Abstract
Rev Bras Ter Intensiva. 2017;29(1):70-76
DOI 10.5935/0103-507X.20170011
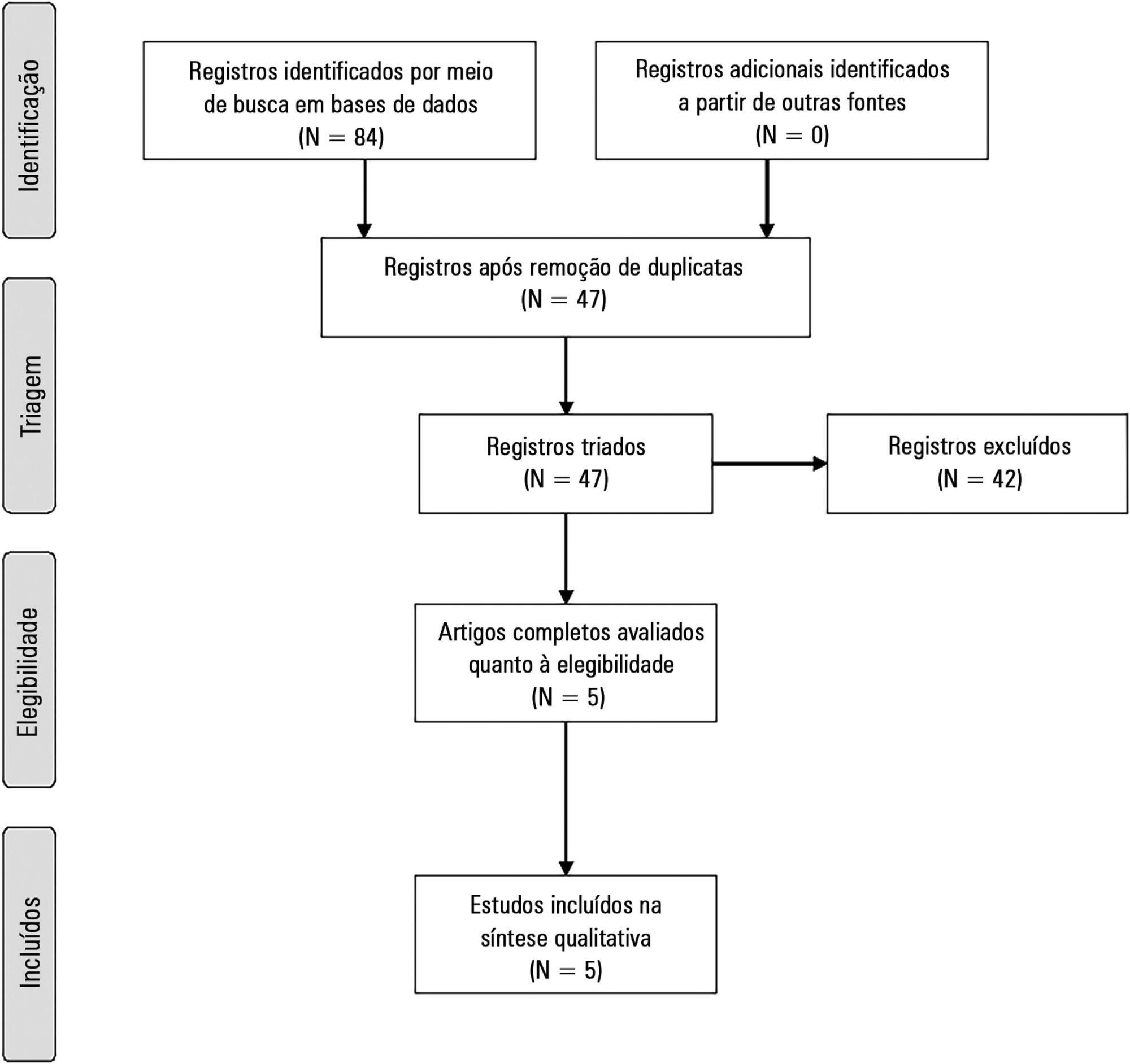
The present systematic review searched for published data on the prevalence of required conditions for proper assessment in critically ill patients.
The Medline, Scopus and Web of Science databases were searched to identify studies that evaluated the prevalence of validated conditions for the fluid responsiveness assessment using respiratory variations in the stroke volume or another surrogate in adult critically ill patients. The primary outcome was the suitability of the fluid responsiveness evaluation. The secondary objectives were the type and prevalence of pre-requisites evaluated to define the suitability.
Five studies were included (14,804 patients). High clinical and statistical heterogeneity was observed (I2 = 98.6%), which prevented us from pooling the results into a meaningful summary conclusion. The most frequent limitation identified is the absence of invasive mechanical ventilation with a tidal volume ≥ 8mL/kg. The final suitability for the fluid responsiveness assessment was low (in four studies, it varied between 1.9 to 8.3%, in one study, it was 42.4%).
Applicability of the dynamic indices of preload responsiveness requiring heart-lung interactions might be limited in daily practice.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):205-211
DOI 10.5935/0103-507X.20150042
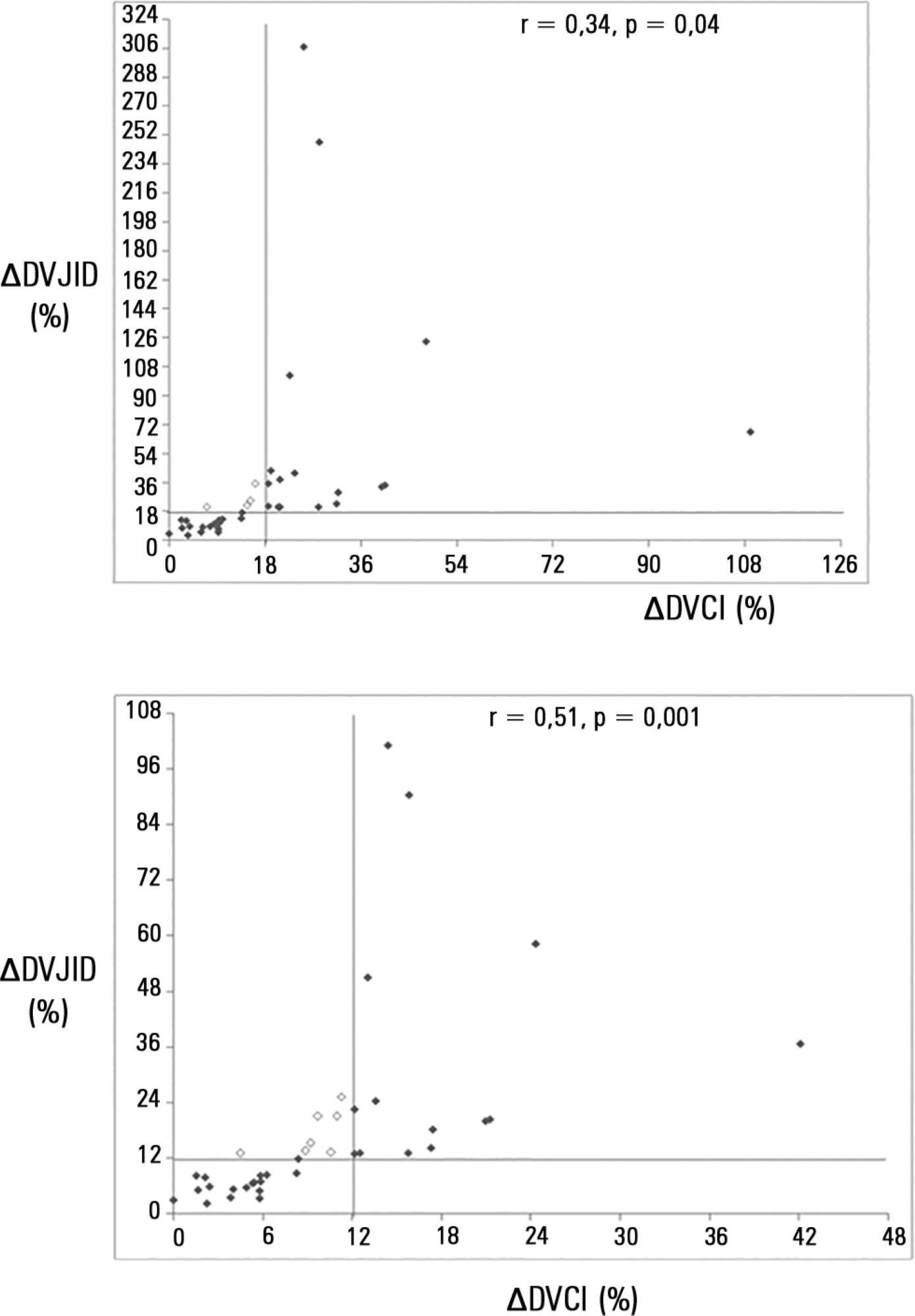
To investigate whether the respiratory variation of the inferior vena cava diameter (∆DIVC) and right internal jugular vein diameter (∆DRIJ) are correlated in mechanically ventilated patients.
This study was a prospective clinical analysis in an intensive care unit at a university hospital. Thirty-nine mechanically ventilated patients with hemodynamic instability were included. ∆DIVC and ∆DRIJ were assessed by echography. Vein distensibility was calculated as the ratio of (A) Dmax - Dmin/Dmin and (B) Dmax - Dmin/ mean of Dmax - Dmin and expressed as a percentage.
∆DIVC and ∆DRIJ were correlated by both methods: (A) r = 0.34, p = 0.04 and (B) r = 0.51, p = 0.001. Using 18% for ∆DIVC, indicating fluid responsiveness by method (A), 16 patients were responders and 35 measurements showed agreement (weighted Kappa = 0.80). The area under the ROC curve was 0.951 (95%CI 0.830 - 0.993; cutoff = 18.92). Using 12% for ∆DIVC, indicating fluid responsiveness by method (B), 14 patients were responders and 32 measurements showed agreement (weighted Kappa = 0.65). The area under the ROC curve was 0.903 (95%CI 0.765 - 0.973; cut-off value = 11.86).
The respiratory variation of the inferior vena cava and the right internal jugular veins are correlated and showed significant agreement. Evaluation of right internal jugular vein distensibility appears to be a surrogate marker for inferior vena cava vein distensibility for evaluating fluid responsiveness.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):168-174
DOI 10.5935/0103-507X.20130029
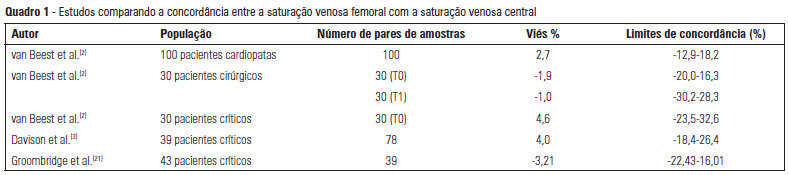
The use of central venous oxygen saturation (SvcO2) and arterial lactate in the diagnosis of severe tissue hypoperfusion is well established, and the optimization of these parameters is currently under investigation, particularly in patients with severe sepsis/septic shock. However, the only place for deep venous puncture or the first choice for puncture is often the femoral vein. Although venous saturation obtained from blood sampling from this catheter, instead of SvcO2, has already been used in the diagnosis of severe tissue hypoperfusion, little is known about the accuracy of the results. The venous lactate in place of arterial puncture has also been used to guide therapeutic decisions. We conducted this literature review to seek evidence on the correlation and concordance of parameters obtained by collecting femoral venous blood gases in relation to SvcO2 and arterial lactate. Few studies in the literature have evaluated the use of femoral venous oxygen saturation (SvfO2) or venous lactate. The results obtained thus far demonstrate no adequate agreement between SvfO2 and SvcO2, which limits the clinical use of SvfO2. However, the apparent strong correlation between arterial and peripheral and central venous lactate values suggests that venous lactate obtained from the femoral vein could eventually be used instead of arterial lactate, although there is insufficient evidence on which to base this procedure at this time.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
OBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients' satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 - 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):63-67
DOI 10.1590/S0103-507X2013000100012
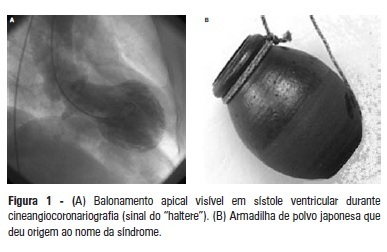
Takotsubo syndrome is characterized by predominantly medial-apical transient left ventricular dysfunction, which is typically triggered by physical or emotional stress. The present article reports the case of a 61-year-old female patient presenting with dizziness, excessive sweating, and sudden state of ill feeling following an episode involving intense emotional stress. The physical examination and electrocardiogram were normal upon admission, but the troponin I and creatine kinase-MB concentrations were increased. Acute myocardial infarction without ST segment elevation was suspected, and coronary angiography was immediately performed, which showed severe diffuse left ventricular hypokinesia, medial-apical systolic ballooning, and a lack of significant coronary injury. The patient was referred to the intensive care unit and was successfully treated with supportive therapy. As this case shows, Takotsubo syndrome might simulate the clinical manifestations of acute myocardial infarction, and coronary angiography is necessary to distinguish between both myocardial infarction and myocardial infarction in the acute stage. The present patient progressed with spontaneous resolution of the ventricular dysfunction without any sequelae.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):72-78
DOI 10.1590/S0103-507X2012000100011
OBJECTIVE: To assess the effects of passive mobilization on acute hemodynamic responses in mechanically ventilated patients. METHODS: This cross-sectional, quantitative, observational study enrolled patients who were admitted to the intensive care unit, sedated and mechanically ventilated. The infusion of sedative and analgesic drugs aimed to maintain a Ramsay scale sedation level of 4 to 6. Passive mobilization consisted of hip and knee flexion-extension movements for five minutes. After 10 minutes of rest, an additional five minutes of flexion-extension passive movements was performed for the shoulders. Hemodynamic assessments (heart rate and systolic, diastolic and mean blood pressure) were performed one minute before the mobilization protocol and one minute after each phase. The double product and myocardial oxygen consumption were calculated using appropriate formulas. RESULTS: A total of 13 patients (69.2% male, with a mean age of 69.1 ± 15.8 years) were admitted from June to December, 2011. Passive mobilization led to statistically significant increases in heart rate, double product and myocardial oxygen consumption. However, mean blood pressure was not significantly altered. CONCLUSIONS: Our results suggest that passive mobilization of mechanically ventilated and sedated patients is safe and provides beneficial effects on acute hemodynamic parameters, particularly heart rate, although mean blood pressure is not significantly altered
Abstract
Rev Bras Ter Intensiva. 2011;23(3):283-290
DOI 10.1590/S0103-507X2011000300005
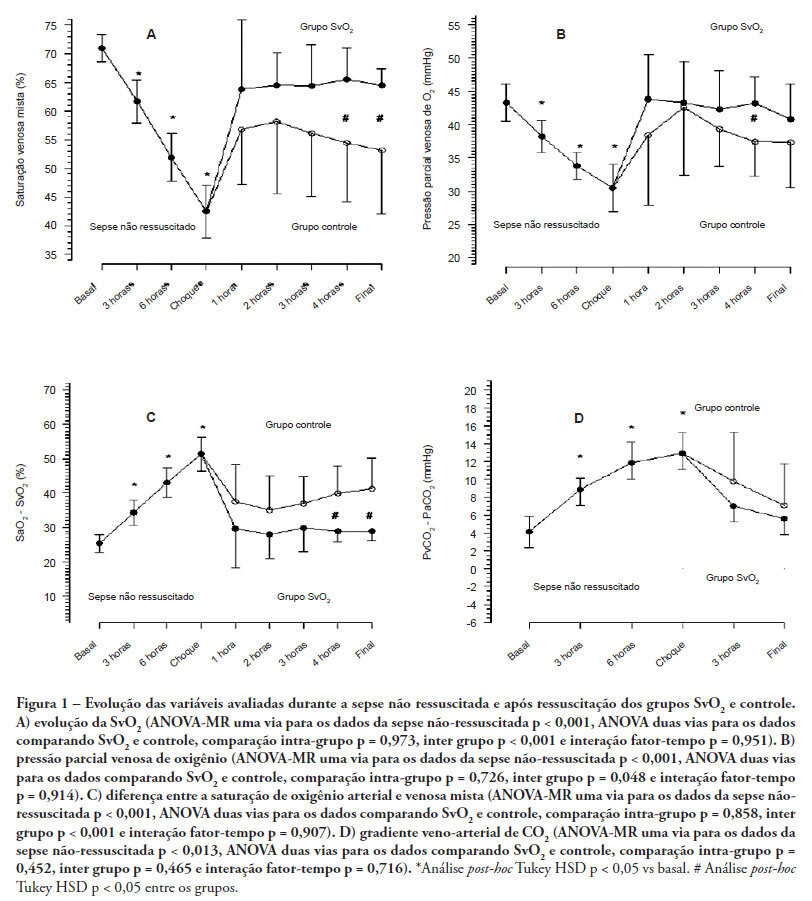
OBJECTIVES: Although fluid resuscitation guided by central venous oxygen saturation (SvcO2) is currently considered the gold standard in sepsis therapy, few studies have described hemodynamic and perfusion parameters during this procedure. This study aims to describe these parameters during septic shock without resuscitation and after 12 hours of goal-directed resuscitation. METHODS: Thirteen anesthetized pigs (35-45 kg) had peritonitis caused by fecal inoculation (0.75 g/kg). After developing persistent hypotension, both groups were given antibiotics and randomized either to the control group (n=7) or the experimental group (n=6). In the control group, hemodynamic control was optimized to maintain a central venous pressure of 8-12 mmHg, a urinary output above 0.5 mL/kg/hour and a mean arterial blood pressure above 65 mmHg. The experimental group received the above target therapy in addition to maintaining a SvO2 above 65%. The interventions included lactated Ringer's solution and norepinephrine for both groups and dobutamine in the SvO2 group. The animals were treated for 12 hours or until death. RESULTS: Untreated sepsis was associated with significant reductions in SvO2, PvO2, cardiac output and central venous pressure in addition to increased arteriovenous oxygen saturation and veno-arterial CO2 differences. Following resuscitation, these parameters were corrected in both groups. Goal-directed resuscitation was associated with a better hemodynamic profile, characterized by higher SvO2, cardiac output and central venous pressure. CONCLUSIONS: Non-resuscitated sepsis showed a hemodynamic profile suggesting hypovolemia, with worsened perfusion and hemodynamics, which is reversed upon fluid resuscitation. Goal-directed resuscitation is associated with significantly improved hemodynamic and perfusion parameters
Abstract
Rev Bras Ter Intensiva. 2011;23(3):352-357
DOI 10.1590/S0103-507X2011000300014
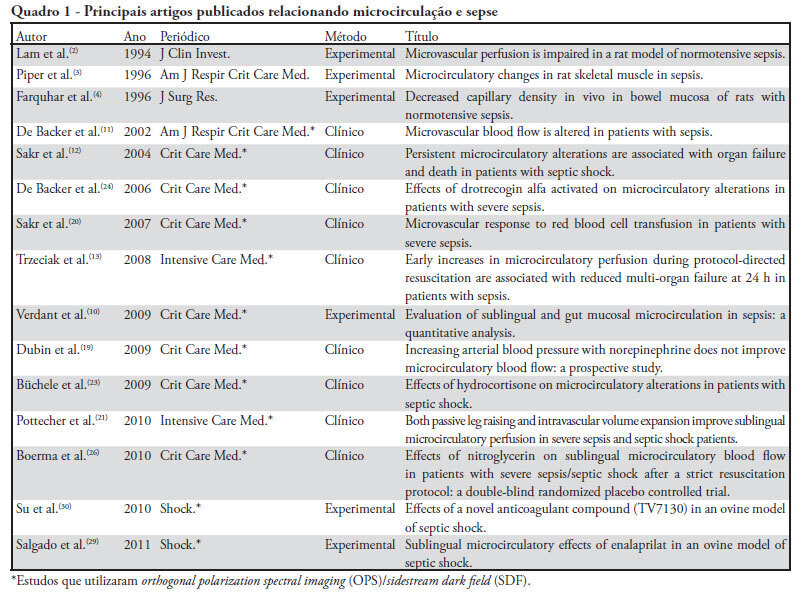
The progression into multi-organ failure continues to be a common feature of sepsis and is directly related to microcirculatory dysfunction. Based on a PubMed database search using the key words microcirculation and sepsis, twenty-six articles were selected for this review. The relevant references from these articles were also selected and included in this analysis. Orthogonal polarization spectral imaging allows for the bedside assessment of the microcirculation of critically ill patients. Such imaging has established a correlation between microvascular dysfunction and patient outcomes, which allows practitioners to directly assess the effects of therapeutic interventions. However, the causal relationships between microcirculatory dysfunction, adverse outcomes, and the effects of therapies aimed at these microcirculatory changes in sepsis, are not clear.