Abstract
Rev Bras Ter Intensiva. 2019;31(2):240-247
DOI 10.5935/0103-507X.20190039
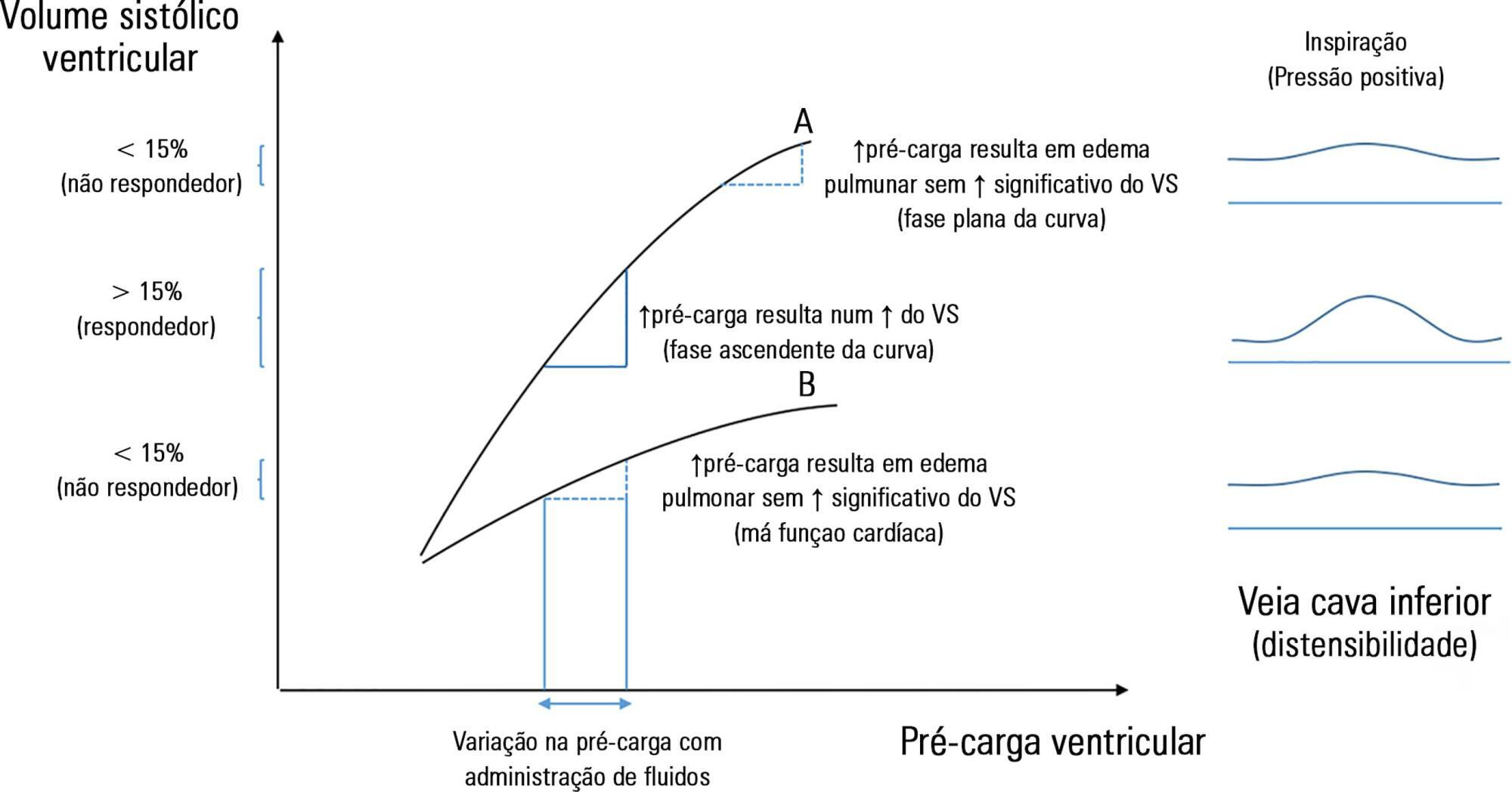
The fluid resuscitation of patients with acute circulatory failure aims to increase systolic volume and consequently improve cardiac output for better tissue oxygenation. However, this effect does not always occur because approximately half of patients do not respond to fluids. The evaluation of fluid responsiveness before their administration may help to identify patients who would benefit from fluid resuscitation and avoid the risk of fluid overload in the others. The dynamic parameters of fluid responsiveness evaluation are promising predictive factors. Of these, the echocardiographic measurement of the respiratory variation in the inferior vena cava diameter is easy to apply and has been used in the hemodynamic evaluation of intensive care unit patients. However, the applicability of this technique has many limitations, and the present studies are heterogeneous and inconsistent across specific groups of patients. We review the use of the inferior vena cava diameter respiratory variation, measured via transthoracic echocardiography, to decide whether to administer fluids to patients with acute circulatory failure in the intensive care unit. We explore the benefits and limitations of this technique, its current use, and the existing evidence.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):47-56
DOI 10.5935/0103-507X.20190011
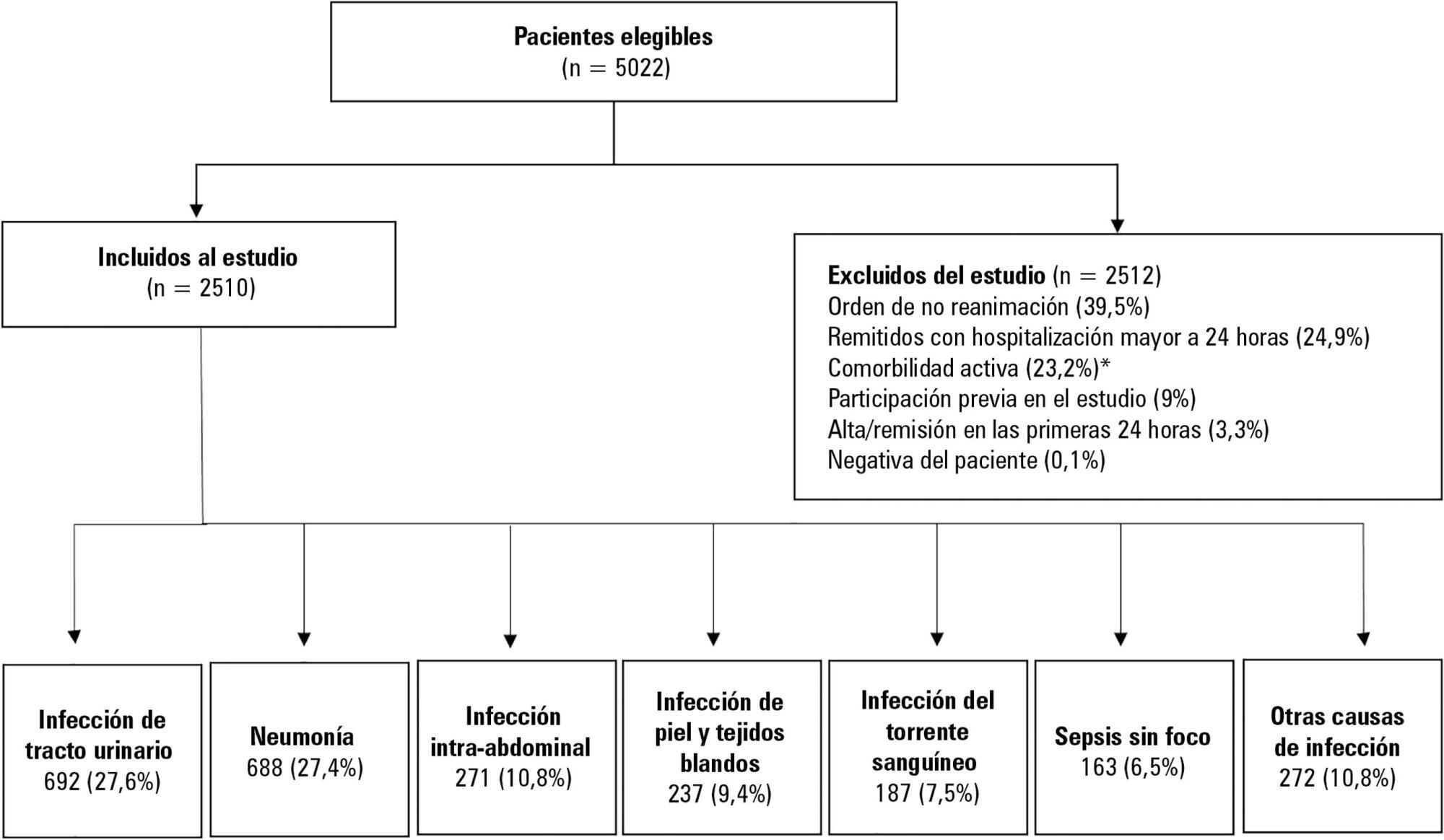
To determine the association between the primary site of infection and in-hospital mortality as the main outcome, or the need for admission to the intensive care unit as a secondary outcome, in patients with sepsis admitted to the emergency department.
This was a secondary analysis of a multicenter prospective cohort. Patients included in the study were older than 18 years with a diagnosis of severe sepsis or septic shock who were admitted to the emergency departments of three tertiary care hospitals. Of the 5022 eligible participants, 2510 were included. Multiple logistic regression analysis was performed for mortality.
The most common site of infection was the urinary tract, present in 27.8% of the cases, followed by pneumonia (27.5%) and intra-abdominal focus (10.8%). In 5.4% of the cases, no definite site of infection was identified on admission. Logistic regression revealed a significant association between the following sites of infection and in-hospital mortality when using the urinary infection group as a reference: pneumonia (OR 3.4; 95%CI, 2.2 - 5.2; p < 0.001), skin and soft tissues (OR 2.6; 95%CI, 1.4 - 5.0; p = 0.003), bloodstream (OR 2.0; 95%CI, 1.1 - 3.6; p = 0.018), without specific focus (OR 2.0; 95%CI, 1.1 - 3.8; p = 0.028), and intra-abdominal focus (OR 1.9; 95%CI, 1.1 - 3.3; p = 0.024).
There is a significant association between the different sites of infection and in-hospital mortality or the need for admission to an intensive care unit in patients with sepsis or septic shock. Urinary tract infection shows the lowest risk, which should be considered in prognostic models of these conditions.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):166-173
DOI 10.5935/0103-507X.20180022
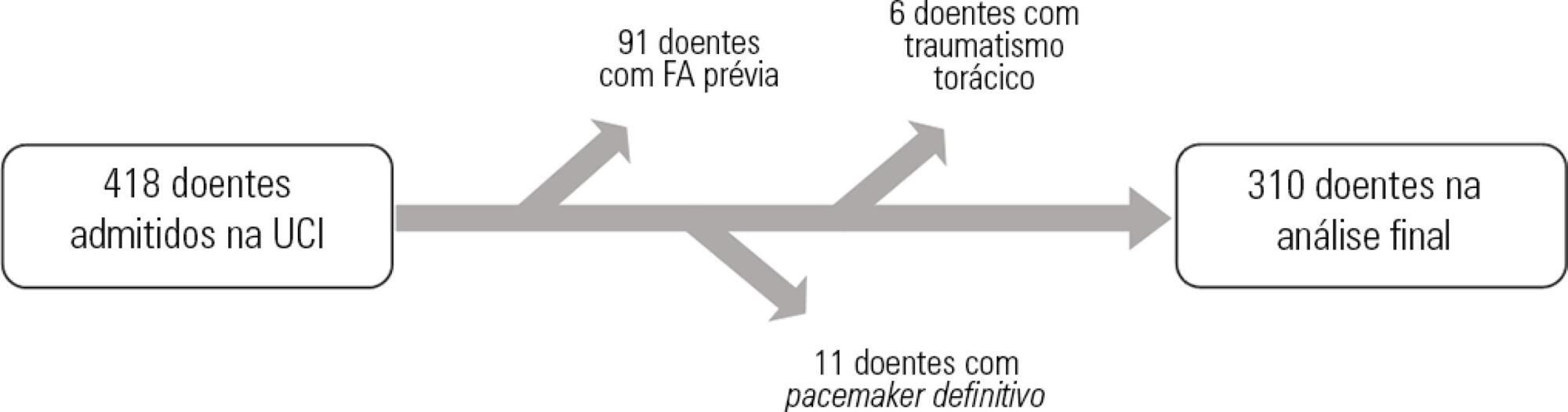
To assess the predictors of de novo atrial fibrillation in patients in a non-cardiac intensive care unit.
A total of 418 hospitalized patients were analyzed between January and September 2016 in a non-cardiac intensive care unit. Clinical characteristics, interventions, and biochemical markers were recorded during hospitalization. In-hospital mortality and length of hospital stay in the intensive care unit were also evaluated.
A total of 310 patients were included. The mean age of the patients was 61.0 ± 18.3 years, 49.4% were male, and 23.5% presented de novo atrial fibrillation. The multivariate model identified previous stroke (OR = 10.09; p = 0.016) and elevated levels of pro-B type natriuretic peptide (proBNP, OR = 1.28 for each 1,000pg/mL increment; p = 0.004) as independent predictors of de novo atrial fibrillation. Analysis of the proBNP receiver operating characteristic curve for prediction of de novo atrial fibrillation revealed an area under the curve of 0.816 (p < 0.001), with a sensitivity of 65.2% and a specificity of 82% for proBNP > 5,666pg/mL. There were no differences in mortality (p = 0.370), but the lengths of hospital stay (p = 0.002) and stay in the intensive care unit (p = 0.031) were higher in patients with de novo atrial fibrillation.
A history of previous stroke and elevated proBNP during hospitalization were independent predictors of de novo atrial fibrillation in the polyvalent intensive care unit. The proBNP is a useful and easy- and quick-access tool in the stratification of atrial fibrillation risk.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):481-489
DOI 10.5935/0103-507X.20170072
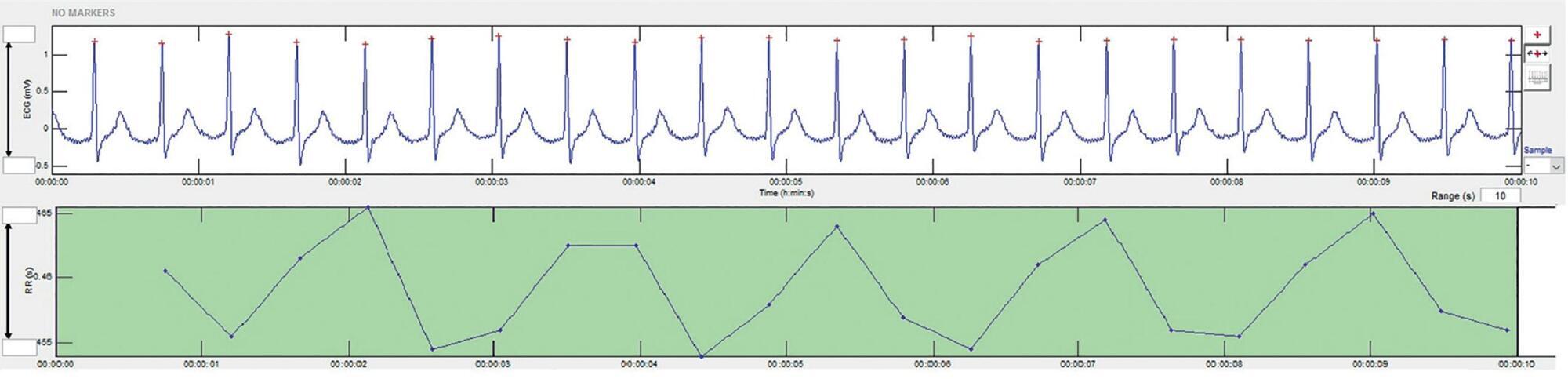
To present a systematic review of the use of autonomic nervous system monitoring as a prognostic tool in intensive care units by assessing heart rate variability.
Literature review of studies published until July 2016 listed in PubMed/Medline and conducted in intensive care units, on autonomic nervous system monitoring, via analysis of heart rate variability as a prognostic tool (mortality study). The following English terms were entered in the search field: ("autonomic nervous system" OR "heart rate variability") AND ("intensive care" OR "critical care" OR "emergency care" OR "ICU") AND ("prognosis" OR "prognoses" OR "mortality").
There was an increased likelihood of death in patients who had a decrease in heart rate variability as analyzed via heart rate variance, cardiac uncoupling, heart rate volatility, integer heart rate variability, standard deviation of NN intervals, root mean square of successive differences, total power, low frequency, very low frequency, low frequency/high frequency ratio, ratio of short-term to long-term fractal exponents, Shannon entropy, multiscale entropy and approximate entropy.
In patients admitted to intensive care units, regardless of the pathology, heart rate variability varies inversely with clinical severity and prognosis.
Abstract
Rev Bras Ter Intensiva. 2017;29(3):373-381
DOI 10.5935/0103-507X.20170051
Novel biomarkers can be suitable for early acute kidney injury diagnosis and the prediction of the need for dialysis. It remains unclear whether such biomarkers may also play a role in the prediction of recovery after established acute kidney injury or in aiding the decision of when to stop renal support therapy. PubMed, Web of Science and Google Scholar were searched for studies that reported on the epidemiology of renal recovery after acute kidney injury, the risk factors of recovery versus non-recovery after acute kidney injury, and potential biomarkers of acute kidney injury recovery. The reference lists of these articles and relevant review articles were also reviewed. Final references were selected for inclusion in the review based on their relevance. New biomarkers exhibited a potential role in the early diagnosis of acute kidney injury recovery. Urine HGF, IGFBP-7, TIMP-2 and NGAL may improve our ability to predict the odds and timing of recovery and eventually renal support withdrawal. Acute kidney injury recovery requires more study, and its definition needs to be standardized to allow for better and more powerful research on biomarkers because some of them show potential for the prediction of acute kidney injury recovery.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):413-419
DOI 10.5935/0103-507X.20160074
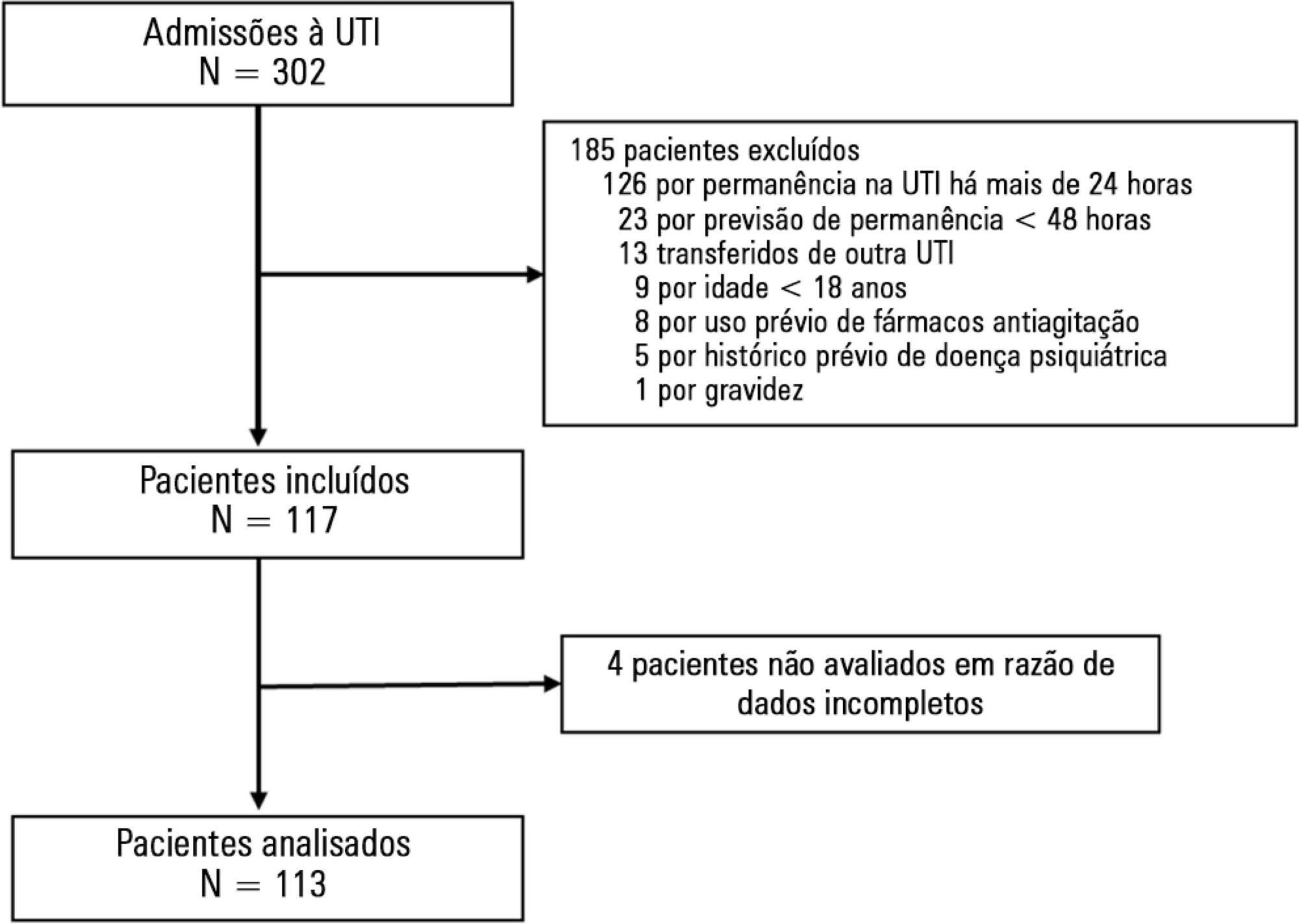
To evaluate the incidence of agitation in the first 7 days after intensive care unit admission, its risk factors and its associations with clinical outcomes.
This single-center prospective cohort study included all patients older than 18 years with a predicted stay > 48 hours within the first 24 hours of intensive care unit admission. Agitation was defined as a Richmond Agitation Sedation Scale score ≥ +2, an episode of agitation or the use of a specific medication recorded in patient charts.
Agitation occurred in 31.8% of the 113 patients. Multivariate analysis showed that delirium [OR = 24.14; CI95% 5.15 - 113.14; p < 0.001], moderate or severe pain [OR = 5.74; CI95% 1.73 - 19.10; p = 0.004], mechanical ventilation [OR = 10.14; CI95% 2.93 - 35.10; p < 0.001], and smoking habits [OR = 4.49; CI95% 1.33 - 15.17; p = 0.015] were independent factors for agitation, while hyperlactatemia was associated with a lower risk [OR = 0.169; CI95% 0.04 - 0.77; p = 0.021]. Agitated patients had fewer mechanical ventilation-free days at day 7 (p = 0.003).
The incidence of agitation in the first 7 days after admission to the intensive care unit was high. Delirium, moderate/severe pain, mechanical ventilation, and smoking habits were independent risk factors. Agitated patients had fewer ventilator-free days in the first 7 days.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):70-77
DOI 10.5935/0103-507X.20160015
Identify prognostic factors related to mortality and non-recovery of renal function.
A prospective single-center study was conducted at the intensive care medicine department of a university hospital between 2012 and 2015. Patients with acute kidney injury receiving continuous renal replacement therapy were included in the study. Clinical and analytical parameters were collected, and the reasons for initiation and discontinuation of renal replacement therapy were examined.
A total of 41 patients were included in the study, of whom 43.9% had sepsis. The median Simplified Acute Physiology Score II (SAPSII) was 56 and the mortality was 53.7%, with a predicted mortality of 59.8%. The etiology of acute kidney injury was often multifactorial (56.1%). Survivors had lower cumulative fluid balance (median = 3,600mL, interquartile range [IQR] = 1,175 - 8,025) than non-survivors (median = 12,000mL, IQR = 6,625 - 17,875; p = 0.004). Patients who recovered renal function (median = 51.0, IQR = 45.8 - 56.2) had lower SAPS II than those who do not recover renal function (median = 73, IQR = 54 - 85; p = 0.005) as well as lower fluid balance (median = 3,850, IQR = 1,425 - 8,025 versus median = 11,500, IQR = 6,625 - 16,275; p = 0.004).
SAPS II at admission and cumulative fluid balance during renal support therapy were risk factors for mortality and non-recovery of renal function among critically ill patients with acute kidney injury needing renal replacement therapy.