Abstract
Rev Bras Ter Intensiva. 2017;29(1):87-95
DOI 10.5935/0103-507X.20170013
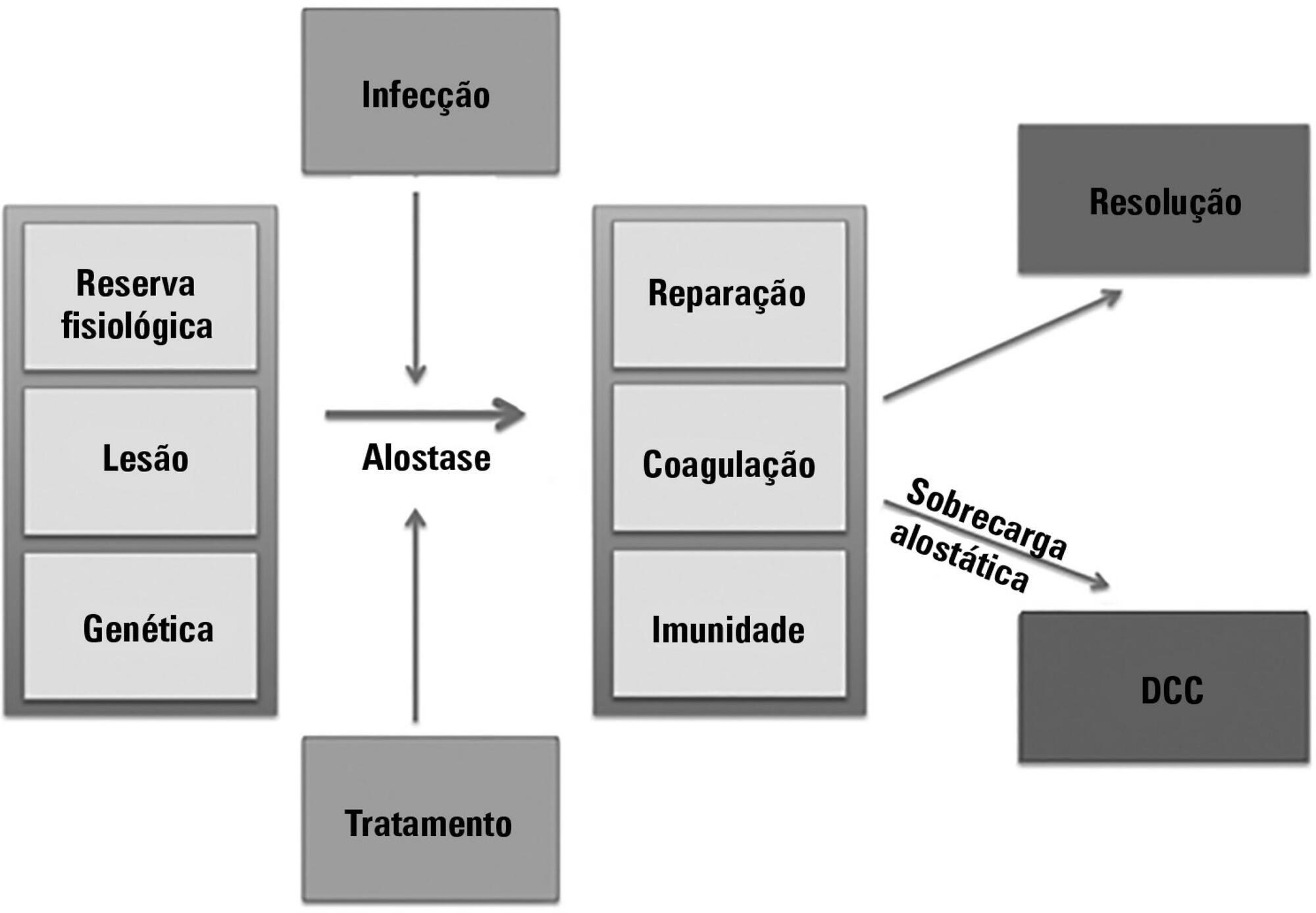
The technological advancements that allow support for organ dysfunction have led to an increase in survival rates for the most critically ill patients. Some of these patients survive the initial acute critical condition but continue to suffer from organ dysfunction and remain in an inflammatory state for long periods of time. This group of critically ill patients has been described since the 1980s and has had different diagnostic criteria over the years. These patients are known to have lengthy hospital stays, undergo significant alterations in muscle and bone metabolism, show immunodeficiency, consume substantial health resources, have reduced functional and cognitive capacity after discharge, create a sizable workload for caregivers, and present high long-term mortality rates. The aim of this review is to report on the most current evidence in terms of the definition, pathophysiology, clinical manifestations, treatment, and prognosis of persistent critical illness.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):180-187
DOI 10.5935/0103-507X.20170028
To analyze patients after cardiac surgery that needed endotracheal reintubation and identify factors associated with death and its relation with the severity scores.
Retrospective analysis of information of 1,640 patients in the postoperative period of cardiac surgery between 2007 and 2015.
The reintubation rate was 7.26%. Of those who were reintubated, 36 (30.3%) underwent coronary artery bypass surgery, 27 (22.7%) underwent valve replacement, 25 (21.0%) underwent correction of an aneurysm, and 8 (6.7%) underwent a heart transplant. Among those with comorbidities, 54 (51.9%) were hypertensive, 22 (21.2%) were diabetic, and 10 (9.6%) had lung diseases. Among those who had complications, 61 (52.6%) had pneumonia, 50 (42.4%) developed renal failure, and 49 (51.0%) had a moderate form of the transient disturbance of gas exchange. Noninvasive ventilation was performed in 53 (44.5%) patients. The death rate was 40.3%, and mortality was higher in the group that did not receive noninvasive ventilation before reintubation (53.5%). Within the reintubated patients who died, the SOFA and APACHE II values were 7.9 ± 3.0 and 16.9 ± 4.5, respectively. Most of the reintubated patients (47.5%) belonged to the high-risk group, EuroSCORE (> 6 points).
The reintubation rate was high, and it was related to worse SOFA, APACHE II and EuroSCORE scores. Mortality was higher in the group that did not receive noninvasive ventilation before reintubation.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):114-119
DOI 10.5935/0103-507X.20160025
To evaluate the variation in mobility during hospitalization in an intensive care unit and its association with hospital mortality.
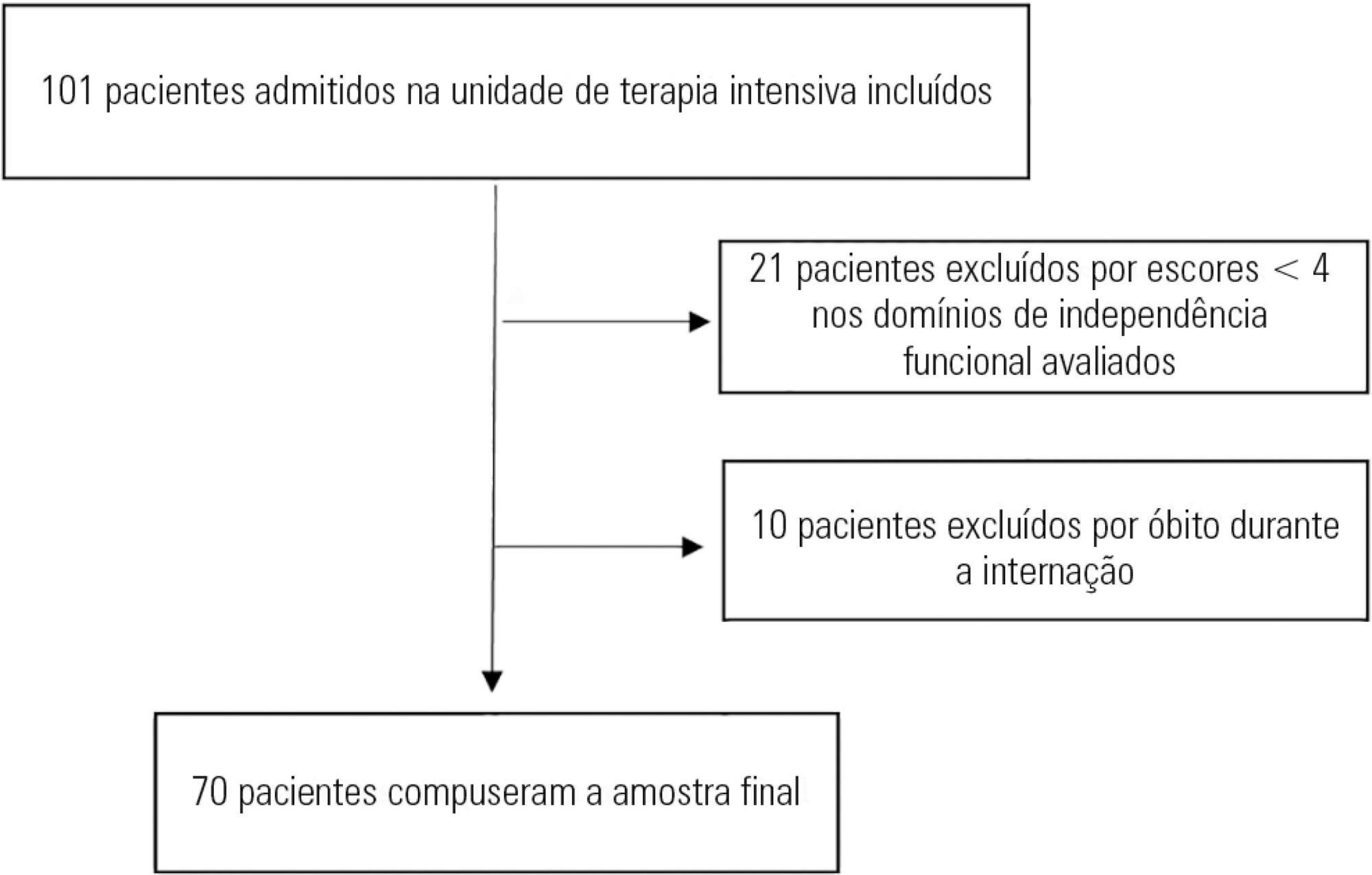
This prospective study was conducted in an intensive care unit. The inclusion criteria included patients admitted with an independence score of ≥ 4 for both bed-chair transfer and locomotion, with the score based on the Functional Independence Measure. Patients with cardiac arrest and/or those who died during hospitalization were excluded. To measure the loss of mobility, the value obtained at discharge was calculated and subtracted from the value obtained on admission, which was then divided by the admission score and recorded as a percentage.
The comparison of these two variables indicated that the loss of mobility during hospitalization was 14.3% (p < 0.001). Loss of mobility was greater in patients hospitalized for more than 48 hours in the intensive care unit (p < 0.02) and in patients who used vasopressor drugs (p = 0.041). However, the comparison between subjects aged 60 years or older and those younger than 60 years indicated no significant differences in the loss of mobility (p = 0.332), reason for hospitalization (p = 0.265), SAPS 3 score (p = 0.224), use of mechanical ventilation (p = 0.117), or hospital mortality (p = 0.063).
There was loss of mobility during hospitalization in the intensive care unit. This loss was greater in patients who were hospitalized for more than 48 hours and in those who used vasopressors; however, the causal and prognostic factors associated with this decline need to be elucidated.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):26-35
DOI 10.5935/0103-507X.20150006
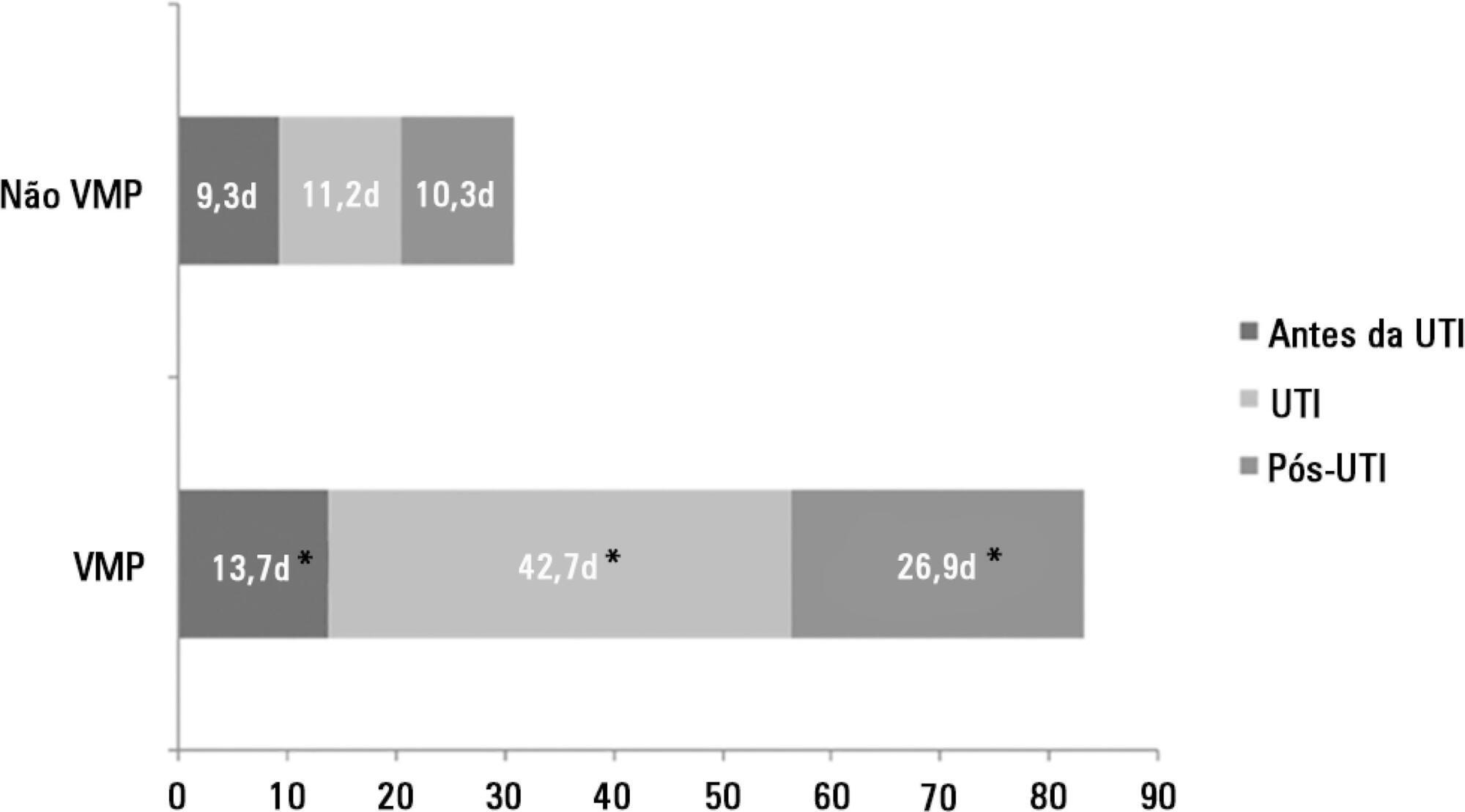
The number of patients who require prolonged mechanical ventilation increased during the last decade, which generated a large population of chronically ill patients. This study established the incidence of prolonged mechanical ventilation in four intensive care units and reported different characteristics, hospital outcomes, and the impact of costs and services of prolonged mechanical ventilation patients (mechanical ventilation dependency ≥ 21 days) compared with non-prolonged mechanical ventilation patients (mechanical ventilation dependency < 21 days).
This study was a multicenter cohort study of all patients who were admitted to four intensive care units. The main outcome measures were length of stay in the intensive care unit, hospital, complications during intensive care unit stay, and intensive care unit and hospital mortality.
There were 5,287 admissions to the intensive care units during study period. Some of these patients (41.5%) needed ventilatory support (n = 2,197), and 218 of the patients met criteria for prolonged mechanical ventilation (9.9%). Some complications developed during intensive care unit stay, such as muscle weakness, pressure ulcers, bacterial nosocomial sepsis, candidemia, pulmonary embolism, and hyperactive delirium, were associated with a significantly higher risk of prolonged mechanical ventilation. Prolonged mechanical ventilation patients had a significant increase in intensive care unit mortality (absolute difference = 14.2%, p < 0.001) and hospital mortality (absolute difference = 19.1%, p < 0.001). The prolonged mechanical ventilation group spent more days in the hospital after intensive care unit discharge (26.9 ± 29.3 versus 10.3 ± 20.4 days, p < 0.001) with higher costs.
The classification of chronically critically ill patients according to the definition of prolonged mechanical ventilation adopted by our study (mechanical ventilation dependency ≥ 21 days) identified patients with a high risk for complications during intensive care unit stay, longer intensive care unit and hospital stays, high death rates, and higher costs.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):105-112
DOI 10.5935/0103-507X.20150020
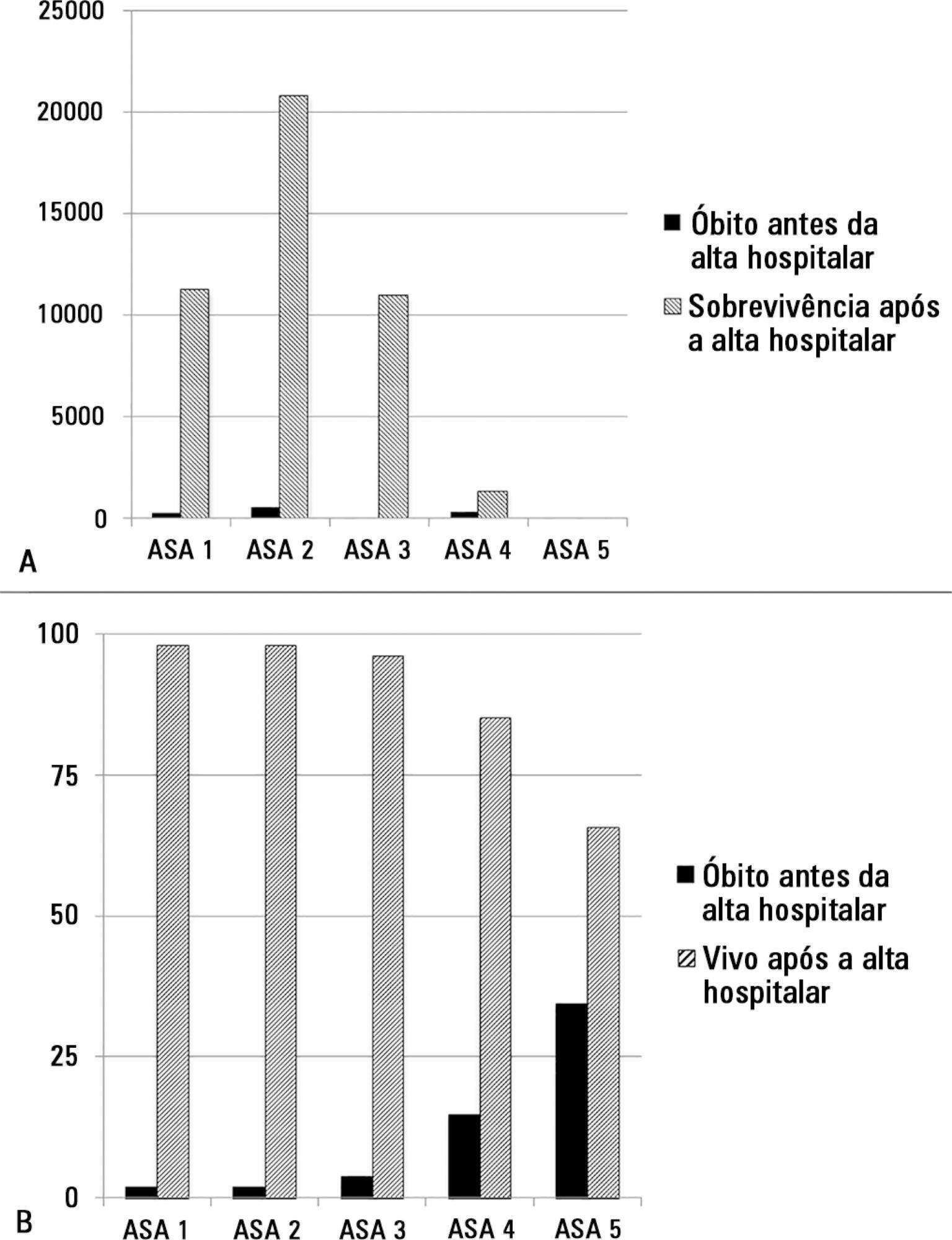
The European Surgical Outcomes Study described mortality following in-patient surgery. Several factors were identified that were able to predict poor outcomes in a multivariate analysis. These included age, procedure urgency, severity and type and the American Association of Anaesthesia score. This study describes in greater detail the relationship between the American Association of Anaesthesia score and postoperative mortality.
Patients in this 7-day cohort study were enrolled in April 2011. Consecutive patients aged 16 years and older undergoing inpatient non-cardiac surgery with a recorded American Association of Anaesthesia score in 498 hospitals across 28 European nations were included and followed up for a maximum of 60 days. The primary endpoint was in-hospital mortality. Decision tree analysis with the CHAID (SPSS) system was used to delineate nodes associated with mortality.
The study enrolled 46,539 patients. Due to missing values, 873 patients were excluded, resulting in the analysis of 45,666 patients. Increasing American Association of Anaesthesia scores were associated with increased admission rates to intensive care and higher mortality rates. Despite a progressive relationship with mortality, discrimination was poor, with an area under the ROC curve of 0.658 (95% CI 0.642 - 0.6775). Using regression trees (CHAID), we identified four discrete American Association of Anaesthesia nodes associated with mortality, with American Association of Anaesthesia 1 and American Association of Anaesthesia 2 compressed into the same node.
The American Association of Anaesthesia score can be used to determine higher risk groups of surgical patients, but clinicians cannot use the score to discriminate between grades 1 and 2. Overall, the discriminatory power of the model was less than acceptable for widespread use.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):44-50
DOI 10.5935/0103-507X.20140007
To assess the discrimination and calibration of the Pediatric Index of Mortality 2 in patients admitted to a pediatric intensive care unit.
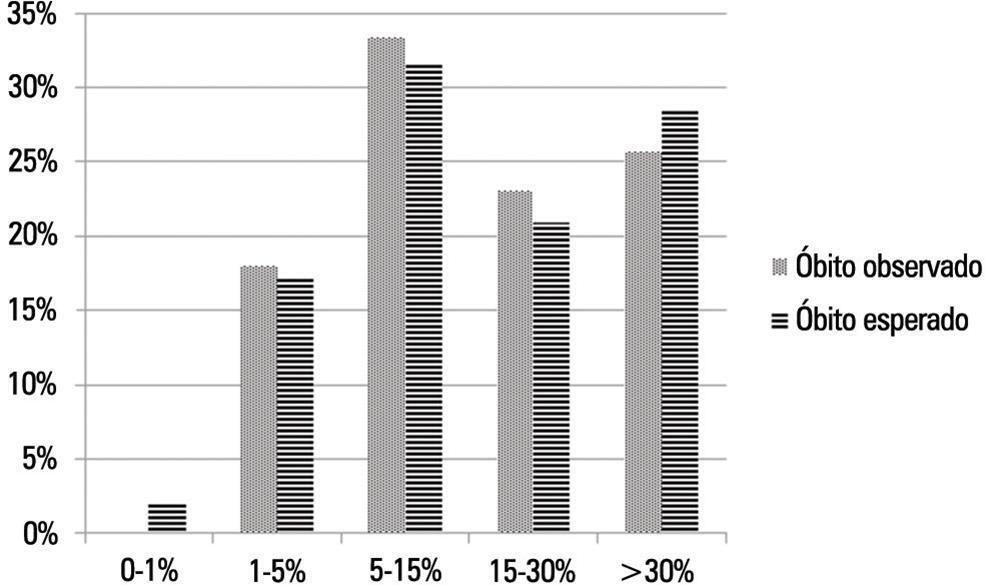
The study was conducted with a contemporary cohort from November 2005 to November 2006. Patients aged 29 days to 18 years were included in the study. Patients who died within 12 hours of admission and cases of readmission were excluded from the study. The performance of the Pediatric Index of Mortality 2 was assessed by means of the Hosmer-Lemeshow goodness-of-fit test, the standardized mortality ratio and the area under receiver operating characteristic (ROC) curve with 95% confidence interval. The significance level was established as 5%.
A total of 276 admissions to the pediatric intensive care unit were included in the analysis. The mortality rate was 14.13%, and the efficiency of admission 0.88%. The median age of the sample was 42.22 months, and most participants were male (60.1%). Most admissions were referrals from the emergency department. The mean duration of stay in pediatric intensive care unit was 6.43±5.23 days. Approximately 72.46% of admissions were for clinical reasons and exhibited an association with the outcome death (odds ratio: 2.9; 95%CI: 1.09-7.74; p=0.017). Calibration of the Pediatric Index of Mortality 2 with the chi-square statistic was 12.2686 (p=0.1396) in the Hosmer-Lemeshow goodness-of-fit test, and the standardized mortality ratio was 1.0. The area under the ROC curve assessing model discrimination was 0.778.
Pediatric Index of Mortality 2 exhibited satisfactory performance.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):130-136
DOI 10.5935/0103-507X.20130024
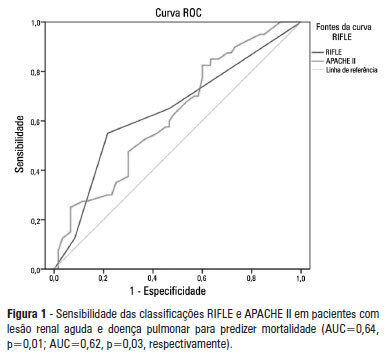
OBJECTIVE: To examine the factors associated with acute kidney injury and outcome in patients with lung disease. METHODS: A prospective study was conducted with 100 consecutive patients admitted to a respiratory intensive care unit in Fortaleza (CE), Brazil. The risk factors for acute kidney injury and mortality were investigated in a group of patients with lung diseases. RESULTS: The mean age of the study population was 57 years, and 50% were male. The incidence of acute kidney injury was higher in patients with PaO2/FiO2<200 mmHg (54% versus 23.7%; p=0.02). Death was observed in 40 cases and the rate of mortality of the acute kidney injury group was higher (62.8% versus 27.6%; p=0.01). The independent factor that was found to be associated with acute kidney injury was PaO2/FiO2<200 mmHg (p=0.01), and the independent risk factors for death were PEEP at admission (OR: 3.6; 95%CI: 1.3-9.6; p=0.009) and need for hemodialysis (OR: 7.9; 95%CI: 2.2-28.3; p=0.001). CONCLUSION: There was a higher mortality rate in the acute kidney injury group. Increased mortality was associated with mechanical ventilation, high PEEP, urea and need for dialysis. Further studies must be performed to better establish the relationship between kidney and lung injury and its impact on patient outcome.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):49-55
DOI 10.1590/S0103-507X2013000100010
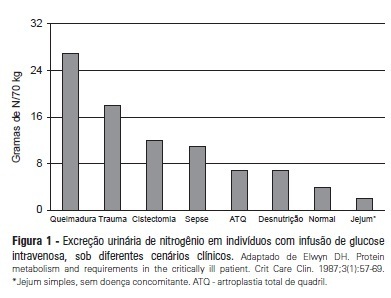
Recent evidence suggests that a negative protein balance secondary to severe disease is associated with increased morbidity. A loss of total body protein is inevitable in this scenario, even with an aggressive nutritional approach, primarily due to the catabolism of skeletal muscle fibers. The ubiquitin-proteasome system is the primary metabolic and biochemical mechanism involved in this process; paradoxically, this system consumes adenosine triphosphate as its energy source. It is possible that a neutral protein balance in these clinical situations is important for improving outcomes and achieving the caloric goals estimated or measured by indirect calorimetry. Recent studies have suggested that the use of higher protein concentrations in nutritional therapy for critically ill patients may help to reduce mortality. The purpose of this study was to review some of the nutrition therapy principles related to protein metabolism, evaluate the main assertions of the guidelines of specialty societies and review the recent studies that address these issues using critical insights from the authors' clinical experience.