Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(4):571-581
DOI 10.5935/0103-507X.20190070
Descrever a adequação de duas escalas comportamentais, a Behavioral Pain Scale e a Critical Care Pain Observation Tool, para a avaliação da dor em pacientes intubados orotraquealmente, internados em unidades de terapia intensiva.
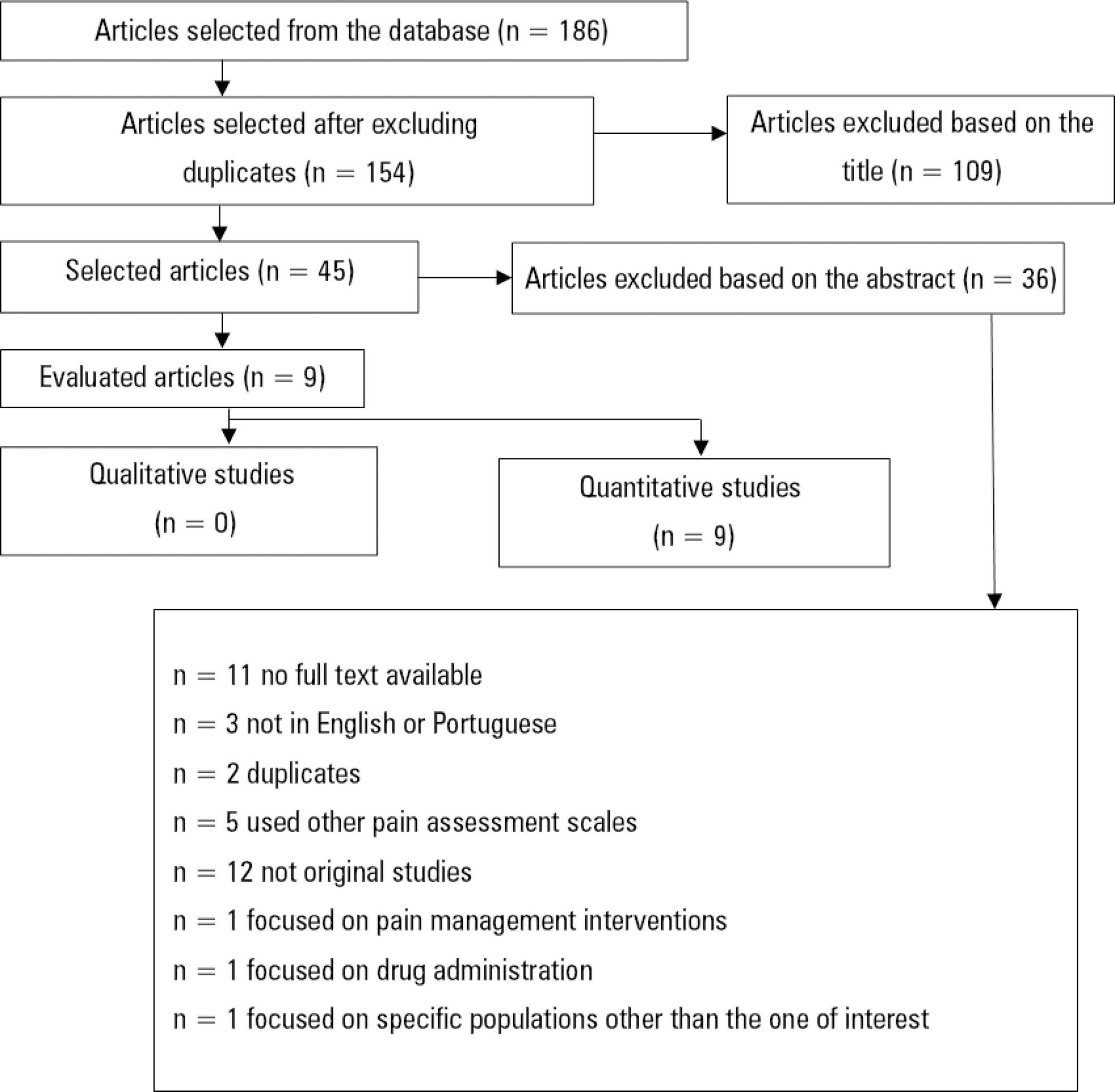
Utilizando a metodologia recomendada pelo Centro Cochrane, foi realizada revisão sistemática da literatura, na base de dados eletrônica EBSCO host (CINAHL Complete, MEDLINE®Complete, Nursing & Allied Health Collection: Comprehensive, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, Library, Information Science & Technology Abstracts, MedicLatina). Foram realizadas duas pesquisas com os seguintes termos em inglês no campo de pesquisa: "behavioral pain scale" AND "critical care pain observation tool" AND "behavioral pain scale" OR "critical care pain observation tool". Dois revisores independentes realizaram a avaliação crítica, a extração e a síntese dos dados.
Foram incluídos 15 estudos que evidenciaram que a Behavioral Pain Scale e a Critical Care Pain Observation Tool eram duas escalas válidas e confiáveis para a avaliação da dor em pacientes intubados orotraquealmente e internados em unidade de terapia intensiva. As escalas apresentaram propriedades psicométricas semelhantes, bem como boa confiabilidade.
Ambas as escalas são adequadas para a avaliação da dor em pacientes intubados orotraquealmente, internados em unidade de terapia intensiva, contudo, apresentam limitações em populações específicas como doentes vítimas de trauma, queimados e do foro neurocirurgico. É sugerida a realização de mais estudos sobre o tema e em populações específicas.
Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(4):555-560
DOI 10.5935/0103-507X.20190074
Patients with acute respiratory distress syndrome require ventilation strategies that have been shown to be important for reducing short-term mortality, such as protective ventilation and prone position ventilation. However, patients who survive have a prolonged stay in both the intensive care unit and the hospital, and they experience a reduction in overall satisfaction with life (independence, acceptance and positive outlook) as well as decreased mental health (including anxiety, depression and posttraumatic stress disorder symptoms), physical health (impaired physical state and activities of daily living; fatigue and muscle weakness), social health and the ability to participate in social activities (including relationships with friends and family, hobbies and social gatherings).
Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(3):403-409
DOI 10.5935/0103-507X.20190050
Brain death, defined as the complete and irreversible loss of brain functions, has a history that is linked to the emergence of intensive care units and the advancement of artificial ventilatory support. In Brazil, by federal law, the criteria for the diagnosis of brain death have been defined by the Federal Council of Medicine since 1997 and apply to the entire Brazilian territory. Resolution 2,173/2017 of the Federal Council of Medicine updated the criteria for diagnosing brain death. These changes include the following: the requirement for the patient to meet specific physiological prerequisites and for the physician to provide optimized care to the patient before starting the procedures for diagnosing brain death and to perform complementary tests, as well as the need for specific training for physicians who make this diagnosis. Other changes include the reduction of the time interval between the two clinical examinations, the possibility of continuing procedures in the presence of unilateral ear or eye injury, the performance of a single apnea test and the creation of a statement of brain death determination that includes the recording of all procedures in a single document. This document, despite the controversy surrounding it, increases the safety necessary when establishing a diagnosis of such importance and has positive implications that extend beyond the patient and the physician to reach the entire health system.
Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(3):368-378
DOI 10.5935/0103-507X.20190060
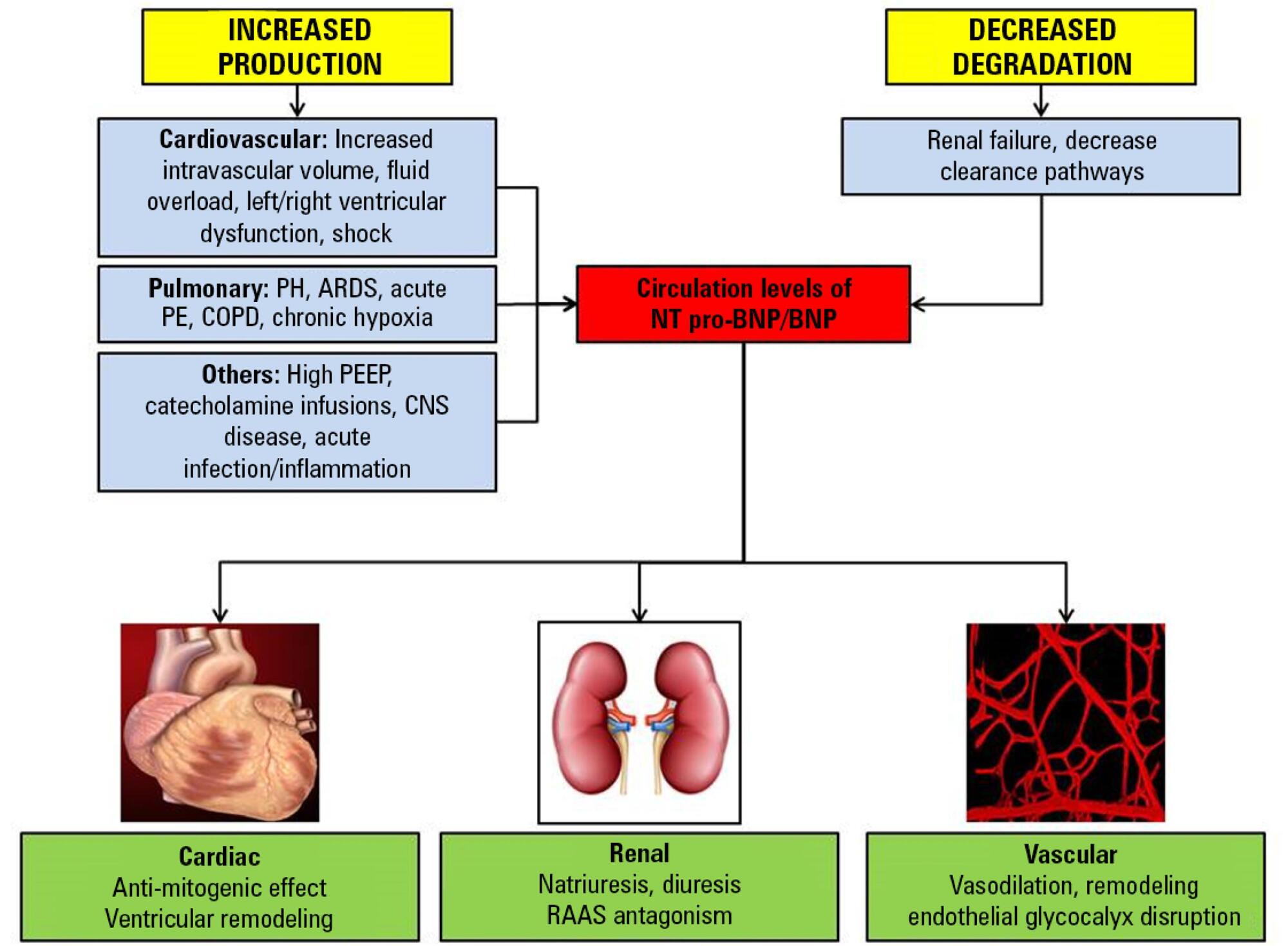
Sepsis continues to be a leading public health burden in the United States and worldwide. With the increasing use of advanced laboratory technology, there is a renewed interest in the use of biomarkers in sepsis to aid in more precise and targeted decision-making. Natriuretic peptides have been increasingly recognized to play a role outside of heart failure. They are commonly elevated among critically ill patients in the setting of cardiopulmonary dysfunction and may play a role in identifying patients with sepsis and septic shock. There are limited data on the role of these biomarkers in the diagnosis, management, outcomes and prognosis of septic patients. This review seeks to describe the role of natriuretic peptides in fluid resuscitation, diagnosis of ventricular dysfunction and outcomes and the prognosis of patients with sepsis. B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) have been noted to be associated with left ventricular systolic and diastolic and right ventricular dysfunction in patients with septic cardiomyopathy. BNP/NT-proBNP may predict fluid responsiveness, and trends of these peptides may play a role in fluid resuscitation. Despite suggestions of a correlation with mortality, the role of BNP in mortality outcomes and prognosis during sepsis needs further evaluation.
Abstract
Revista Brasileira de Terapia Intensiva. 2019;31(3):386-392
DOI 10.5935/0103-507X.20190051
The improvement in cardiopulmonary resuscitation quality has reduced the mortality of individuals treated for cardiac arrest. However, survivors have a high risk of severe brain damage in cases of return of spontaneous circulation. Data suggest that cases of cardiac arrest in critically ill patients with non-shockable rhythms have only a 6% chance of returning of spontaneous circulation, and of these, only one-third recover their autonomy. Should we, therefore, opt for a procedure in which the chance of survival is minimal and the risk of hospital death or severe and definitive brain damage is approximately 70%? Is it worth discussing patient resuscitation in cases of cardiac arrest? Would this discussion bring any benefit to the patients and their family members? Advanced discussions on do-not-resuscitate are based on the ethical principle of respect for patient autonomy, as the wishes of family members and physicians often do not match those of patients. In addition to the issue of autonomy, advanced discussions can help the medical and care team anticipate future problems and, thus, better plan patient care. Our opinion is that discussions regarding the resuscitation of critically ill patients should be performed for all patients within the first 24 to 48 hours after admission to the intensive care unit.
Abstract
Revista Brasileira de Terapia Intensiva. 2018;30(1):80-85
DOI 10.5935/0103-507X.20180014
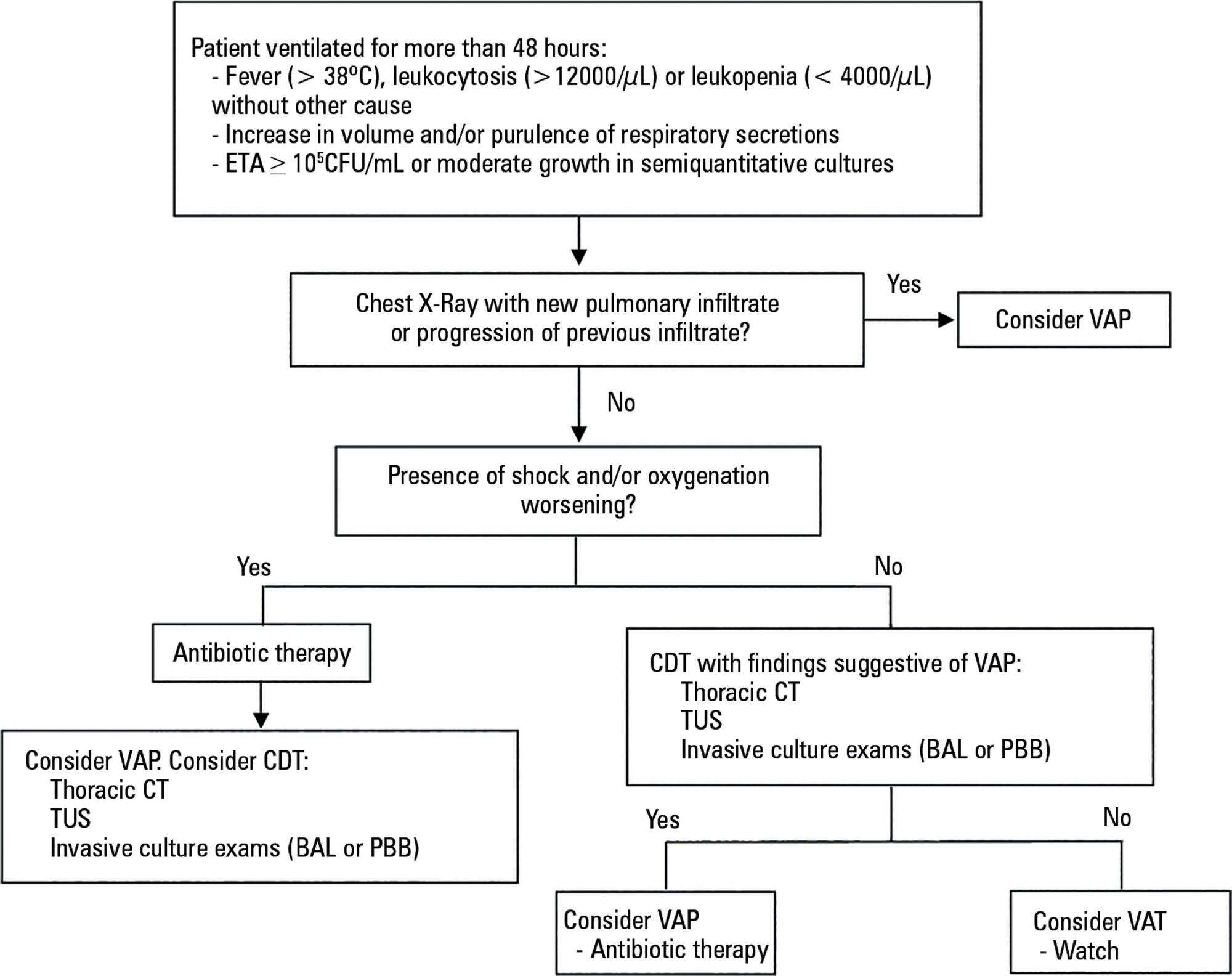
The concept of ventilator-associated tracheobronchitis is controversial; its definition is not unanimously accepted and often overlaps with ventilator-associated pneumonia. Ventilator-associated tracheobronchitis has an incidence similar to that of ventilator-associated pneumonia, with a high prevalence of isolated multiresistant agents, resulting in an increase in the time of mechanical ventilation and hospitalization but without an impact on mortality. The performance of quantitative cultures may allow better diagnostic definition of tracheobronchitis associated with mechanical ventilation, possibly avoiding the overdiagnosis of this condition. One of the major difficulties in differentiating between ventilator-associated tracheobronchitis and ventilator-associated pneumonia is the exclusion of a pulmonary infiltrate by chest radiography; thoracic computed tomography, thoracic ultrasonography, or invasive specimen collection may also be required. The institution of systemic antibiotic therapy does not improve the clinical impact of ventilator-associated tracheobronchitis, particularly in reducing time of mechanical ventilation, hospitalization or mortality, despite the possible reduced progression to ventilator-associated pneumonia. However, there are doubts regarding the methodology used. Thus, considering the high prevalence of tracheobronchitis associated with mechanical ventilation, routine treatment of this condition would result in high antibiotic usage without clear benefits. However, we suggest the institution of antibiotic therapy in patients with tracheobronchitis associated with mechanical ventilation and septic shock and/or worsening of oxygenation, and other auxiliary diagnostic tests should be simultaneously performed to exclude ventilator-associated pneumonia. This review provides a better understanding of the differentiation between tracheobronchitis associated with mechanical ventilation and pneumonia associated with mechanical ventilation, which can significantly decrease the use of antibiotics in critically ventilated patients.