Abstract
Rev Bras Ter Intensiva. 2016;28(3):315-322
DOI 10.5935/0103-507X.20160044
To evaluate the prevalence of antibiotic de-escalation in patients diagnosed with severe sepsis or septic shock at a public academic tertiary hospital and to evaluate antibiotic adequacy and culture positivity.
The prevalence of antibiotic de-escalation, the adequacy of antibiotic treatment and the rates of culture positivity were analyzed in patients with severe sepsis and septic shock between April and December 2013 at an intensive care unit in a tertiary university hospital.
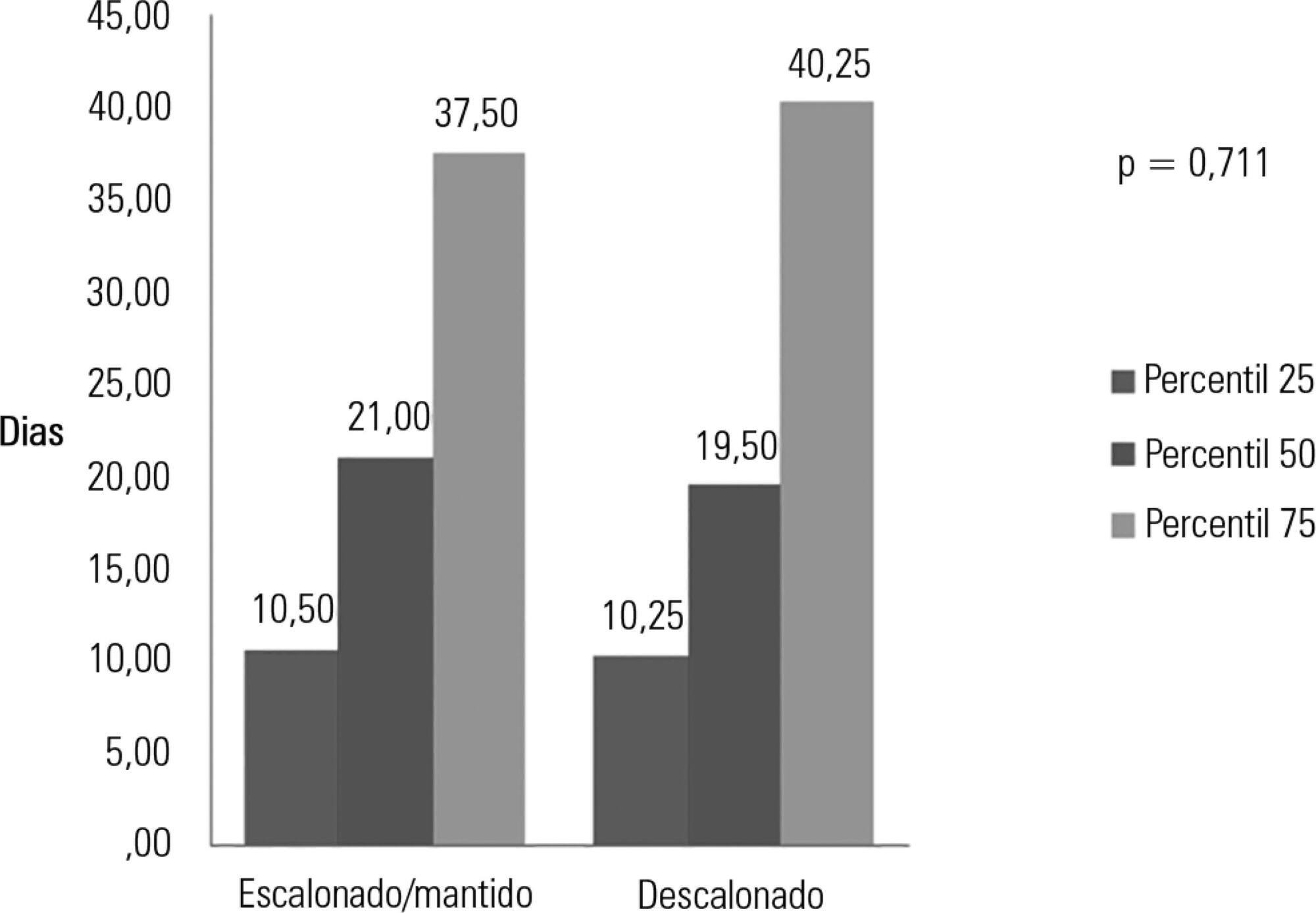
Among the 224 patients included in the study, de-escalation was appropriate in 66 patients (29.4%) but was implemented in 44 patients (19.6%). Among the patients who underwent de-escalation, half experienced narrowing of the antimicrobial spectrum. The mortality rate was 56.3%, with no differences between the patients with or without de-escalation (56.8% versus 56.1%; p = 0.999) nor in the length of hospital stay. Empirical antibiotic therapy was appropriate in 89% of cases. Microorganisms were isolated from total cultures in 30% of cases and from blood cultures in 26.3% of cases.
The adequacy rate of empirical antibiotic therapy was high, reflecting an active institutional policy of monitoring epidemiological profiles and institutional protocols on antimicrobial use. However, antibiotic de-escalation could have been implemented in a greater number of patients. De-escalation did not affect mortality rates.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):19-26
DOI 10.5935/0103-507X.20160009
Hypercapnia resulting from protective ventilation in acute respiratory distress syndrome triggers metabolic pH compensation, which is not entirely characterized. We aimed to describe this metabolic compensation.
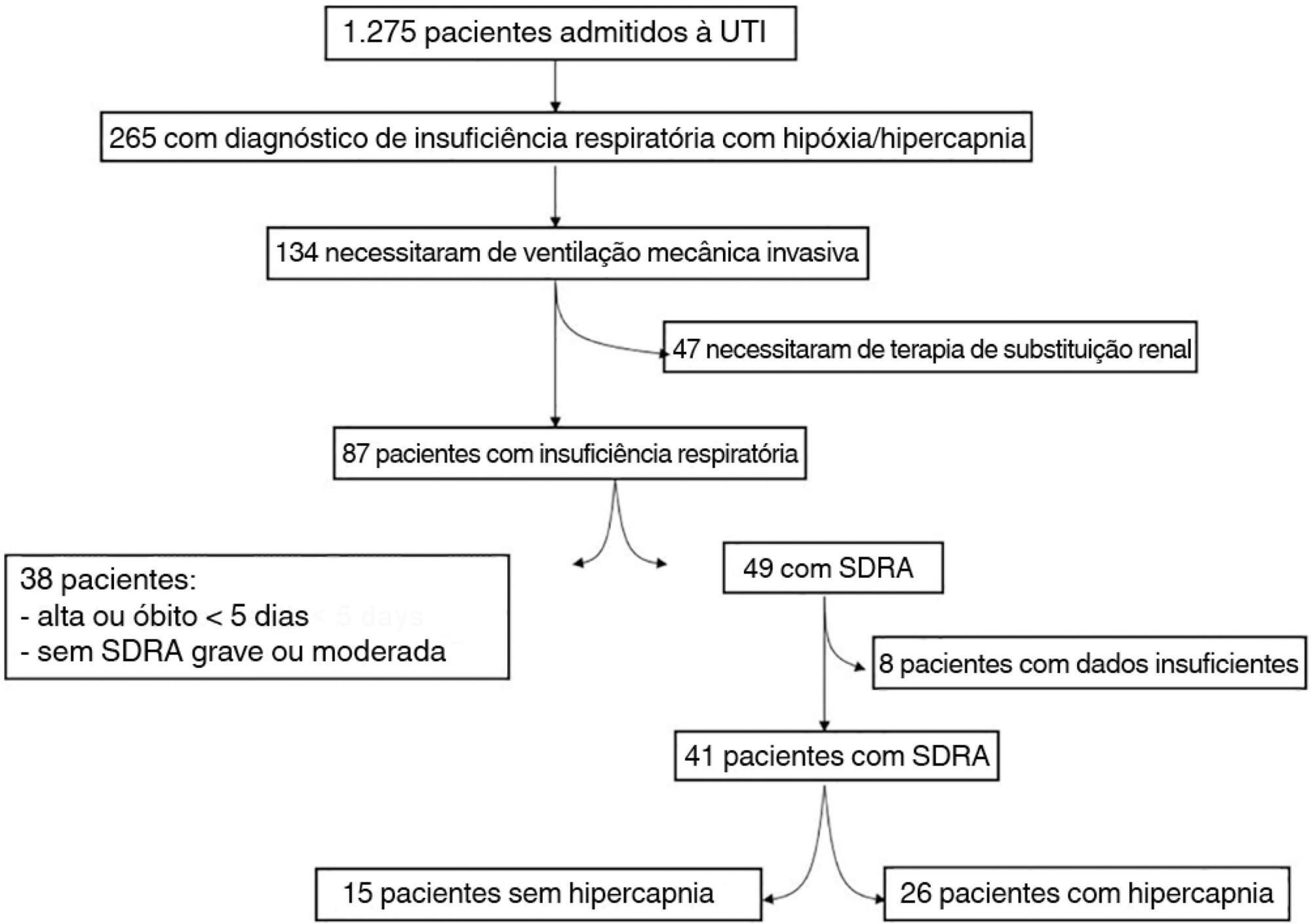
The data were retrieved from a prospective collected database. Variables from patients' admission and from hypercapnia installation until the third day after installation were gathered. Forty-one patients with acute respiratory distress syndrome were analyzed, including twenty-six with persistent hypercapnia (PaCO2 > 50mmHg > 24 hours) and 15 non-hypercapnic (control group). An acid-base quantitative physicochemical approach was used for the analysis.
The mean ages in the hypercapnic and control groups were 48 ± 18 years and 44 ± 14 years, respectively. After the induction of hypercapnia, pH markedly decreased and gradually improved in the ensuing 72 hours, consistent with increases in the standard base excess. The metabolic acid-base adaptation occurred because of decreases in the serum lactate and strong ion gap and increases in the inorganic apparent strong ion difference. Furthermore, the elevation in the inorganic apparent strong ion difference occurred due to slight increases in serum sodium, magnesium, potassium and calcium. Serum chloride did not decrease for up to 72 hours after the initiation of hypercapnia.
In this explanatory study, the results indicate that metabolic acid-base adaptation, which is triggered by acute persistent hypercapnia in patients with acute respiratory distress syndrome, is complex. Furthermore, further rapid increases in the standard base excess of hypercapnic patients involve decreases in serum lactate and unmeasured anions and increases in the inorganic apparent strong ion difference by means of slight increases in serum sodium, magnesium, calcium, and potassium. Serum chloride is not reduced.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):27-32
DOI 10.5935/0103-507X.20160010
To determine the efficacy of lung hyperinflation maneuvers via a mechanical ventilator compared to isolated tracheal aspiration for removing secretions, normalizing hemodynamics and improving lung mechanics in patients on mechanical ventilation.
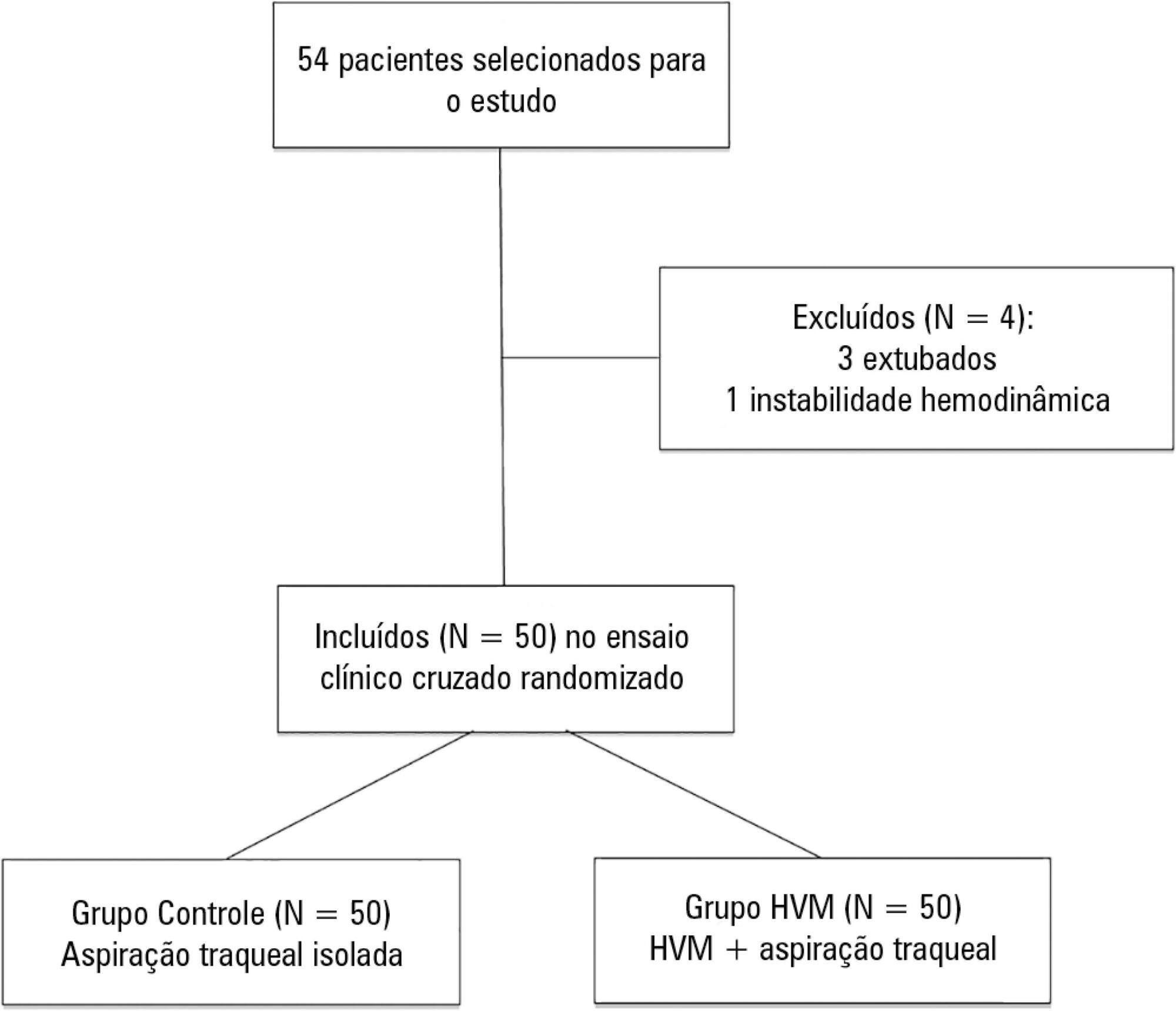
This was a randomized crossover clinical trial including patients admitted to the intensive care unit and on mechanical ventilation for more than 48 hours. Patients were randomized to receive either isolated tracheal aspiration (Control Group) or lung hyperinflation by mechanical ventilator (MVH Group). Hemodynamic and mechanical respiratory parameters were measured along with the amount of aspirated secretions.
A total of 50 patients were included. The mean age of the patients was 44.7 ± 21.6 years, and 31 were male. Compared to the Control Group, the MVH Group showed greater aspirated secretion amount (3.9g versus 6.4g, p = 0.0001), variation in mean dynamic compliance (-1.3 ± 2.3 versus -2.9 ± 2.3; p = 0.008), and expired tidal volume (-0.7 ± 0.0 versus -54.1 ± 38.8, p = 0.0001) as well as a significant decrease in peak inspiratory pressure (0.2 ± 0.1 versus 2.5 ± 0.1; p = 0.001).
In the studied sample, the MVH technique led to a greater amount of aspirated secretions, significant increases in dynamic compliance and expired tidal volume and a significant reduction in peak inspiratory pressure.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):33-39
DOI 10.5935/0103-507X.20160011
The purpose of our study was to determine the admission factors associated with intensive care unit readmission among oncohematological patients.
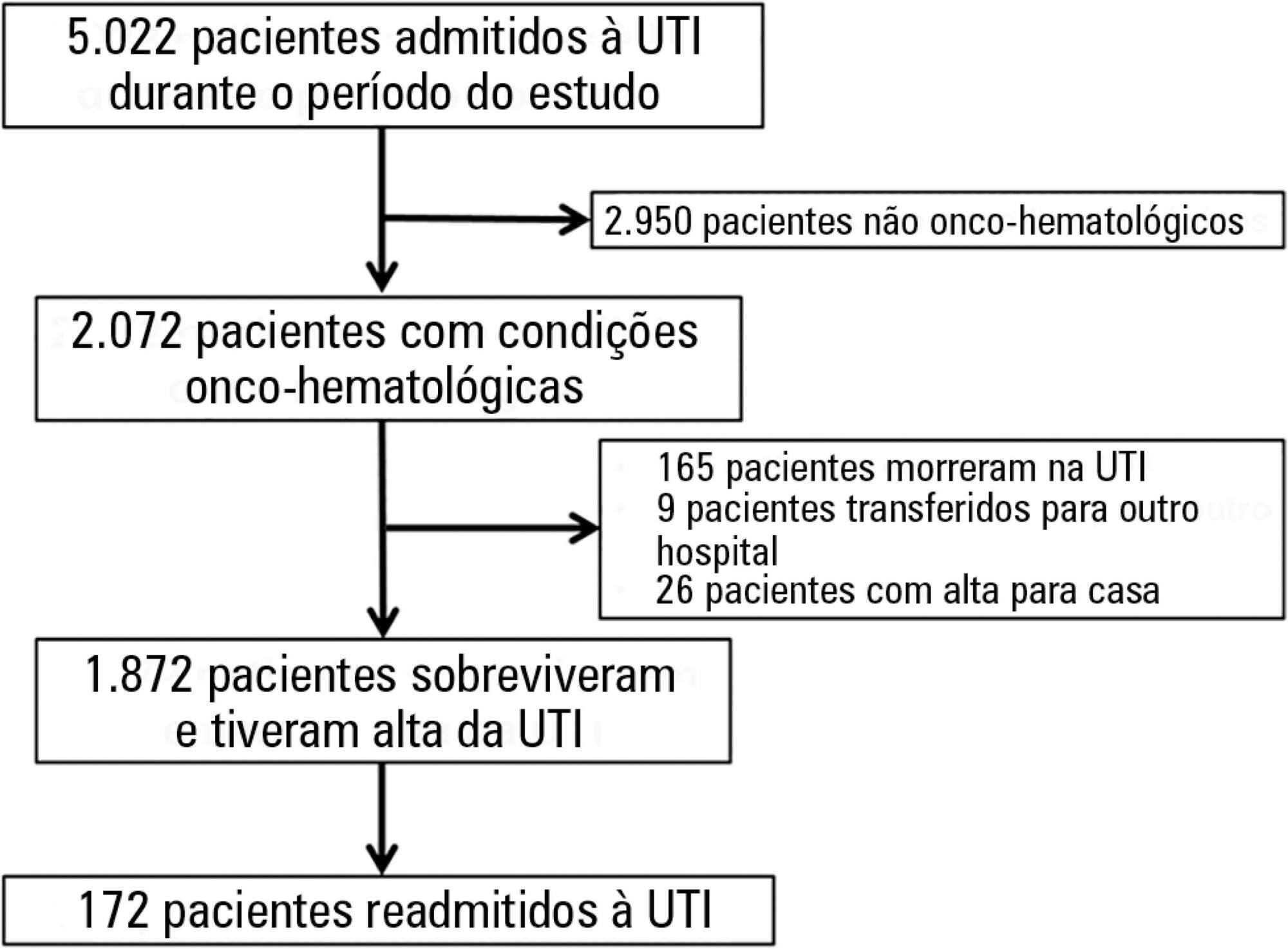
Retrospective cohort study using an intensive care unit database from a tertiary oncological center. The participants included 1,872 critically ill oncohematological patients who were admitted to the intensive care unit from January 2012 to December 2014 and who were subsequently discharged alive. We used univariate and multivariate analysis to identify the admission risk factors associated with later intensive care unit readmission.
One hundred seventy-two patients (9.2% of 1,872 oncohematological patients discharged alive from the intensive care unit) were readmitted after intensive care unit discharge. The readmitted patients were sicker compared with the non-readmitted group and had higher hospital mortality (32.6% versus 3.7%, respectively; p < 0.001). In the multivariate analysis, the independent risk factors for intensive care unit readmission were male sex (OR: 1.5, 95% CI: 1.07 - 2.12; p = 0.019), emergency surgery as the admission reason (OR: 2.91, 95%CI: 1.53 - 5.54; p = 0.001), longer hospital length of stay before intensive care unit transfer (OR: 1.02, 95%CI: 1.007 - 1.035; p = 0.003), and mechanical ventilation (OR: 2.31, 95%CI: 1.57 - 3.40; p < 0.001).
In this cohort of oncohematological patients, we identified some risk factors associated with intensive care unit readmission, most of which are not amenable to interventions. The identification of risk factors at intensive care unit discharge might be a promising approach.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):55-61
DOI 10.5935/0103-507X.20160003
To analyze the characteristics of children with acute viral bronchiolitis subjected to mechanical ventilation for three consecutive years and to correlate their progression with mechanical ventilation parameters and fluid balance.
Longitudinal study of a series of infants (< one year old) subjected to mechanical ventilation for acute viral bronchitis from January 2012 to September 2014 in the pediatric intensive care unit. The children's clinical records were reviewed, and their anthropometric data, mechanical ventilation parameters, fluid balance, clinical progression, and major complications were recorded.
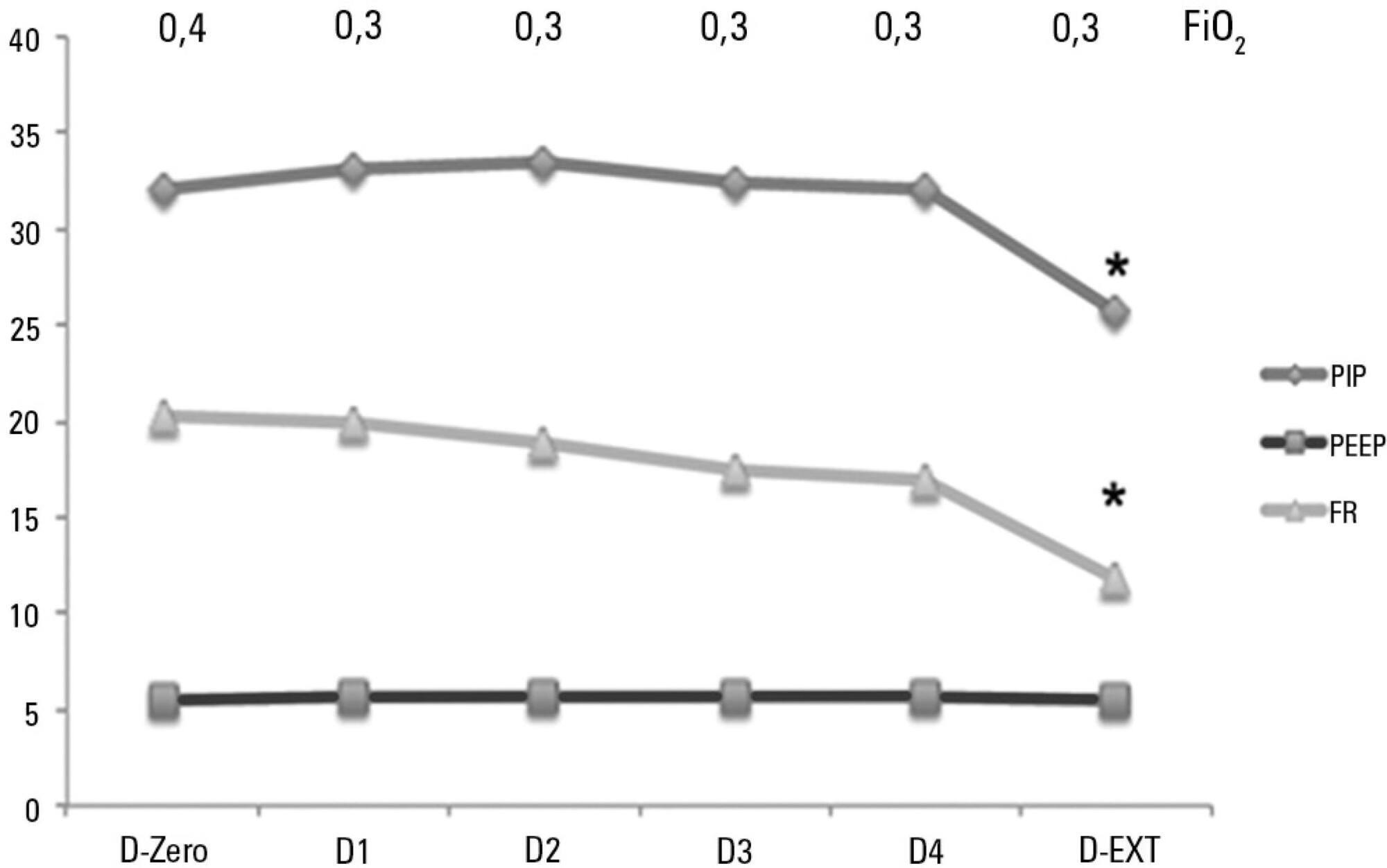
Sixty-six infants (3.0 ± 2.0 months old and with an average weight of 4.7 ± 1.4kg) were included, of whom 62% were boys; a virus was identified in 86%. The average duration of mechanical ventilation was 6.5 ± 2.9 days, and the average length of stay in the pediatric intensive care unit was 9.1 ± 3.5 days; the mortality rate was 1.5% (1/66). The peak inspiratory pressure remained at 30cmH2O during the first four days of mechanical ventilation and then decreased before extubation (25 cmH2O; p < 0.05). Pneumothorax occurred in 10% of the sample and extubation failure in 9%, which was due to upper airway obstruction in half of the cases. The cumulative fluid balance on mechanical ventilation day four was 402 ± 254mL, which corresponds to an increase of 9.0 ± 5.9% in body weight. Thirty-seven patients (56%) exhibited a weight gain of 10% or more, which was not significantly associated with the ventilation parameters on mechanical ventilation day four, extubation failure, duration of mechanical ventilation or length of stay in the pediatric intensive care unit.
The rate of mechanical ventilation for acute viral bronchiolitis remains constant, being associated with low mortality, few adverse effects, and positive cumulative fluid balance during the first days. Better fluid control might reduce the duration of mechanical ventilation.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):330-334
DOI 10.5935/0103-507X.20160056
To identify and evaluate the correct positioning of the most commonly used medical devices as visualized in thoracic radiograms of patients in the intensive care unit of our center.
A literature search was conducted for the criteria used to evaluate the correct positioning of medical devices on thoracic radiograms. All the thoracic radiograms performed in the intensive care unit of our center over an 18-month period were analyzed. All admissions in which at least one thoracic radiogram was performed in the intensive care unit and in which at least one medical device was identifiable in the thoracic radiogram were included. One radiogram per admission was selected for analysis. The radiograms were evaluated by an independent observer.
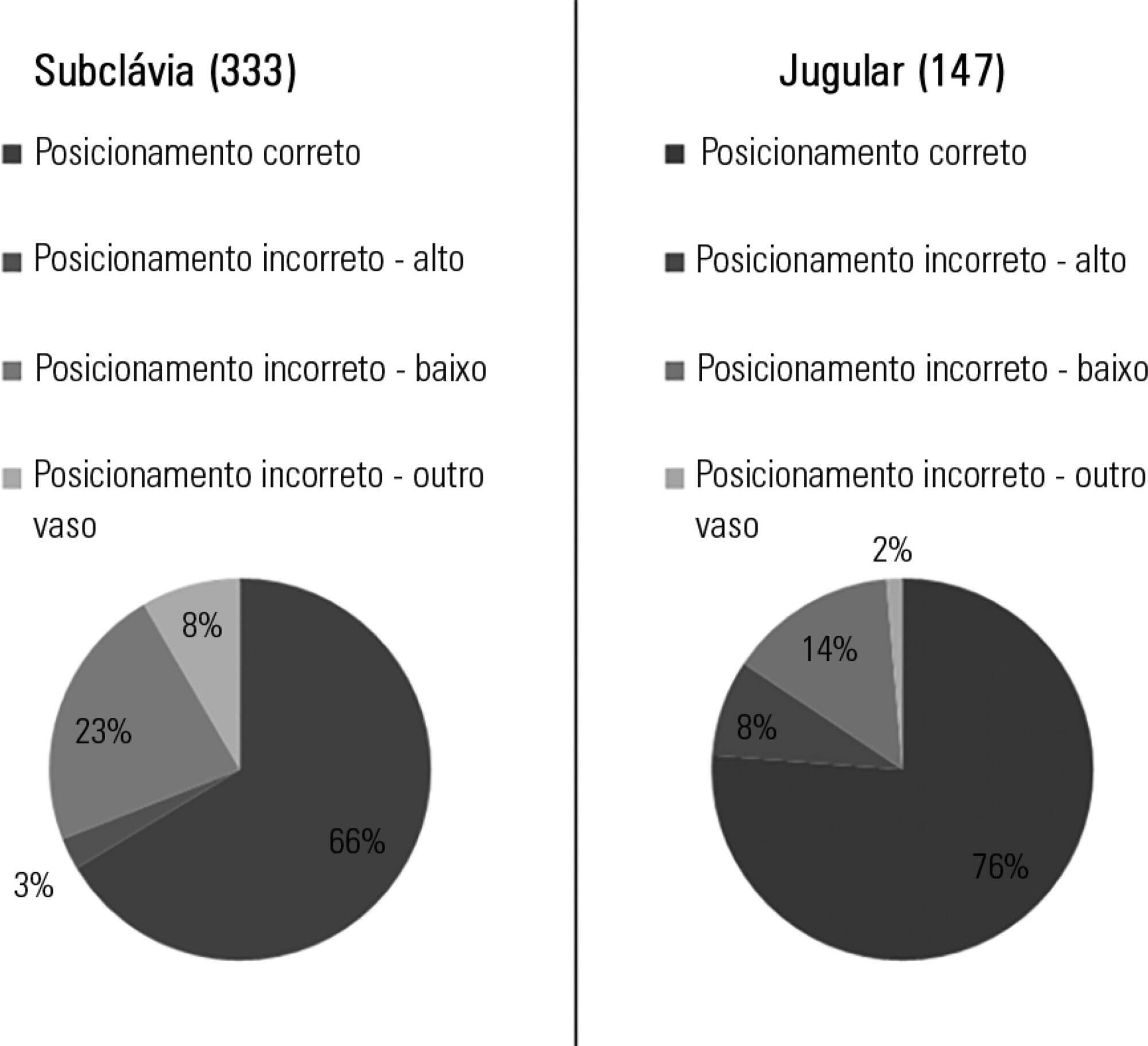
Out of the 2,312 thoracic radiograms analyzed, 568 were included in this study. Several medical devices were identified, including monitoring leads, endotracheal and tracheostomy tubes, central venous catheters, pacemakers and prosthetic cardiac valves. Of the central venous catheters that were identified, 33.6% of the subclavian and 23.8% of the jugular were malpositioned. Of the endotracheal tubes, 19.9% were malpositioned, while all the tracheostomy tubes were correctly positioned.
Malpositioning of central venous catheters and endotracheal tubes is frequently identified in radiograms of patients in an intensive care unit. This is relevant because malpositioned devices may be related to adverse events. In future studies, an association between malpositioning and adverse events should be investigated.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):147-153
DOI 10.5935/0103-507X.20160029
This study sought to identify the physical and chemical incompatibilities among the drugs administered intravenously to patients admitted to an adult intensive care unit. We also aimed to establish pharmaceutical guidelines for administering incompatible drugs.
This cross-sectional, prospective, and quantitative study was conducted from July to September 2015. Drug incompatibilities were identified based on an analysis of the patient prescriptions available in the hospital online management system. A pharmaceutical intervention was performed using the guidelines on the preparation and administration of incompatible drugs. Adherence to those guidelines was subsequently assessed among the nursing staff.
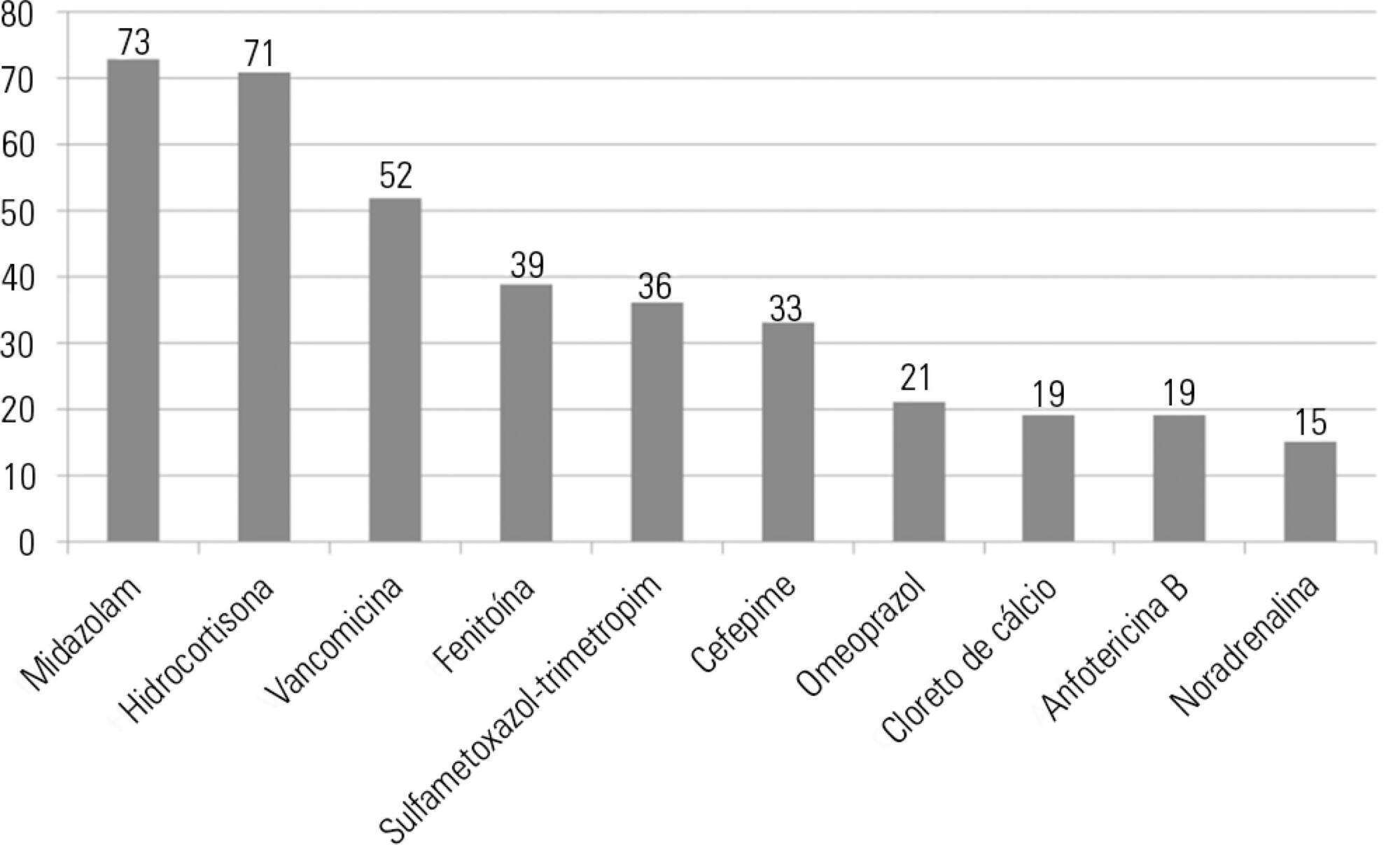
A total of 100 prescriptions were analyzed; 68 were incompatible with the intravenous drugs prescribed. A total of 271 drug incompatibilities were found, averaging 4.0 ± 3.3 incompatibilities per prescription. The most commonly found drug incompatibilities were between midazolam and hydrocortisone (8.9%), between cefepime and midazolam (5.2%), and between hydrocortisone and vancomycin (5.2%). The drugs most commonly involved in incompatibilities were midazolam, hydrocortisone, and vancomycin. The most common incompatibilities occurred when a drug was administered via continuous infusion and another was administered intermittently (50%). Of the 68 prescriptions that led to pharmaceutical guidelines, 45 (66.2%) were fully adhered to by the nursing staff.
Patients under intensive care were subjected to a high rate of incompatibilities. Drug incompatibilities can be identified and eliminated by the pharmacist on the multidisciplinary team, thereby reducing undesirable effects among patients.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):270-277
DOI 10.5935/0103-507X.20160053
To estimate the prevalence of burnout in intensivist doctors working in adult, pediatric and neonatal intensive care units in five Brazilian capitals.
Descriptive epidemiological study with a random sample stratified by conglomerate with 180 intensivist doctors from five capitals representing the Brazilian geographic regions: Porto Alegre (RS), Sao Paulo (SP), Salvador (BA), Goiania (GO) and Belem (PA). A self-administered questionnaire examining sociodemographic data and the level of burnout was evaluated through the Maslach Burnout Inventory.
A total of 180 doctors were evaluated, of which 54.4% were female. The average age was 39 ± 8.1 years, 63.4% had specialization as the highest degree, 55.7% had up to 10 years of work experience in an intensive care unit, and 46.1% had the title intensive care specialist. Most (50.3%) had weekly workloads between 49 and 72 hours, and the most frequent employee type was salaried. High levels of emotional exhaustion, depersonalization and inefficacy were found (50.6%, 26.1% and 15.0%, respectively). The prevalence of burnout was 61.7% when considering a high level in at least one dimension and 5% with a high level in three dimensions simultaneously.
A high prevalence of burnout syndrome among intensivist doctors was observed. Strategies for the promotion and protection of health in these workers must be discussed and implemented in hospitals.