Abstract
Rev Bras Ter Intensiva. 2010;22(1):40-46
DOI 10.1590/S0103-507X2010000100008
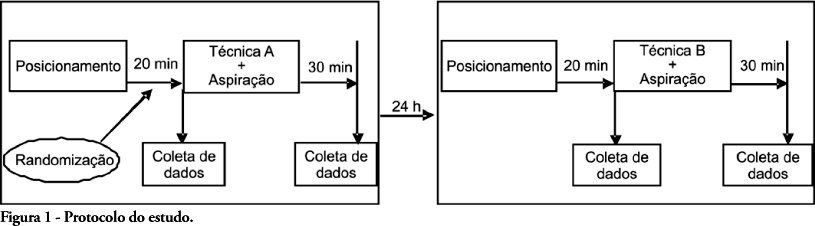
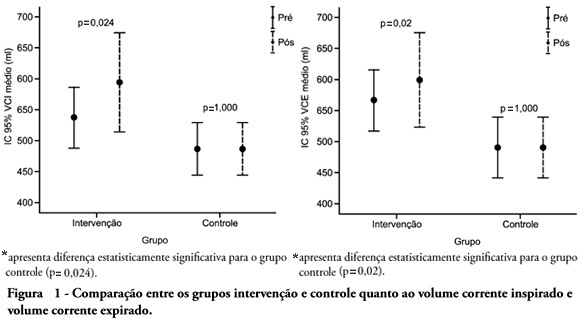
OBJECTIVE: To verify the effects of manual hyperinflation maneuver associated with positive end expiratory pressure in coronary artery bypass grafting patients. METHODS: This was a randomized trial, conducted from August 2007 to July 2008 in the intensive care unit of the Hospital Luterano (ULBRA). The patients were divided in the groups intervention - with manual hyperinflation plus positive end expiratory pressure - and controlThe ventilatory variables were measured before and after the manual hyperinflation. The t Student's test was used for independent and paired samples as well as Fisher's exact test and McNemar's Chi-square test with 0.05 significance level. RESULTS: Eighteen patients were included. The mean age was 64± 11 years and 55.6% were female. The inspired tidal volume was 594± 112ml in the intervention group and 487± 51ml in the control group (p=0.024) and the expired tidal volume was 598± 105ml in the intervention group and 490± 58ml in the control group (p=0.02). The mean pre-maneuver static pulmonary compliance in the intervention group was 41.6± 12.1 ml/cmH2O and post maneuver it was 47.4± 16.6 ml/cmH2O (p=0.03). There was no significant between groups difference in the following variables: oxygen peripheral saturation, oxygen arterial pressure, extubation time and radiological changes. CONCLUSION: The results show that the manual hyperinflation associated with positive end expiratory pressure maneuver trends to promote increased lung volumes and static compliance, however these findings require further confirmation.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):47-52
DOI 10.1590/S0103-507X2010000100009
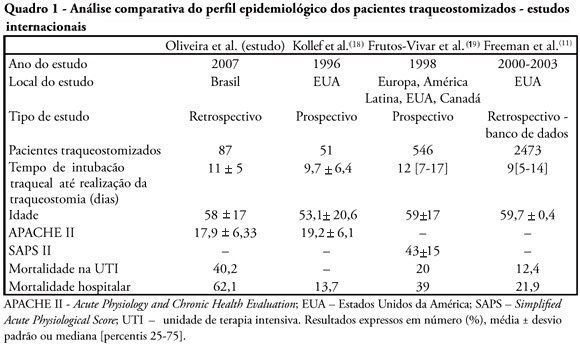
OBJECTIVES: Tracheostomy is a common procedure in intensive care unit to promote mechanical ventilation weaning. Despite tracheostomy is increasingly used there is no agreement of actual clinical practice of tracheostomy in different groups of patients in our environment. Objective of this study was to evaluate the epidemiological profile and outcomes of patients with tracheostomy at a clinical-surgical intensive care unit and compare this profile with the current literature. METHODS: Retrospective descriptive study through review of medical records and quality control database of "QuaTI" (Qualidade em Terapia Intensiva) of 87 patients with tracheostomy at Santa Casa de Belo Horizonte intensive care unit in 2007. We studied variables related to evolution aspects. RESULTS: The clinical and epidemiological analysis of the 87 patients showed: mean age 58 ± 17 years, mean Acute Physiology and Chronic Health Evaluation - APACHE II 18 ± 6, mean time of orotracheal intubation before tracheostomy of 11.17 ± 4.78 days. Intensive care unit mortality was 40.2% (35/87 patients), ward mortality was 36.5% (19/52) and overall hospital mortality 62.1% (54/87). Mean age of patients who died at intensive care unit (65 + 17 years) was greater than who were discharged to ward (53 ± 16 years) p = 0.003. Mean age of who died in hospital (intensive care unit and ward) (62 ± 17 years) was also higher than survivors (52 ± 16 years) p = 0.008. Old age (> 65 years) was related to intensive care unit mortality (OR 2.874, CI 1.165 a 7.088 p = 0.020) and also related to the overall hospital mortality (OR 3.202, CI 1.188 a 8.628 p = 0.019). There were not others variables related to mortality in this sample. CONCLUSIONS: The epidemiological profile of patients who underwent tracheotomy in the intensive care unit showed high mortality rate when compared to international series. Senility was related to worse outcome in these patients. Other issues were not related mortality in this group.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):349-352
DOI 10.1590/S0103-507X2009000400003
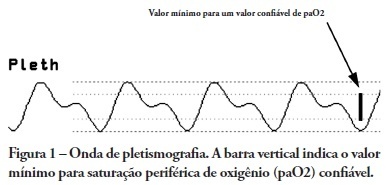
OBJECTIVES: Arterial pulse pressure respiratory variation is a good predictor of fluid response in ventilated patients. Recently, it was shown that respiratory variation in arterial pulse pressure correlates with variation in pulse oximetry plethysmographic waveform amplitude. We wanted to evaluate the correlation between respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude, and to determine whether this correlation was influenced by norepinephrine administration. METHODS: Prospective study of sixty patients with normal sinus rhythm on mechanical ventilation, profoundly sedated and with stable hemodynamics. Oxygenation index and invasive arterial pressure were monitored. Respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude were recorded simultaneously in a beat-to-beat evaluation, and were compared using the Pearson coefficient of agreement and linear regression. RESULTS: Thirty patients (50%) required norepinephrine. There was a significant correlation (K = 0.66; p < 0.001) between respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude. Area under the ROC curve was 0.88 (range, 0.79 - 0.97), with a best cutoff value of 14% to predict a respiratory variation in arterial pulse pressure of 13. The use of norepinephrine did not influence the correlation (K = 0.63, p = 0.001, respectively). CONCLUSIONS: Respiratory variation in arterial pulse pressure above 13% can be accurately predicted by a respiratory variation in pulse oximetry plethysmographic waveform amplitude of 14%. The use of norepinephrine does not alter this relationship.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):453-460
DOI 10.1590/S0103-507X2009000400017
Recent changes were introduced in acute hypoxemic respiratory failure children ventilation methods. There are evidences that less aggressive ventilation strategies can improve severe pulmonary injury survival. Experimental trials evidenced a relationship between inappropriate ventilatory measures and delayed acute pulmonary injury improvement, or even worsening. From this, a protective ventilatory measure arises in combination with alveolar recruitment maneuver. This association is believed in clinical practice to determine importantly reduced morbidity and mortality as well as reduced mechanic ventilation-induced injuries. It is indicated for acute lung injury patients, generally from pneumonia or sepsis, with severe hypoxemia. Its main contraindications are homodynamic instability, pneumothorax and intracranial hypertension. Experimental trials showed beneficial maneuver effects on both oxygenation and alveolar collapse. Adult studies showed improved pulmonary function with hypoxemia reversion. In children, the maneuver lead to significant inspired oxygen fraction and alveolar collapse reductions, less oxygen dependency, improved pulmonary complacency, and reduced bronchopulmonary dysplasia. However, studies in children are limited. Additional investigation is warranted on this matter, and its clinical application evidence. A literature review was conducted based on textbooks and MEDLINE, Pubmed, Cochrane library, SciELO, and Ovid databases, from 1998 to 2009, both in Portuguese and English. Publications on alveolar recruitment maneuver both in adults and children, review articles, experimental and clinical trials were included using the key words: protective ventilatory strategy, alveolar recruitment maneuver, pediatrics and mechanic ventilation.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):262-268
DOI 10.1590/S0103-507X2009000300005
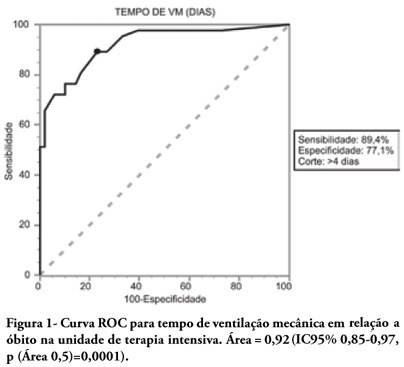
OBJECTIVES: To describe the population of aged as compared to young patients under mechanical ventilation and to analyze the mortality risk factors of this group in an intensive care unit. METHODS: This was a prospective observational trial in patients over 18 years of age, admitted in an intensive care unit and under mechanical ventilation, during one year. Patients were divided into two groups according to age: Group 1 - patients over 65 years old; and Group 2, 65 years old or younger. RESULTS: eighty one mechanic ventilation patients were included, 62 aged and 18 younger, mean ages from aged was 76 years, while in the younger it was 56 years. As compared to the control, aged patients had longer mechanic ventilation time , higher intensive care unit and hospital mortality: 63.1% versus 26.3% and 74.2% versus 47.4% (P<0.05), respectively. In addition, the aged under mechanic ventilation had increased desintubation failures, difficult ventilatory weaning and deaths directly related to respiratory dysfunction. The mechanic ventilation time was an independent risk factor for death in the intensive care unit in aged patients (OR= 2.7, p=0.02). The area under the ROC curve of mechanic ventilation about intensive care unit death was 0.92 (95% CI 0.85-0.97, p (area 0.5)=0.0001), cutoff point of 4 days, sensitivity 89.4% and specificity 77.1%. CONCLUSIONS: Mechanic ventilation patients over 65years of age have a worse prognosis than the younger, and the longer the mechanic ventilation time, the higher will be intensive care mortality.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):231-236
DOI 10.1590/S0103-507X2009000300001
OBJECTIVE: This study aimed to analyze outcome, clinical and epidemiological characteristics and severity factors in adult patients admitted with a diagnosis of infection by virus A (H1N1) to public and private intensive care units, in Paraná, Brazil. METHODS: Cohort study of medical charts of patients older than 12 years admitted to 11 intensive care units in 6 cities in the state of Parana, Brazil, during a period of 45 days, with diagnosis of swine influenza. The diagnosis of infection with A (H1N1) was made by real time polymerase chain reaction (RT-PCR) of nasopharyngeal secretion, or strong clinical suspicion when other causes had been ruled out (even with negative RT-PCR). Descriptive statistics were performed, analysis by the Chi square test was used to compare percentages and the Student's t test for continuous variables with univariate analysis, assuming a significance level of p <0.05. RESULTS: There were 63 adult patients admitted with a diagnosis of H1N1, 37 (58.7%) being RT-PCR positive. Most patients were young adults (65% under 40 years of age) with no gender predominance and high incidence of obesity (27.0% with Body Mass Index > 30). Mean of the Acute Physiologic Chronic Health Evaluation II (APACHE II) score was 15.0 + 8.1. Mortality in the intensive care unit was 39.7%. The main factors associated with mortality were: positive RT-PCR, low levels of initial PaO2/FiO2, high initial levels of urea and lactate dehydrogenase, required level of positive end expiratory pressure, need for the prone position and vasopressors. CONCLUSIONS: Adult patients with A (H1N1) virus infection admitted to intensive care units had a high risk of death, particularly due to respiratory impairment. Positive RT-PCR, urea and lactic dehydrogenase, low initial PaO2/FiO2 and high levels of PEEP were correlated with higher mortality.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):155-161
DOI 10.1590/S0103-507X2009000200007
OBJECTIVES: Patients unable to perform breathing functions may be submitted to invasive mechanical ventilation. Chest physiotherapy acts directly on the treatment of these patients for the purpose of improving their lung function. The objective of this study was to evaluate the effects of manual rib-cage compression versus the positive end expiratory pressure-zero end expiratory pressure (PEEP-ZEEP) maneuver, on compliance of the respiratory system and oxygenation in patients under invasive mechanical ventilation. METHODS: A double centric, prospective, randomized and crossover study, with patients under invasive mechanical ventilation, in controlled mode for more than 48 hours was carried out. The protocols of chest physiothe-rapy were randomly applied at an interval of 24 hours. Data of respiratory system compliance and oxygenation were collected before application of the protocols and 30 minutes after. RESULTS: Twelve patients completed the study. Intragroup analysis, for both techniques showed a statistically significant difference in tidal volume (p=0.002), static compliance (p=0.002) and dynamic compliance (p=0.002). In relation to oxygenation, in the group of manual rib-cage compression, peripheral oxygen saturation increased with a significant difference (p=0.011). CONCLUSIONS: Manual rib-cage compression and PEEP-ZEEP maneuver have positive clinical effects. In relation to oxygenation we found a favorable behavior of peripheral oxygen saturation in the group of manual rib-cage compression.