Abstract
Rev Bras Ter Intensiva. 2017;29(2):163-170
DOI 10.5935/0103-507X.20170026
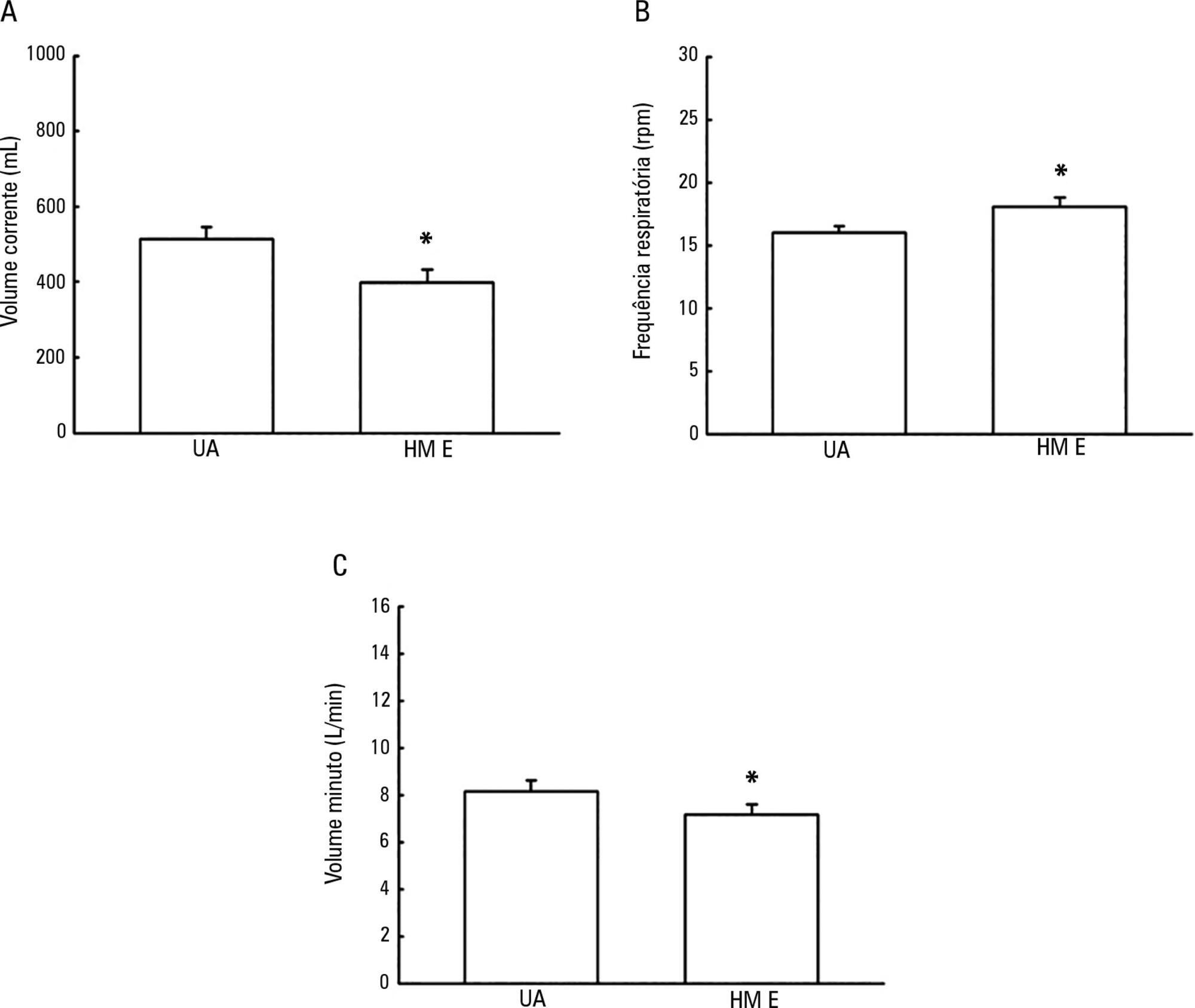
To evaluate the possible changes in tidal volume, minute volume and respiratory rate caused by the use of a heat and moisture exchanger in patients receiving pressure support mechanical ventilation and to quantify the variation in pressure support required to compensate for the effect caused by the heat and moisture exchanger.
Patients under invasive mechanical ventilation in pressure support mode were evaluated using heated humidifiers and heat and moisture exchangers. If the volume found using the heat and moisture exchangers was lower than that found with the heated humidifier, an increase in pressure support was initiated during the use of the heat and moisture exchanger until a pressure support value was obtained that enabled the patient to generate a value close to the initial tidal volume obtained with the heated humidifier. The analysis was performed by means of the paired t test, and incremental values were expressed as percentages of increase required.
A total of 26 patients were evaluated. The use of heat and moisture exchangers increased the respiratory rate and reduced the tidal and minute volumes compared with the use of the heated humidifier. Patients required a 38.13% increase in pressure support to maintain previous volumes when using the heat and moisture exchanger.
The heat and moisture exchanger changed the tidal and minute volumes and respiratory rate parameters. Pressure support was increased to compensate for these changes.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):364-372
DOI 10.5935/0103-507X.20170054
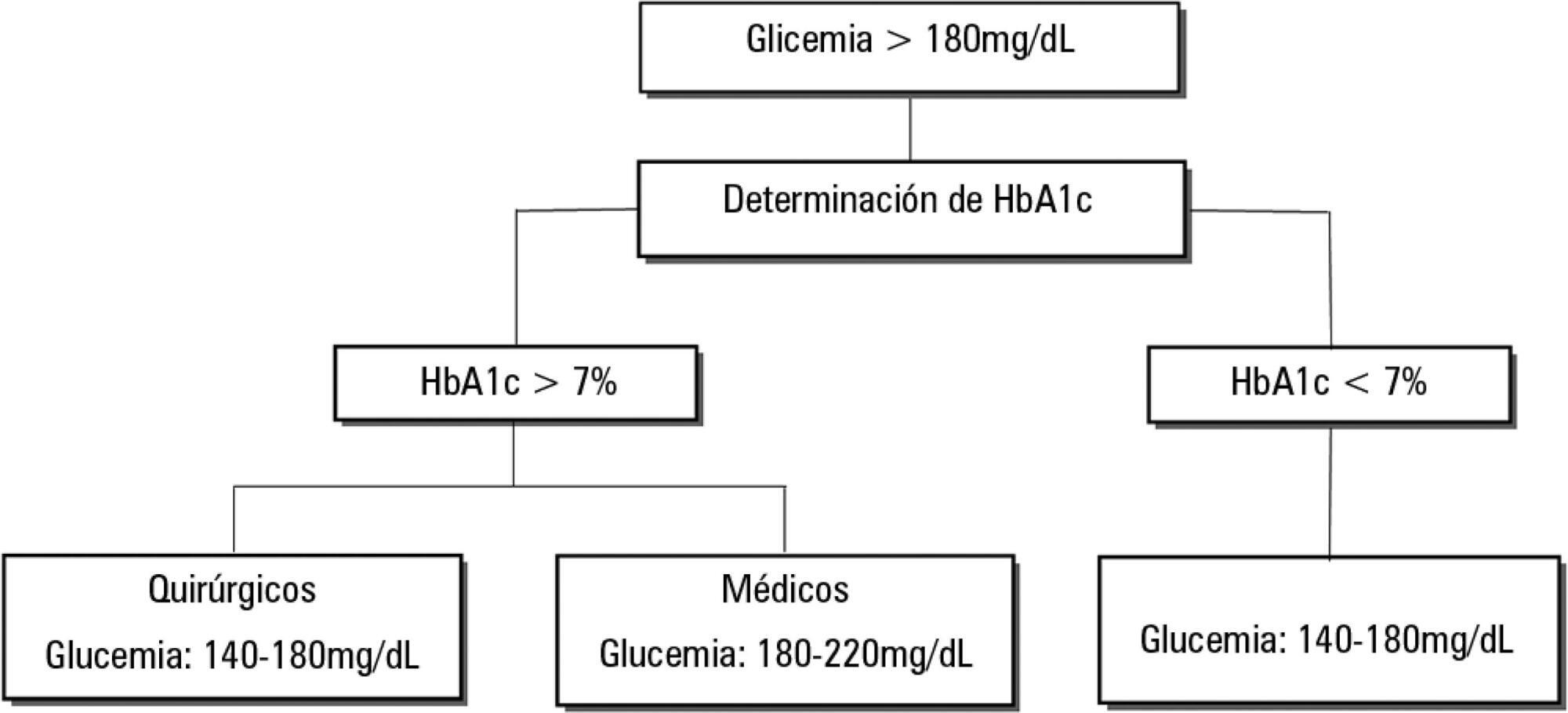
Dysglycemia in critically ill patients (hyperglycemia, hypoglycemia, glycemic variability and time in range) is a biomarker of disease severity and is associated with higher mortality. However, this impact appears to be weakened in patients with previous diabetes mellitus, particularly in those with poor premorbid glycemic control; this phenomenon has been called "diabetes paradox". This phenomenon determines that glycated hemoglobin (HbA1c) values should be considered in choosing glycemic control protocols on admission to an intensive care unit and that patients' target blood glucose ranges should be adjusted according to their HbA1c values. Therefore, HbA1c emerges as a simple tool that allows information that has therapeutic utility and prognostic value to be obtained in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):436-443
DOI 10.5935/0103-507X.20170070
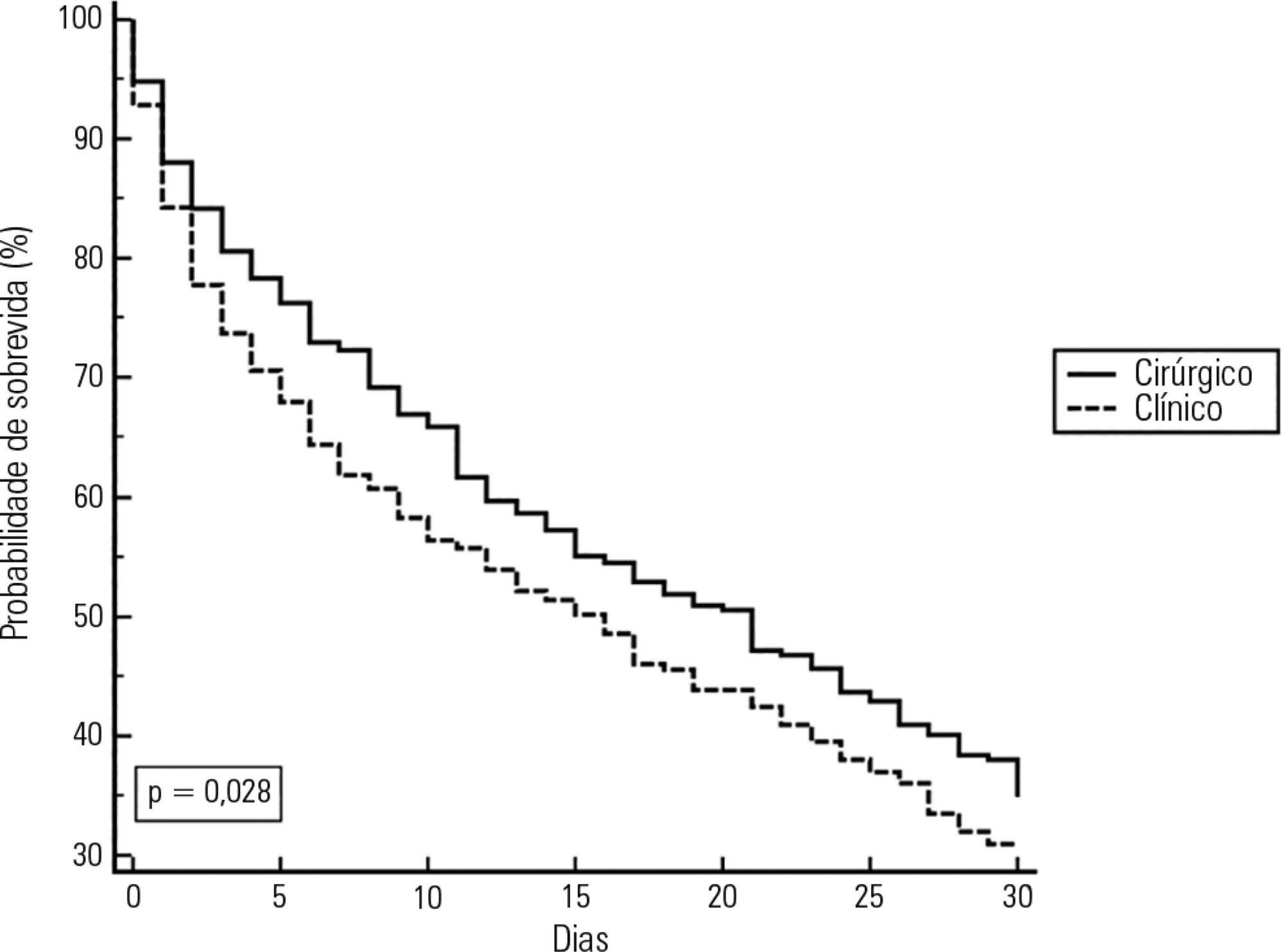
To define the frequency of cytomegalovirus disease among kidney transplant patients in an intensive care unit in which this complication was suspected and to identify predisposing factors and their possible impact on clinical outcome.
Retrospective observational study in which kidney transplant patients over the age of 18 years were hospitalized for any reason in an intensive care unit with at least one collection of samples to test for the presence of antigenemia or cytomegalovirus via polymerase chain reaction during hospitalization. Cytomegalovirus disease was defined as positive antigenemia or polymerase chain reaction above 500 copies/mL in the presence of symptoms and in the appropriate clinical setting, as judged by the attending physician.
A total of 99 patients were included (age: 53.4 ± 12.8 years, 71.6% male). Cytomegalovirus disease was diagnosed in 39 patients (39.4%). Respiratory symptoms (51%), non-specific clinical worsening (20%) or gastrointestinal symptoms (14%) were the main reasons for exam collection. Transplant time was lower in those with cytomegalovirus disease than in those without this diagnosis (6.5 months and 31.2 months, p = 0.001), along with pulse therapy in the last 6 months (41% and 16.9%, p = 0.008) and previous use of thymoglobulin in the last year (35.9% and 6.8%, p < 0.001). In the logistic regression model, only the transplant time and the use of thymoglobulin were associated with a higher frequency of cytomegalovirus. There was no difference in clinical evolution between patients with and without cytomegalovirus disease.
In kidney transplant patients suspected of cytomegalovirus disease, the prevalence was high. Transplant time less than 6 months, and the use of thymoglobulin in the last year should increase the intensivist's suspicion for this complication.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):476-480
DOI 10.5935/0103-507X.20170071
To evaluate the intra- and inter-reliability and the ease of measuring the quadriceps muscle thickness using bedside ultrasound.
This is a prospective, observational study. The assessment of quadriceps muscle thickness was performed at two reference points and was quantified using portable B-mode ultrasound in two healthy volunteers. For standardization of measurements and validation of image collections, the team was trained through theoretical and practical classes, with a 6-hour workload.
A total of 112 images were examined by the coach and compared with the trainees. Pearson's correlation analysis found an excellent relationship between the coach and all trainees (R2 > 0.90). The best association was between the coach and the dietitians (R2: 0.99; p < 0.001), and the worst association was between the coach and the medical trainees (R2: 0.92; p < 0.001). In the Bland-Altman comparison, the highest error rate found between coach and trainees was 5.12% (95% confidence interval [CI] 3.64-12.37), and the lowest was 1.01% (95%CI 0.72 - 2.58); the highest bias of the values described was -0.12 ± 0.19, and the lowest was -0.01 ± 0.04.
The data analyzed showed a good correlation between the measurements made by the coach and trainees, indicating that ultrasound of the quadriceps muscle is a viable and easily applicable tool.

Abstract
Rev Bras Ter Intensiva. 2016;28(3):278-284
DOI 10.5935/0103-507X.20160045
To evaluate the implementation of a multidisciplinary rapid response team led by an intensive care physician at a university hospital.
This retrospective cohort study analyzed assessment forms that were completed during the assessments made by the rapid response team of a university hospital between March 2009 and February 2014.
Data were collected from 1,628 assessments performed by the rapid response team for 1,024 patients and included 1,423 code yellow events and 205 code blue events. The number of assessments was higher in the first year of operation of the rapid response team. The multivariate analysis indicated that age (OR 1.02; 95%CI 1.02 - 1.03; p < 0.001), being male (OR 1.48; 95%CI 1.09 - 2.01; p = 0.01), having more than one assessment (OR 3.31; 95%CI, 2.32 - 4.71; p < 0.001), hospitalization for clinical care (OR 1.77; 95%CI 1.29 - 2.42; p < 0.001), the request of admission to the intensive care unit after the code event (OR 4.75; 95%CI 3.43 - 6.59; p < 0.001), and admission to the intensive care unit before the code event (OR 2.13; 95%CI 1.41 - 3.21; p = 0.001) were risk factors for hospital mortality in patients who were seen for code yellow events.
The hospital mortality rates were higher than those found in previous studies. The number of assessments was higher in the first year of operation of the rapid response team. Moreover, hospital mortality was higher among patients admitted for clinical care.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):285-293
DOI 10.5935/0103-507X.20160043
To evaluate the knowledge and acceptance of the public and professionals working in intensive care units regarding organ donation after cardiac death.
The three hospitals with the most brain death notifications in Curitiba were selected, and two groups of respondents were established for application of the same questionnaire: the general public (i.e., visitors of patients in intensive care units) and health professionals working in the same intensive care unit. The questionnaire contained questions concerning demographics, intention to donate organs and knowledge of current legislation regarding brain death and donation after cardiac death.
In total, 543 questionnaires were collected, including 442 from family members and 101 from health professionals. There was a predominance of women and Catholics in both groups. More females intended to donate. Health professionals performed better in the knowledge comparison. The intention to donate organs was significantly higher in the health professionals group (p = 0.01). There was no significant difference in the intention to donate in terms of education level or income. There was a greater acceptance of donation after uncontrolled cardiac death among Catholics than among evangelicals (p < 0.001).
Most of the general population intended to donate, with greater intentions expressed by females. Education and income did not affect the decision. The type of transplant that used a donation after uncontrolled cardiac death was not well accepted in the study population, indicating the need for more clarification for its use in our setting.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):294-300
DOI 10.5935/0103-507X.20160042
To estimate the incidence of limitations to Advanced Life Support in critically ill patients admitted to an intensive care unit with integrated palliative care.
This retrospective cohort study included patients in the palliative care program of the intensive care unit of Hospital Paulistano over 18 years of age from May 1, 2011, to January 31, 2014. The limitations to Advanced Life Support that were analyzed included do-not-resuscitate orders, mechanical ventilation, dialysis and vasoactive drugs. Central tendency measures were calculated for quantitative variables. The chi-squared test was used to compare the characteristics of patients with or without limits to Advanced Life Support, and the Wilcoxon test was used to compare length of stay after Advanced Life Support. Confidence intervals reflecting p ≤ 0.05 were considered for statistical significance.
A total of 3,487 patients were admitted to the intensive care unit, of whom 342 were included in the palliative care program. It was observed that after entering the palliative care program, it took a median of 2 (1 - 4) days for death to occur in the intensive care unit and 4 (2 - 11) days for hospital death to occur. Many of the limitations to Advanced Life Support (42.7%) took place on the first day of hospitalization. Cardiopulmonary resuscitation (96.8%) and ventilatory support (73.6%) were the most adopted limitations.
The contribution of palliative care integrated into the intensive care unit was important for the practice of orthothanasia, i.e., the non-extension of the life of a critically ill patient by artificial means.