of patients presented with pulmonary impairment, which was the obstructive pattern observed most frequently. When comparing functional independence with pulmonary function, it was observed that the lower the functional status, the worse the pulmonary function, with a significant difference being observed in peak expiratory flow (p = 0.030).
The majority of patients who returned to the outpatient clinic 3 months after discharge had good functional status but did present with pulmonary impairment, which is related to the degree of functional dependence.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):261-265
DOI 10.5935/0103-507X.20210033
To identify the possible association between driving pressure and mechanical power values and oxygenation index on the first day of mechanical ventilation with the mortality of trauma patients without a diagnosis of acute respiratory distress syndrome.
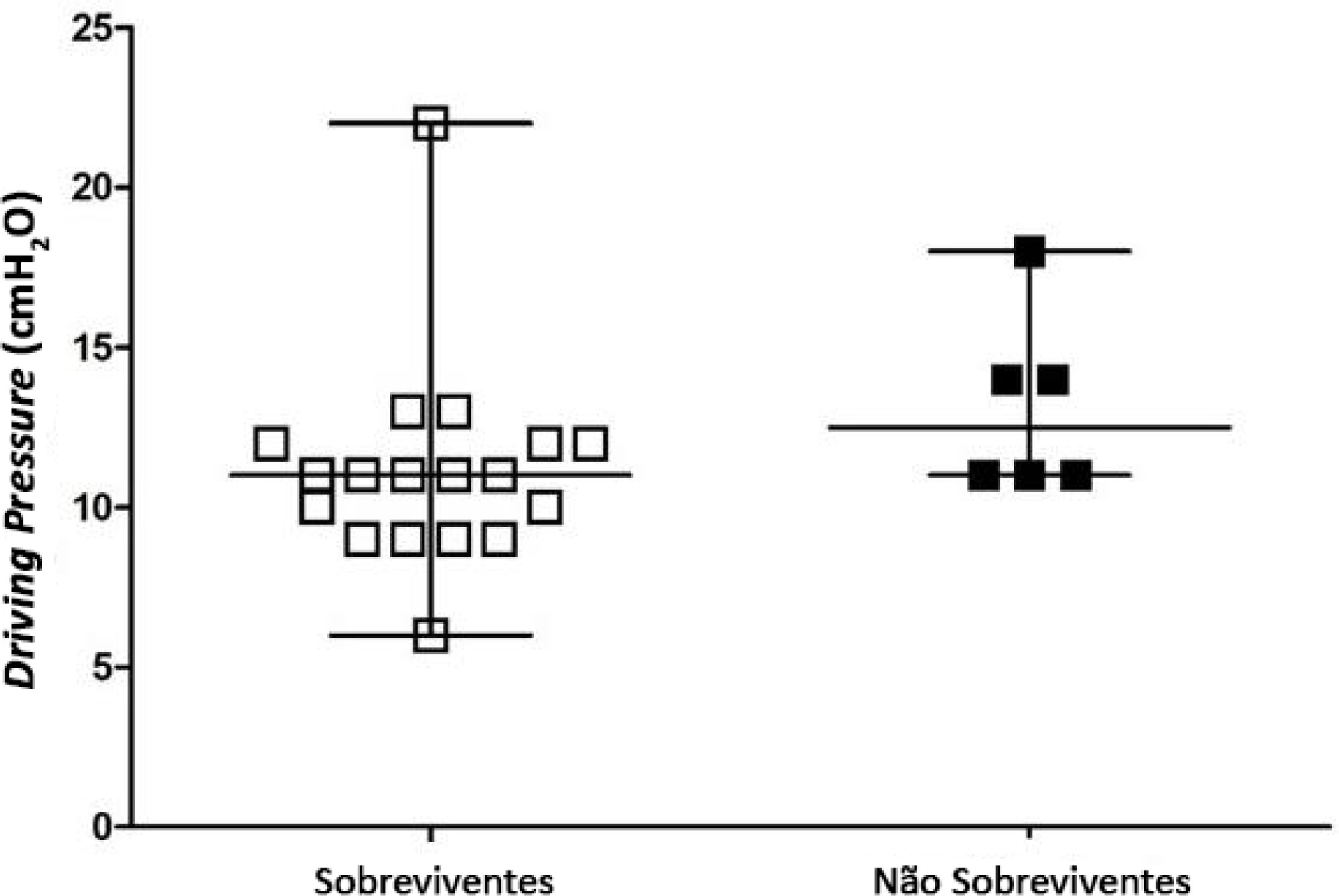
Patients under pressure-controlled or volume-controlled ventilation were included, with data collection 24 hours after orotracheal intubation. Patient follow-up was performed for 30 days to obtain the clinical outcome. The patients were admitted to two intensive care units of the Hospital de Pronto Socorro de Porto Alegre from June to September 2019.
A total of 24 patients were evaluated. Driving pressure, mechanical power and oxygenation index were similar among patients who survived and those who died, with no statistically significant difference between groups.
Driving pressure, mechanical power and oxygenation index values obtained on the first day of mechanical ventilation were not associated with mortality of trauma patients without acute respiratory distress syndrome.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):304-311
DOI 10.5935/0103-507X.20210039
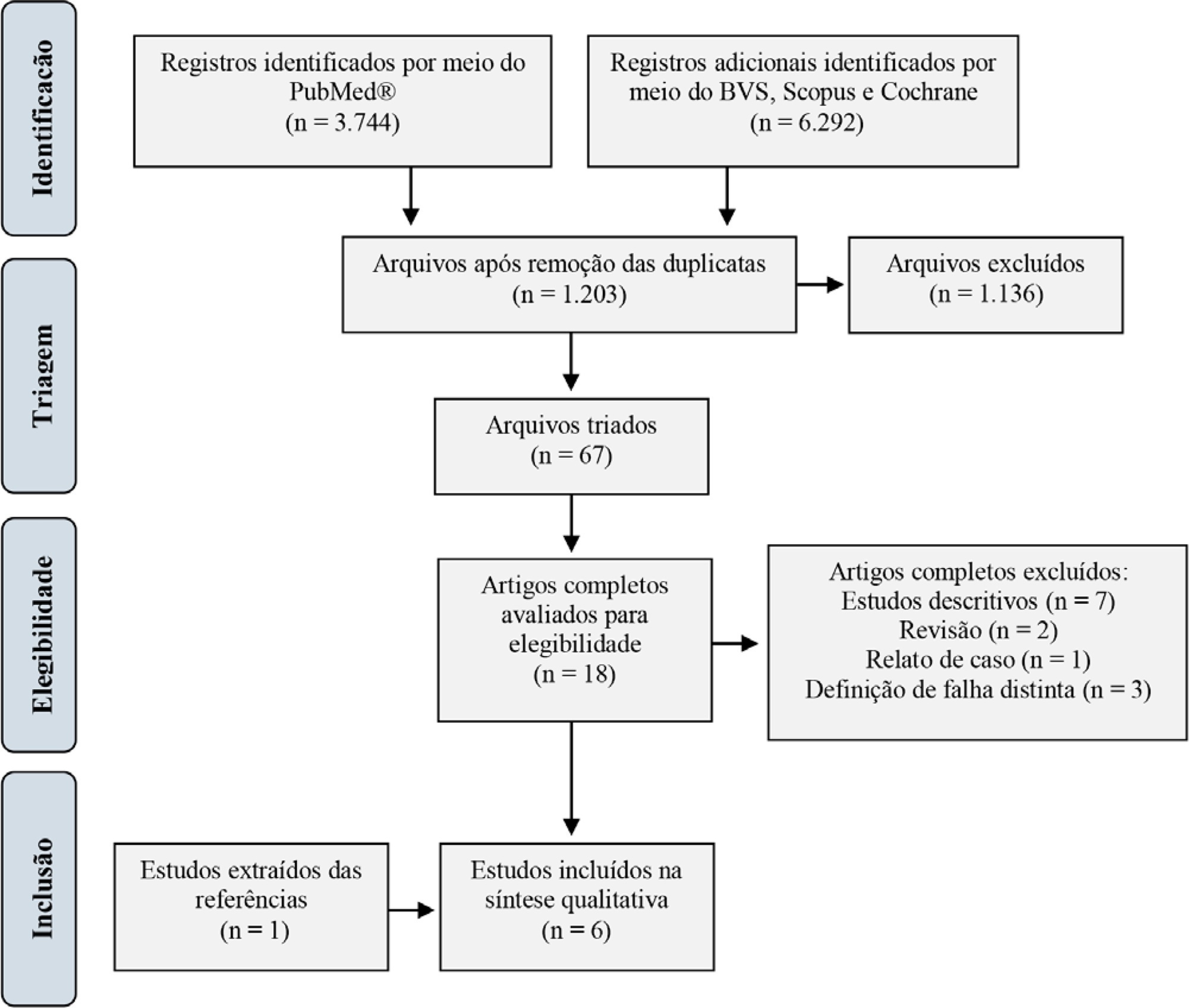
For extubation in pediatric patients, the evaluation of readiness is strongly recommended. However, a device or practice that is superior to clinical judgment has not yet been accurately determined. Thus, it is important to conduct a review on the techniques of choice in clinical practice to predict extubation failure in pediatric patients. Based on a search in the PubMed®, Biblioteca Virtual em Saúde, Cochrane Library and Scopus databases, we conducted a survey of the predictive variables of extubation failure most commonly used in clinical practice in pediatric patients. Of the eight predictors described, the three most commonly used were the spontaneous breathing test, the rapid shallow breathing index and maximum inspiratory pressure. Although the disparity of the data presented in the studies prevented statistical treatment, it was still possible to describe and analyze the performance of these tests.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):48-67
DOI 10.5935/0103-507X.20210005
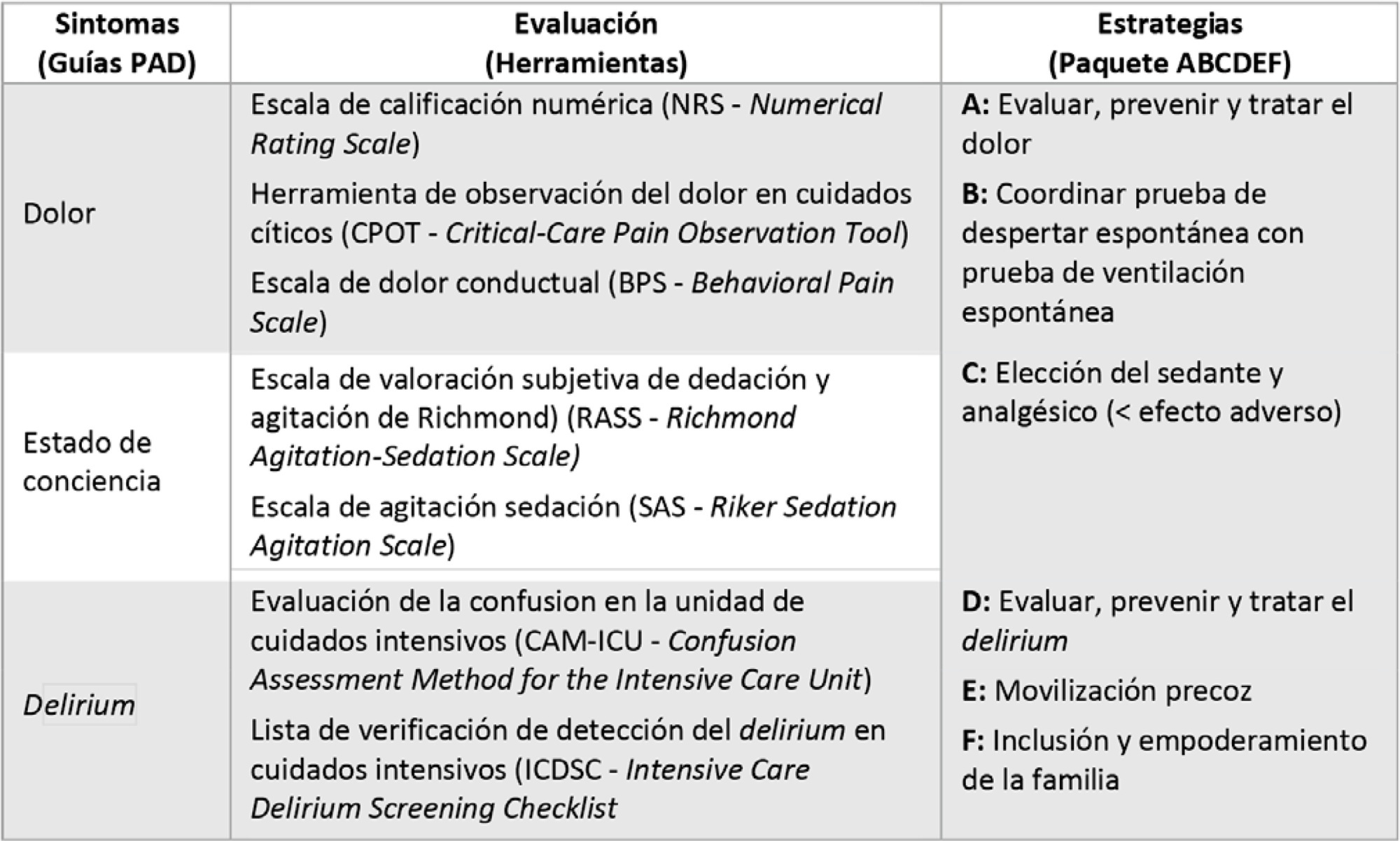
To propose agile strategies for a comprehensive approach to analgesia, sedation, delirium, early mobility and family engagement for patients with COVID-19-associated acute respiratory distress syndrome, considering the high risk of infection among health workers, the humanitarian treatment that we must provide to patients and the inclusion of patients’ families, in a context lacking specific therapeutic strategies against the virus globally available to date and a potential lack of health resources.
A nonsystematic review of the scientific evidence in the main bibliographic databases was carried out, together with national and international clinical experience and judgment. Finally, a consensus of recommendations was made among the members of the Committee for Analgesia, Sedation and Delirium of the Sociedad Argentina de Terapia Intensiva.
Recommendations were agreed upon, and tools were developed to ensure a comprehensive approach to analgesia, sedation, delirium, early mobility and family engagement for adult patients with acute respiratory distress syndrome due to COVID-19.
Given the new order generated in intensive therapies due to the advancing COVID-19 pandemic, we propose to not leave aside the usual good practices but to adapt them to the particular context generated. Our consensus is supported by scientific evidence and national and international experience and will be an attractive consultation tool in intensive therapies.