Abstract
Rev Bras Ter Intensiva. 2016;28(3):301-309
DOI 10.5935/0103-507X.20160054
To describe the characteristics of patients with HIV/AIDS and to compare the therapeutic interventions and end-of-life care before and after evaluation by the palliative care team.
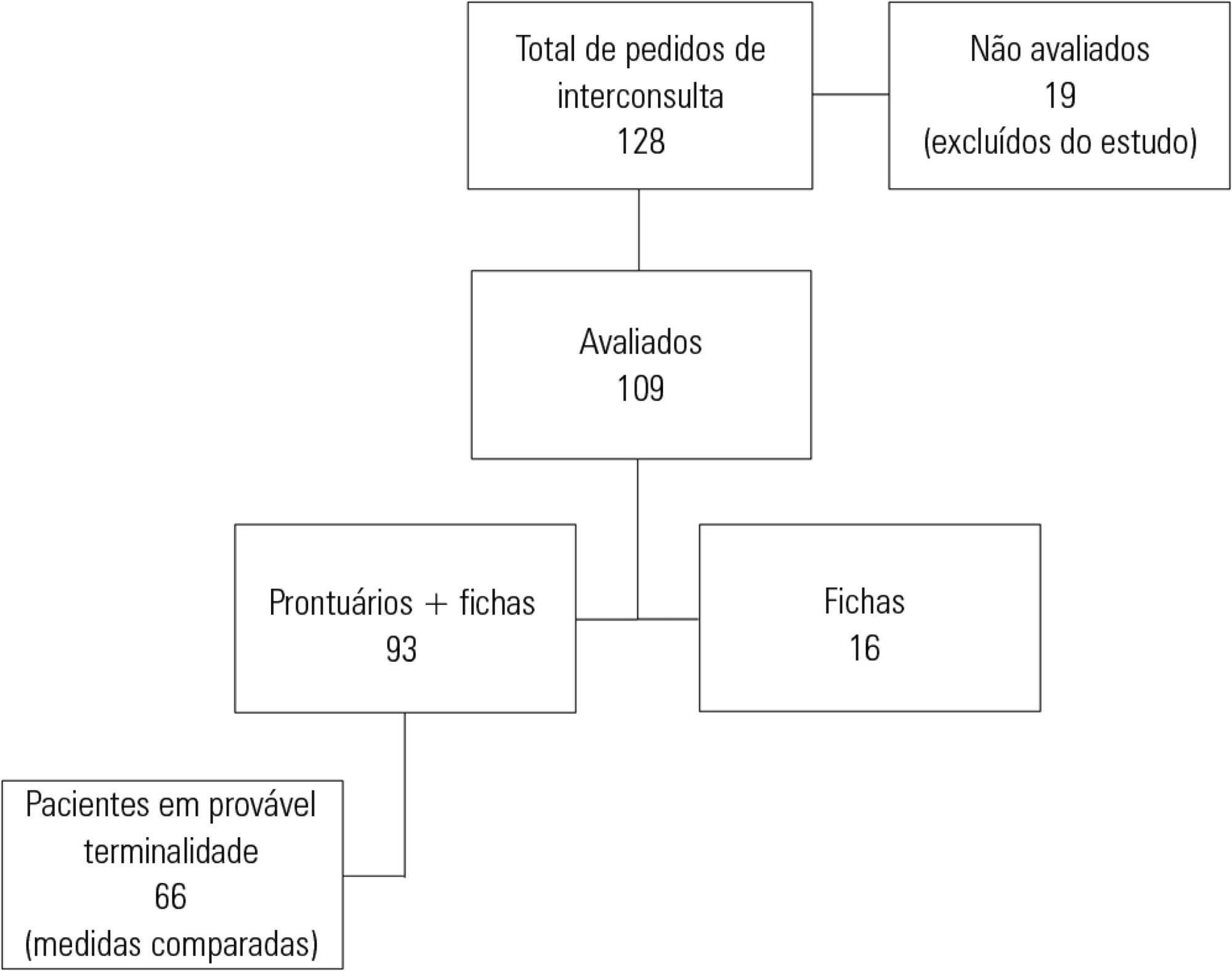
This retrospective cohort study included all patients with HIV/AIDS admitted to the intensive care unit of the Instituto de Infectologia Emílio Ribas who were evaluated by a palliative care team between January 2006 and December 2012.
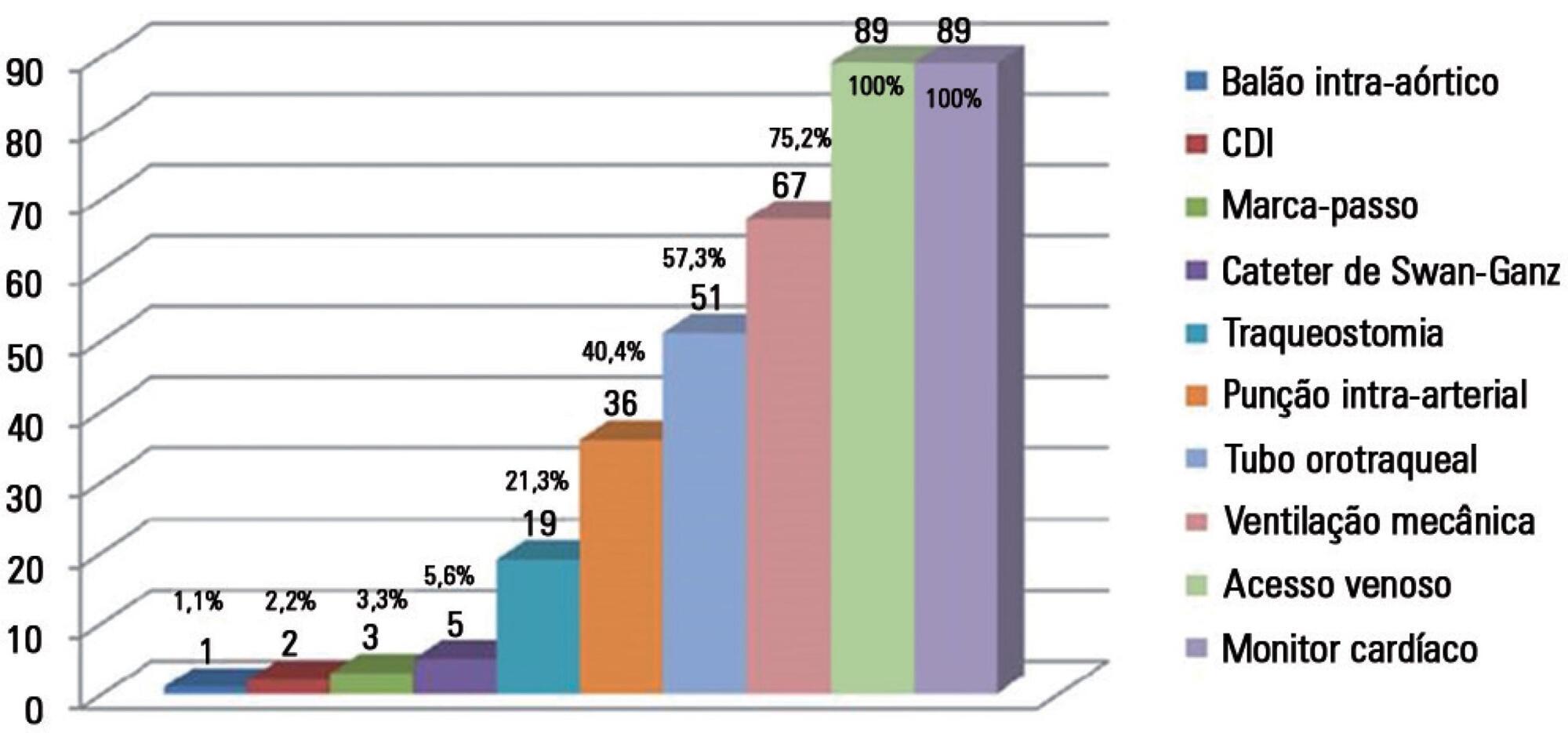
Of the 109 patients evaluated, 89% acquired opportunistic infections, 70% had CD4 counts lower than 100 cells/mm3, and only 19% adhered to treatment. The overall mortality rate was 88%. Among patients predicted with a terminally ill (68%), the use of highly active antiretroviral therapy decreased from 50.0% to 23.1% (p = 0.02), the use of antibiotics decreased from 100% to 63.6% (p < 0.001), the use of vasoactive drugs decreased from 62.1% to 37.8% (p = 0.009), the use of renal replacement therapy decreased from 34.8% to 23.0% (p < 0.0001), and the number of blood product transfusions decreased from 74.2% to 19.7% (p < 0.0001). Meetings with the family were held in 48 cases, and 23% of the terminally ill patients were discharged from the intensive care unit.
Palliative care was required in patients with severe illnesses and high mortality. The number of potentially inappropriate interventions in terminally ill patients monitored by the palliative care team significantly decreased, and 26% of the patients were discharged from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):107-113
DOI 10.5935/0103-507X.20160024
To evaluate job and personal satisfaction rates in physicians who work in adult intensive care units and to identify the factors associated with satisfaction.
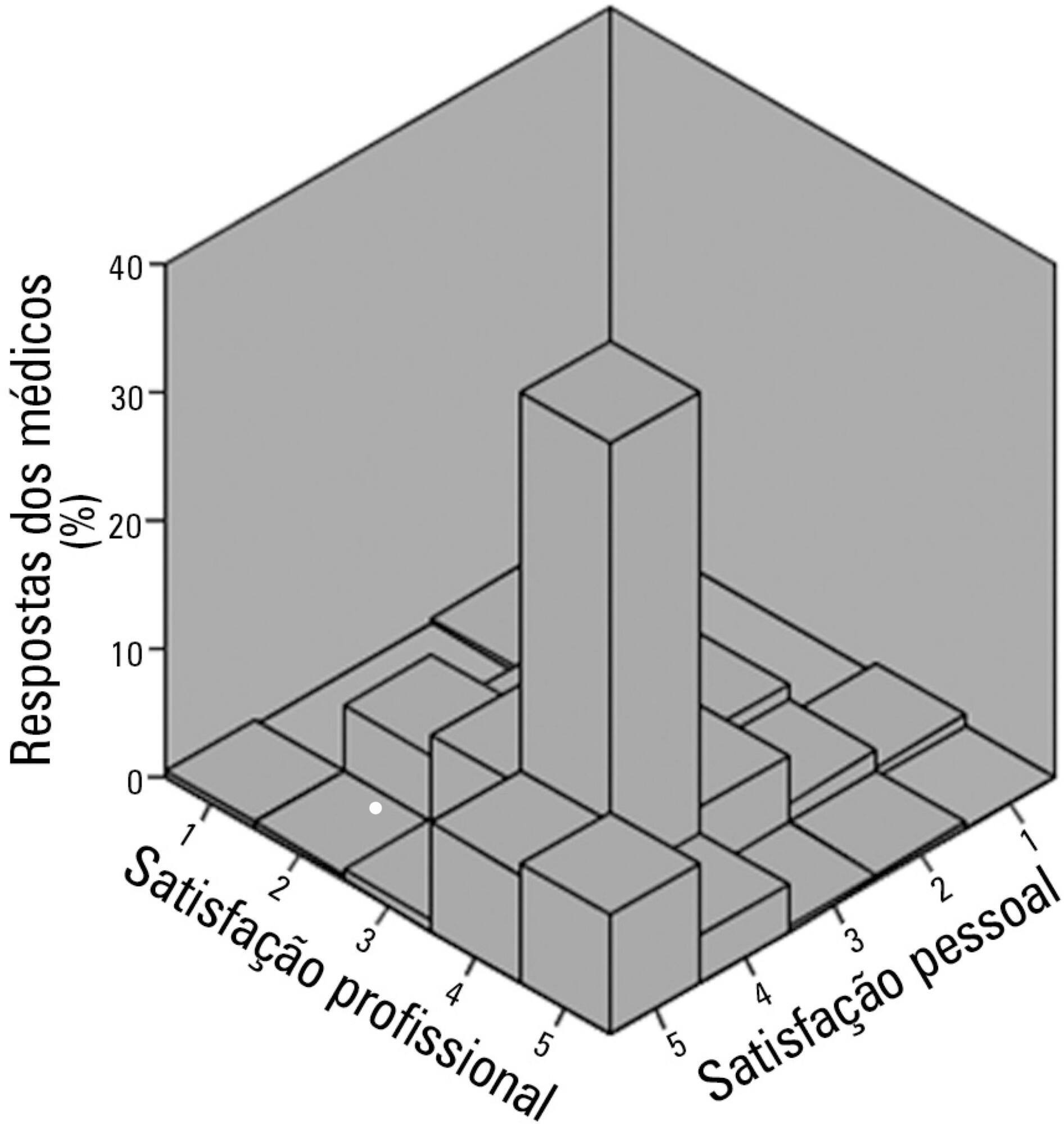
A cross-sectional study performed with physicians who participated in two intensive medicine online discussion groups. A questionnaire designed to assess the physician's sociodemographic profile and job was available for both groups for 3 months. At the end of the questionnaire, the participants addressed their degrees of job and personal satisfaction using a Likert scale in which 1 represented "very dissatisfied" and 5 represented "very satisfied". The association between sociodemographic and job characteristics with job and personal satisfaction was evaluated. Variables independently associated with satisfaction were identified using a logistic regression model.
The questionnaire was answered by 250 physicians, of which 137 (54.8%) declared they were satisfied with their jobs and 34 (13.5%) were very satisfied. None of the evaluated characteristics were independently associated with job satisfaction. Regarding personal satisfaction, 136 (54.4%) physicians reported being satisfied, and 48 (19.9%) reported being very satisfied. Job satisfaction (OR = 7.21; 95%CI 3.21 - 16.20) and working in a university hospital (OR = 3.24; 95%CI 1.29 - 8.15) were factors independently associated with the personal satisfaction of the participants.
The participant physicians reported job and personal satisfaction with their work in intensive care. Job satisfaction and working in a university hospital were independently associated with greater personal satisfaction.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):323-329
DOI 10.5935/0103-507X.20160055
To identify and stratify the main stressors for the relatives of patients admitted to the adult intensive care unit of a teaching hospital.
Cross-sectional descriptive study conducted with relatives of patients admitted to an intensive care unit from April to October 2014. The following materials were used: a questionnaire containing identification information and demographic data of the relatives, clinical data of the patients, and 25 stressors adapted from the Intensive Care Unit Environmental Stressor Scale. The degree of stress caused by each factor was determined on a scale of values from 1 to 4. The stressors were ranked based on the average score obtained.
The main cause of admission to the intensive care unit was clinical in 36 (52.2%) cases. The main stressors were the patient being in a state of coma (3.15 ± 1.23), the patient being unable to speak (3.15 ± 1.20), and the reason for admission (3.00 ± 1.27). After removing the 27 (39.1%) coma patients from the analysis, the main stressors for the relatives were the reason for admission (2.75 ± 1.354), seeing the patient in the intensive care unit (2.51 ± 1.227), and the patient being unable to speak (2.50 ± 1.269).
Difficulties in communication and in the relationship with the patient admitted to the intensive care unit were identified as the main stressors by their relatives, with the state of coma being predominant. By contrast, the environment, work routines, and relationship between the relatives and intensive care unit team had the least impact as stressors.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):114-119
DOI 10.5935/0103-507X.20160025
To evaluate the variation in mobility during hospitalization in an intensive care unit and its association with hospital mortality.
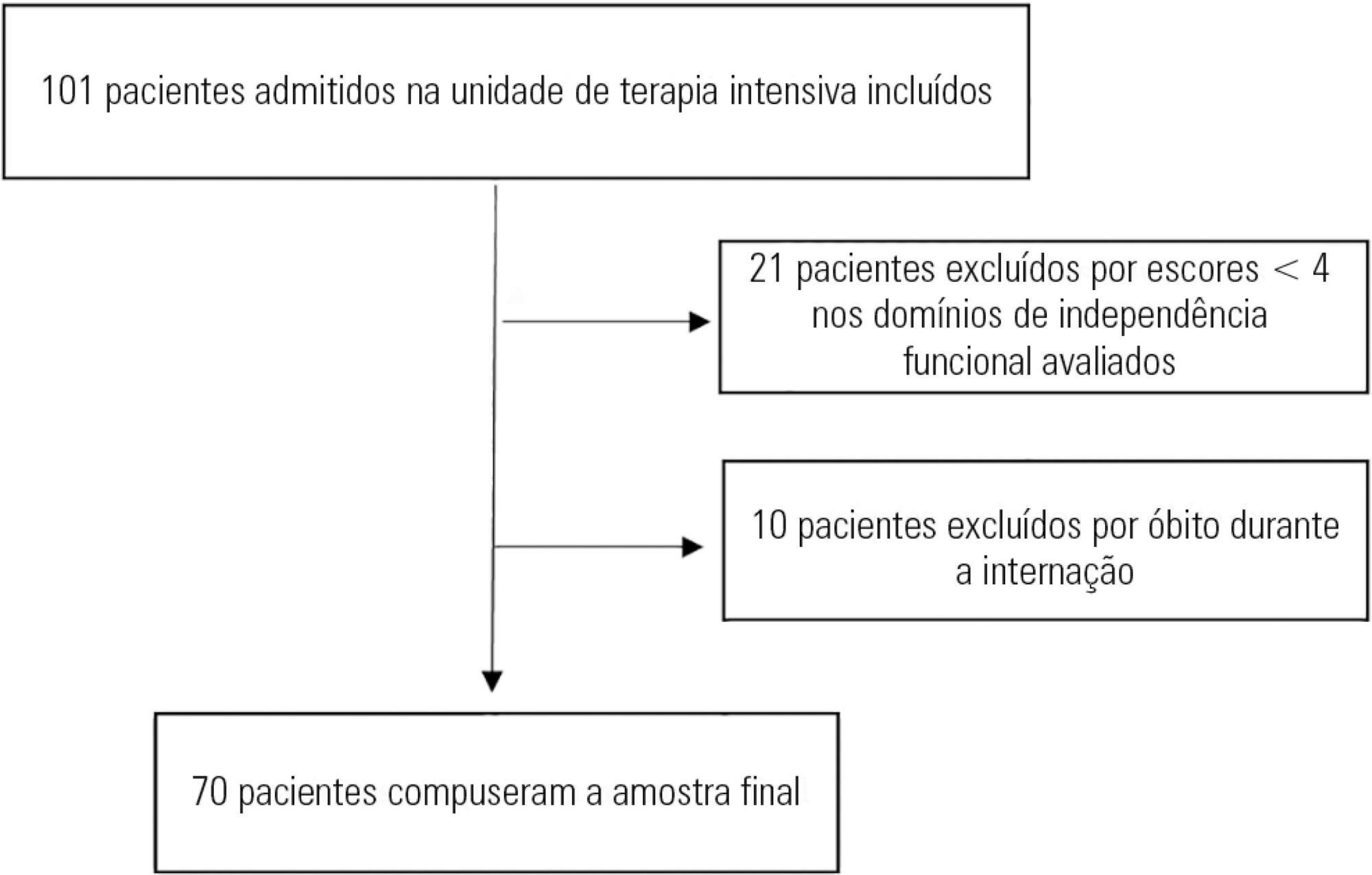
This prospective study was conducted in an intensive care unit. The inclusion criteria included patients admitted with an independence score of ≥ 4 for both bed-chair transfer and locomotion, with the score based on the Functional Independence Measure. Patients with cardiac arrest and/or those who died during hospitalization were excluded. To measure the loss of mobility, the value obtained at discharge was calculated and subtracted from the value obtained on admission, which was then divided by the admission score and recorded as a percentage.
The comparison of these two variables indicated that the loss of mobility during hospitalization was 14.3% (p < 0.001). Loss of mobility was greater in patients hospitalized for more than 48 hours in the intensive care unit (p < 0.02) and in patients who used vasopressor drugs (p = 0.041). However, the comparison between subjects aged 60 years or older and those younger than 60 years indicated no significant differences in the loss of mobility (p = 0.332), reason for hospitalization (p = 0.265), SAPS 3 score (p = 0.224), use of mechanical ventilation (p = 0.117), or hospital mortality (p = 0.063).
There was loss of mobility during hospitalization in the intensive care unit. This loss was greater in patients who were hospitalized for more than 48 hours and in those who used vasopressors; however, the causal and prognostic factors associated with this decline need to be elucidated.
Abstract
Rev Bras Ter Intensiva. 2016;28(2):195-198
DOI 10.5935/0103-507X.20160033
Ralstonia pickettii is a low-virulence gram-negative bacillus that may be associated with infections related to health care and may cause bacteremia. Ralstonia pickettii bacteremia is uncommon but is related to the contamination of medical products, mainly in immunodepressed patients. We present two cases of patients on chronic hemodialysis with Ralstonia pickettii bacteremia linked to contamination of the dialysis water. Similar cases have been published with links to intravenous fluid administration, medication ampules, and the use of extracorporeal oxygenation membranes, among other factors. The detection of Ralstonia pickettii bacteremia should provoke suspicion and a search for contaminated medical products, fluids, and/or medications.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):397-404
DOI 10.5935/0103-507X.20160073
To identify factors associated with maternal death in patients admitted to an intensive care unit.
A cross-sectional study was conducted in a maternal intensive care unit. All medical records of patients admitted from January 2012 to December 2014 were reviewed. Pregnant and puerperal women were included; those with diagnoses of hydatidiform mole, ectopic pregnancy, or anembryonic pregnancy were excluded, as were patients admitted for non-obstetrical reasons. Death and hospital discharge were the outcomes subjected to comparative analysis.
A total of 373 patients aged 13 to 45 years were included. The causes for admission to the intensive care unit were hypertensive disorders of pregnancy, followed by heart disease, respiratory failure, and sepsis; complications included acute kidney injury (24.1%), hypotension (15.5%), bleeding (10.2%), and sepsis (6.7%). A total of 28 patients died (7.5%). Causes of death were hemorrhagic shock, multiple organ failure, respiratory failure, and sepsis. The independent risk factors associated with death were acute kidney injury (odds ratio [OR] = 6.77), hypotension (OR = 15.08), and respiratory failure (OR = 3.65).
The frequency of deaths was low. Acute kidney injury, hypotension, and respiratory insufficiency were independent risk factors for maternal death.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):427-435
DOI 10.5935/0103-507X.20160076
The objective of this study was to analyze the clinical profile of patients with in-hospital cardiac arrest using the Utstein style.
This study is an observational, prospective, longitudinal study of patients with cardiac arrest treated in intensive care units over a period of 1 year.
The study included 89 patients who underwent cardiopulmonary resuscitation maneuvers. The cohort was 51.6% male with a mean age 59.0 years. The episodes occurred during the daytime in 64.6% of cases. Asystole/bradyarrhythmia was the most frequent initial rhythm (42.7%). Most patients who exhibited a spontaneous return of circulation experienced recurrent cardiac arrest, especially within the first 24 hours (61.4%). The mean time elapsed between hospital admission and the occurrence of cardiac arrest was 10.3 days, the mean time between cardiac arrest and cardiopulmonary resuscitation was 0.68 min, the mean time between cardiac arrest and defibrillation was 7.1 min, and the mean duration of cardiopulmonary resuscitation was 16.3 min. Associations between gender and the duration of cardiopulmonary resuscitation (19.2 min in women versus 13.5 min in men, p = 0.02), the duration of cardiopulmonary resuscitation and the return of spontaneous circulation (10.8 min versus 30.7 min, p < 0.001) and heart disease and age (60.6 years versus 53.6, p < 0.001) were identified. The immediate survival rates after cardiac arrest, until hospital discharge and 6 months after discharge were 71%, 9% and 6%, respectively.
The main initial rhythm detected was asystole/bradyarrhythmia; the interval between cardiac arrest and cardiopulmonary resuscitation was short, but defibrillation was delayed. Women received cardiopulmonary resuscitation for longer periods than men. The in-hospital survival rate was low.