Abstract
. ;
Abstract
Revista Brasileira de Terapia Intensiva. 2017;29(3):331-336
DOI 10.5935/0103-507X.20170040
The goal was to determine the main drug-related problems in neonates who were using antimicrobials.
This was an observational, prospective and longitudinal study. Drug-related problems were classified according to version 6.2 of the Pharmaceutical Care Network Europe Foundation classification. A descriptive analysis was performed, in which the clinical and therapeutic variables were presented as absolute and relative frequencies or as the mean and standard deviation, as appropriate.
In total, 152 neonates with a predominance of males (58.5%), gestational age of 32.7 ± 4.2 weeks and weight of 1,903.1 ± 846.9g were included. The main diagnostic hypothesis of infection was early sepsis (66.5%), and 71.7% of the neonates had some risk factor for infection. Among the neonates, 33.6% had at least one drug-related problem. Of these, 84.8% were related to treatment effectiveness and 15.2% to adverse reactions. The main cause of drug-related problems was the selected dose, particularly for aminoglycosides and cephalosporins.
The use of antimicrobials in the neonatal intensive care is mainly associated with problems related to medication effectiveness, predominantly the prescription of subdoses of antimicrobials, especially aminoglycosides.
Abstract
Revista Brasileira de Terapia Intensiva. 2016;28(3):341-347
DOI 10.5935/0103-507X.20160058
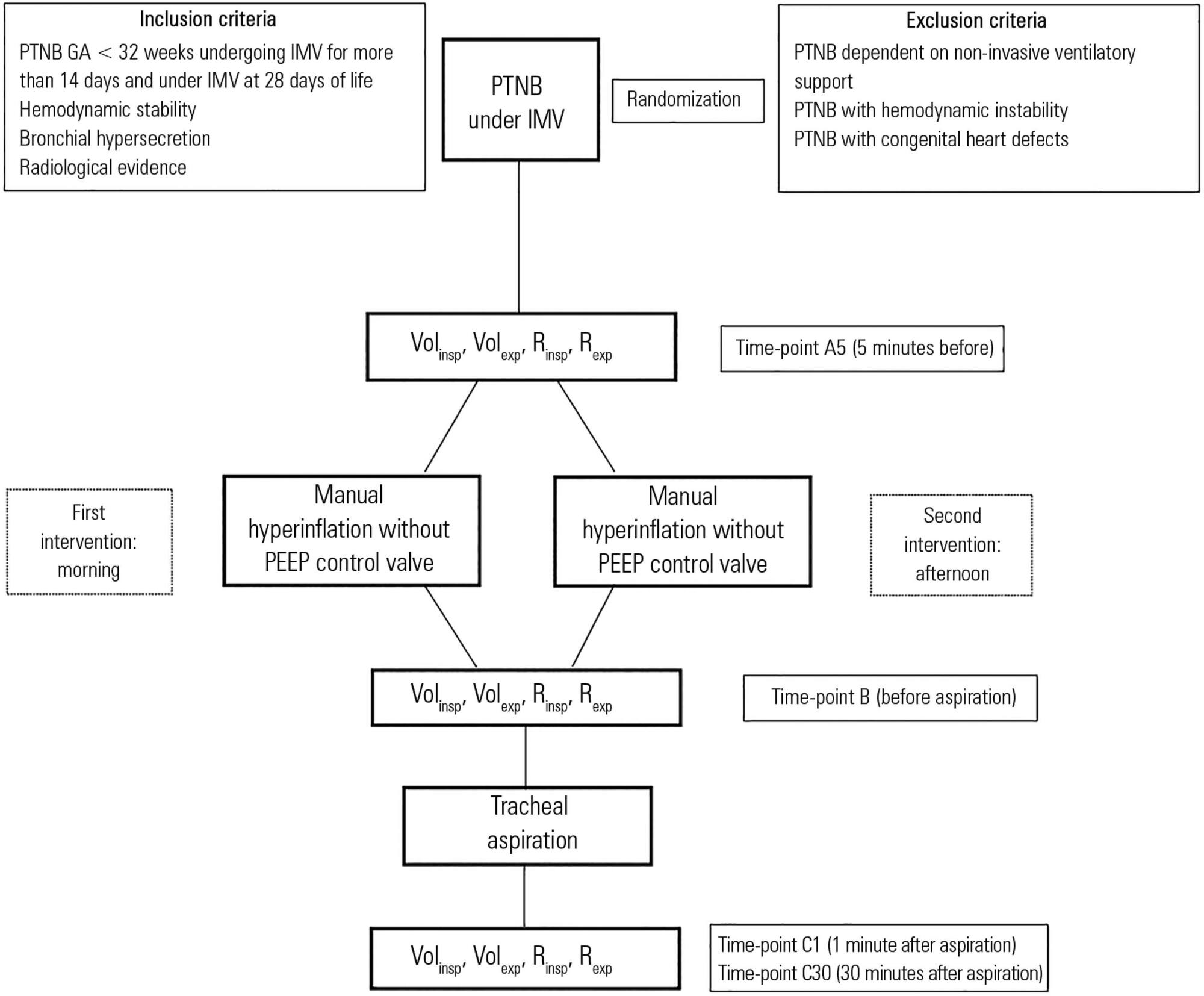
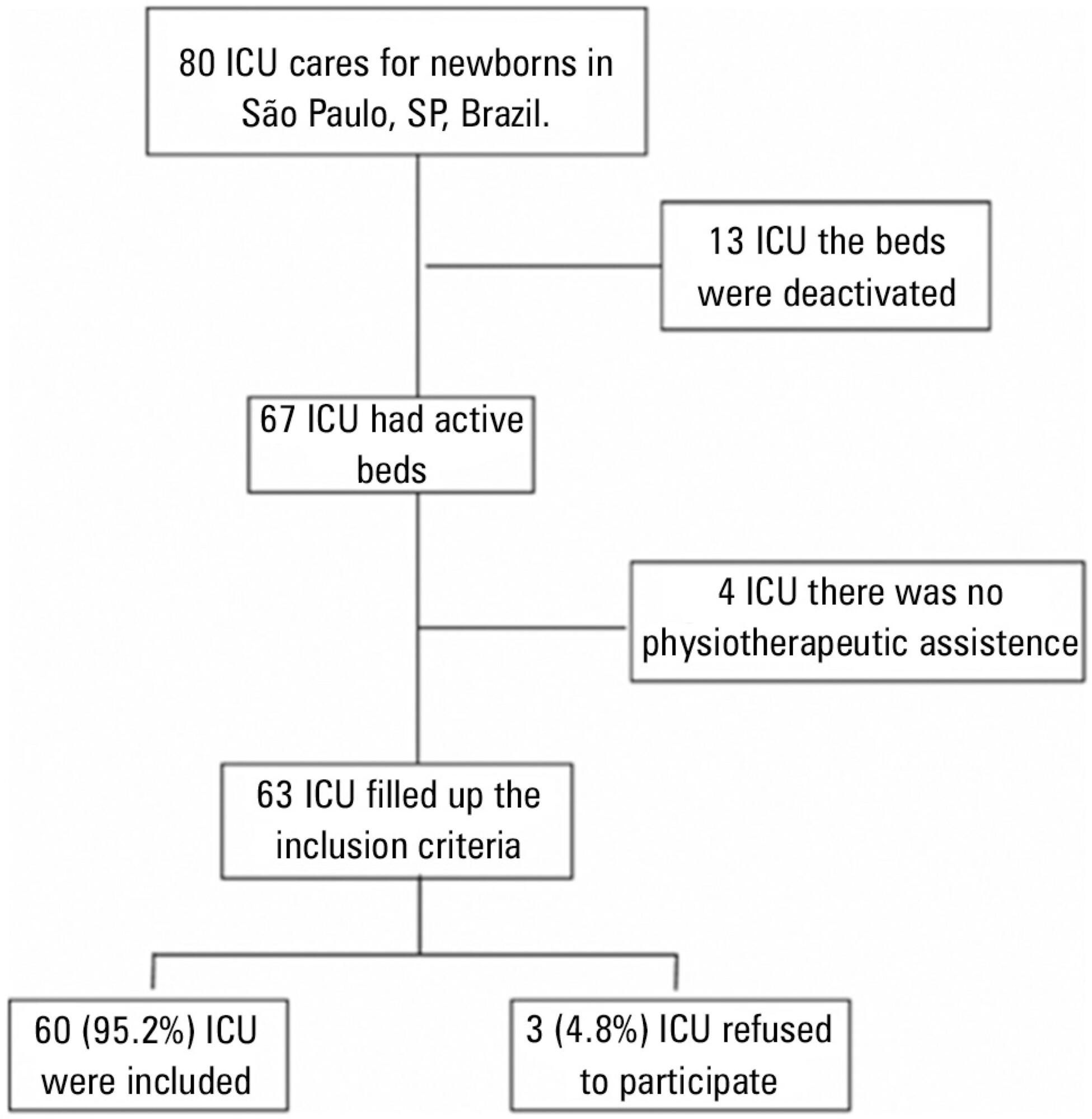
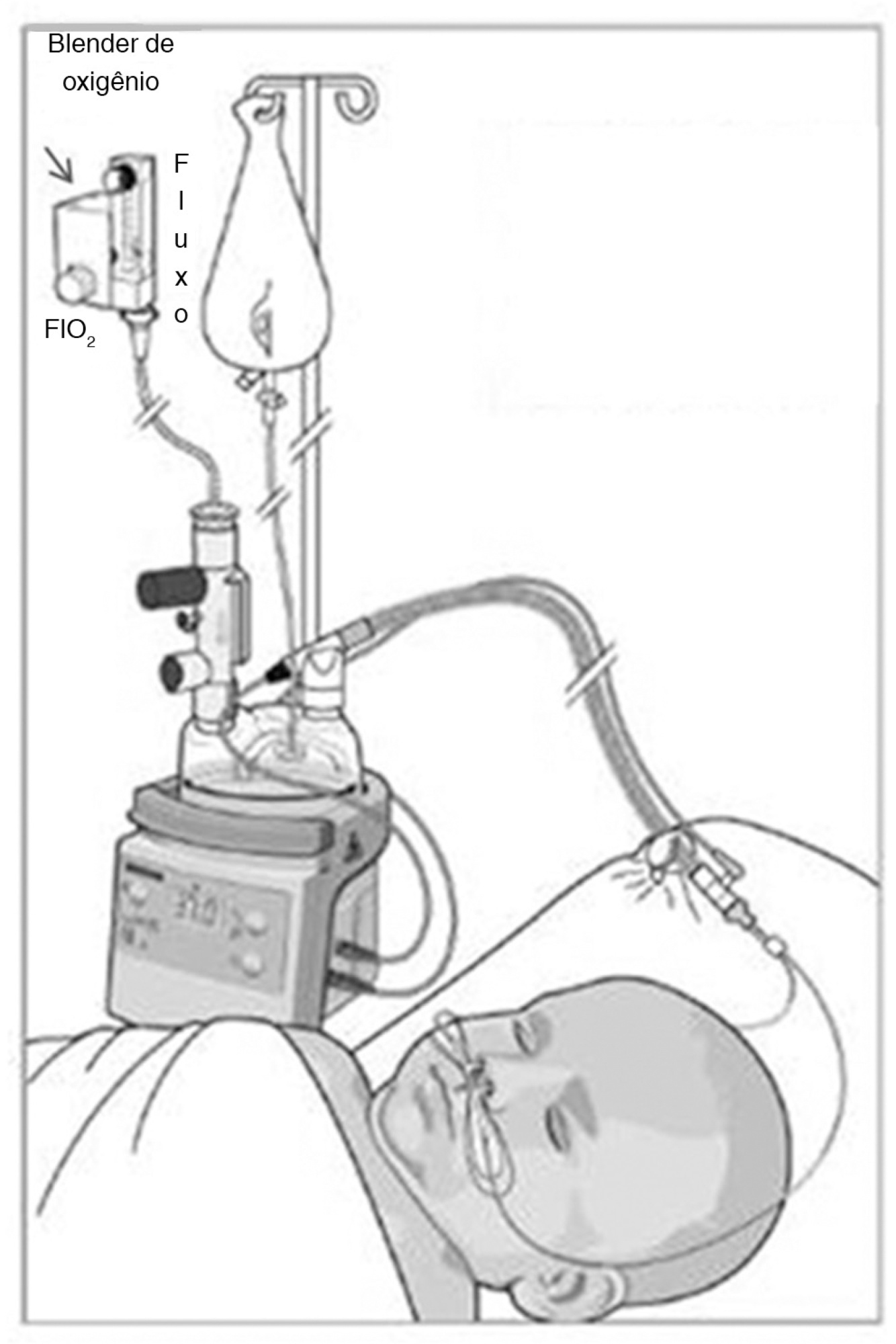
To assess the effects of manual hyperinflation, performed with a manual resuscitator with and without the positive end-expiratory pressure valve, on the respiratory function of preterm newborns under mechanical ventilation.
Cross-sectional study of hemodynamically stable preterm newborns with gestational age of less than 32 weeks, under mechanical ventilation and dependent on it at 28 days of life. Manual hyperinflation was applied randomly, alternating the use or not of the positive end-expiratory pressure valve, followed by tracheal aspiration for ending the maneuver. For nominal data, the two-tailed Wilcoxon test was applied at the 5% significance level and 80% power.
Twenty-eight preterm newborns, with an average birth weight of 1,005.71 ± 372.16g, an average gestational age of 28.90 ± 1.79 weeks, an average corrected age of 33.26 ± 1.78 weeks, and an average mechanical ventilation time of 29.5 (15 - 53) days, were studied. Increases in inspiratory and expiratory volumes occurred between time-points A5 (before the maneuver) and C1 (immediately after tracheal aspiration) in both the maneuver with the valve (p = 0.001 and p = 0.009) and without the valve (p = 0.026 and p = 0.001), respectively. There was also an increase in expiratory resistance between time-points A5 and C1 (p = 0.044).
Lung volumes increased when performing the maneuver with and without the valve, with a significant difference in the first minute after aspiration. There was a significant difference in expiratory resistance between the time-points A5 (before the maneuver) and C1 (immediately after tracheal aspiration) in the first minute after aspiration within each maneuver.
Abstract
Revista Brasileira de Terapia Intensiva. 2015;27(3):284-292
DOI 10.5935/0103-507X.20150048
Evidence-based practices search for the best available scientific evidence to support problem solving and decision making. Because of the complexity and amount of information related to health care, the results of methodologically sound scientific papers must be integrated by performing literature reviews. Although endotracheal suctioning is the most frequently performed invasive procedure in intubated newborns in neonatal intensive care units, few Brazilian studies of good methodological quality have examined this practice, and a national consensus or standardization of this technique is lacking. Therefore, the purpose of this study was to review secondary studies on the subject to establish recommendations for endotracheal suctioning in intubated newborns and promote the adoption of best-practice concepts when conducting this procedure. An integrative literature review was performed, and the recommendations of this study are to only perform endotracheal suctioning in newborns when there are signs of tracheal secretions and to avoid routinely performing the procedure. In addition, endotracheal suctioning should be conducted by at least two people, the suctioning time should be less than 15 seconds, the negative suction pressure should be below 100 mmHg, and hyperoxygenation should not be used on a routine basis. If indicated, oxygenation is recommended with an inspired oxygen fraction value that is 10 to 20% greater than the value of the previous fraction, and it should be performed 30 to 60 seconds before, during and 1 minute after the procedure. Saline instillation should not be performed routinely, and the standards for invasive procedures must be respected.
Abstract
. ;
Abstract
Revista brasileira de terapia intensiva. 2014;26(1):51-56
DOI 10.5935/0103-507X.20140008
To identify risk factors for extubation failure and reintubation in newborn infants subjected to mechanical ventilation and to establish whether ventilation parameters and blood gas analysis behave as predictors of those outcomes.
Prospective study conducted at a neonatal intensive care unit from May to November 2011. A total of 176 infants of both genders subjected to mechanical ventilation were assessed after extubation. Extubation failure was defined as the need to resume mechanical ventilation within less than 72 hours. Reintubation was defined as the need to reintubate the infants any time after the first 72 hours.
Based on the univariate analysis, the variables gestational age <28 weeks, birth weight <1,000g and low Apgar scores were associated with extubation failure and reintubation. Based on the multivariate analysis, the variables length of mechanical ventilation (days), potential of hydrogen (pH) and partial pressure of oxygen (pO2) remained associated with extubation failure, and the five-minute Apgar score and age at extubation were associated with reintubation.
Low five-minute Apgar scores, age at extubation, length of mechanical ventilation, acid-base disorders and hyperoxia exhibited associations with the investigated outcomes of extubation failure and reintubation.
Abstract
Revista brasileira de terapia intensiva. 2014;26(3):317-320
DOI 10.5935/0103-507X.20140045
Atelectasis is a pulmonary disorder that lengthens the hospitalization time of newborns in intensive care units, resulting in increased morbidity among these infants. High-flow nasal cannulae have been used in newborns to prevent atelectasis and/or expand pulmonary regions affected by atelectasis; however, to date, no evidence-based data regarding this approach have been reported. In this paper, we report on the cases of two male newborn patients. The first and second patients described in this report were hospitalized for a neurosurgical procedure and the treatment of abdominal disease, respectively, and were subjected to invasive mechanical ventilation for 4 and 36 days, respectively. After extubation, these patients continued receiving oxygen therapy but experienced clinical and radiological worsening typical of atelectasis. In both cases, by 24 hours after the implantation of an high-flow nasal cannulae to provide noninvasive support, radiological examinations revealed the complete resolution of atelectasis. In these cases, the use of an high-flow nasal cannulae was effective in reversing atelectasis. Thus, this approach may be utilized as a supplemental noninvasive ventilatory therapy to avoid unnecessary intubation.
Abstract
Revista Brasileira de Terapia Intensiva. 2012;24(3):230-235
DOI 10.1590/S0103-507X2012000300005
OBJECTIVE: This study established the incidence and primary causes of unplanned extubation in newborns in the neonatal intensive care units of the Hospital Sofia Feldman, Belo Horizonte (Minas Gerais). METHODS: This retrospective study was conducted between July 1, 2009 and April 30, 2010. Unplanned extubations and their primary causes were assessed using an adverse events form. The following variables were assessed: gender, corrected age, present weight, duration of mechanical ventilation time, and motives/causes of the event on the day of the unplanned extubation event. RESULTS: Fifty-four unplanned extubations occurred, which corresponded to an incidence of 1.0 event/100 days of mechanical ventilation. This rate was higher among newborns with a corrected age of 30 to 36 weeks and weight < 1,000 g. The primary causes of unplanned extubations included patient agitation, inappropriate handling of patients during the performance of procedures, and inappropriate fixation and positioning of the endotracheal tube. CONCLUSION: The incidence of unplanned extubation in the investigated neonatal intensive care units was low during the study period compared to previously reported data. Nevertheless, the assessment of the quality of procedures, the continuous follow-up of newborns, and the monitoring of the causes of extubation are required to further reduce this incidence.